Translate this page into:
Idiopathic sporadic tumoral calcinosis in an Indian girl
Correspondence Address:
G K Tharini
No. 108 Vellala Street, Purasaiwalkam, Chennai 600 084
India
| How to cite this article: Tharini G K, Prabhavathy D, Hema N, Jayakumar S. Idiopathic sporadic tumoral calcinosis in an Indian girl. Indian J Dermatol Venereol Leprol 2011;77:536 |
Sir,
Calcinosis cutis may be divided into dystrophic, metastatic, idiopathic, and iatrogenic type. Tumoral calcinosis (considered as a variant of idiopathic calcinosis) is characterized by calcium deposits in skin over large joints resembling neoplasm. It most commonly affects adolescents, although occurrences of tumoral calcinosis in all age groups ranging from infancy to old age have been reported in literature. [1] There is no sexual predilection. Tumoral calcinosis is mainly reported from Africa, but there are few case reports from India. [2],[3] We present this case for its rare occurrence.
A 13-year-old girl reported for multiple, painless, slowly progressing hard swellings over left elbow, left knee, and right ankle of 6 months duration. She had restricted joint mobility and reported discharge of chalky white material from the swelling over elbow. She had no systemic symptoms. There was no family history of trauma or administration of any medication prior to appearance of swellings. On examination, she was found to have multiple, large, firm swellings over left elbow, left knee and right ankle [Figure - 1], [Figure - 2] and [Figure - 3]. The swelling over left elbow was studded with white papules and extruding white material. The material was sent for biochemical analysis and found to be calcium. Radiological examination of swellings revealed soft tissue calcification [Figure - 4]. Her serum calcium, phosphate, and alkaline phosphatase levels were normal. Screening tests for collagen vascular disease and hormonal assay revealed normal results. Laboratory tests showed normal blood count and renal function. Histopathological examination revealed basophilic granular calcium deposits within cystic spaces in epidermis and dermis, surrounded by inflammatory infiltrate and few giant cells [Figure - 5]. von Kossa stain confirmed the diagnosis [Figure - 6]. Based on all these findings a diagnosis of idiopathic sporadic (primary normophosphatemic) tumoral calcinosis was made. Surgical excisions were done along with aluminium hydroxide 300 mg (antacid) two tablets three times daily for 3 months. During the follow-up period of 3 months there was no recurrence.
 |
| Figure 1: Photograph of the patient showing swelling over right ankle with few nodules on surface |
 |
| Figure 2: Swelling over the left knee. |
 |
| Figure 3: Swelling over the left elbow studded with white papules and surface ulceration. |
 |
| Figure 4: Radiograph of knee showing soft tissue calcification. |
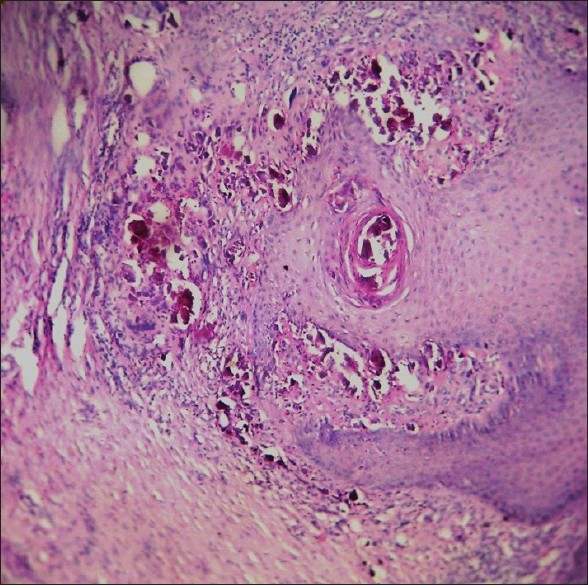 |
| Figure 5: Histopathology showing acanthosis, basophilic calcium granules in epidermis (transepidermal elimination) and dermis within cystic spaces, surrounded by inflammatory infiltrate (H and E, ×200) |
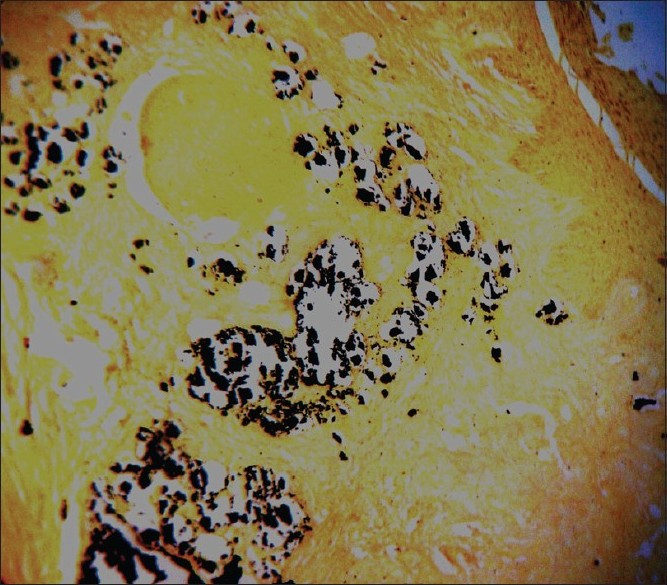 |
| Figure 6: Micrograph showing calcium granules that are stained black (von Kossa, ×200) |
The term tumoral calcinosis (synonym: Teutschländer disease) was coined by Inclan in 1943. Tumoral calcinosis is a morphological diagnosis and it can occur in a variety of clinical settings: primary normophosphatemic, primary hyperphosphatemic, and secondary tumoral calcinosis occurring along with disorders that are capable of producing soft tissue calcification. [2] Tumoral calcinosis often occurs in association with conditions such as chronic renal failure, hyperparathyroidism, and milk alkali syndrome. The underlying defect in hyperphosphatemic familial tumoral calcinosis, an autosomal recessive disorder, might be mutations in any one of the following three genes; fibroblast growth factor gene, KL and GALTN3 gene. [4] Defective function of any one of these three proteins results in hyperphosphatemic tumoral calcinosis with enhanced renal phosphate reabsorption. Elevated levels of serum 1,25-dihydroxyvitamin D are observed, while serum calcium and parathormone levels are normal.
Tumoral calcinosis is a benign disorder that develops gradually. Patients usually present with asymptomatic, single or multiple, unilateral or bilateral, firm swellings over hip, shoulder, elbow, and knee joints. [2],[3] Rarely wrist, hands, ankle, scalp, eyelid, and feet are involved. [5] Nodules may ulcerate and extrude chalky white material. Complications include pain due to nerve compression, ulceration, bacterial infection, cosmetic disfigurement, and restricted joint mobility. Severe complications are uncommon.
Patients with idiopathic sporadic tumoral calcinosis have normal mineral levels without underlying disease. There are many case reports of idiopathic sporadic tumoral calcinosis, similar to the present one. [2],[3],[5] Hammoud et al., [1] have reported that, in almost all infantile cases they have studied, tumoral calcinosis manifested without any predisposing factors, such as a family history.
The etiology of tumoral calcinosis remains unknown. The presence of lesions around pressure points suggests the possibility of local trauma as a causative factor. Histologically there is collagen necrobiosis initially, which results in aggregates of densely calcified material.
Tumoral calcinosis can be mistaken for mycetoma, osteosarcoma, and chondrosarcoma. Investigations include serum mineral levels, renal function tests, complete blood count, autoantibodies, hormonal assay, X-ray, bone scintigraphy, CT scan, MRI, FNAC, chemical analysis, microspectroscopic study of deposit and skin biopsy.
Skin biopsy reveals calcium deposits as basophilic granules within dermis or as massive deposits in subcutis. They occur within cystic spaces, surrounded by histiocytes and foreign body giant cells. Ultrastructural studies demonstrate that crystals are both extracellular and within mononuclear cells. von Kossa (stains black) and alizarin red stain are confirmatory.
Surgical excision is the preferred method of treatment. Incomplete excision can result in recurrences. Recurrence in sporadic cases is rare although it can occur in patients with genetic anomalies or secondary cases, as the underlying disorder persists. Calcium channel blocker diltiazem and bisphosphonates are reported to be effective in idiopathic sporadic tumoral calcinosis. [3] Antacids, sevelamer (phosphate-binders) and acetazolamide are found useful in hyperphosphatemic cases. [4]
| 1. |
Hammoud S, McCarthy EF, Weber K. Tumoral calcinosis in infants: A report of three cases and review of the literature. Clin Orthop Relat Res 2005;436:261-4.
[Google Scholar]
|
| 2. |
Datta C, Bandyopadhyay D, Battacharyya S, Ghosh S. Tumoral calcinosis. Indian J Dermatol Venereol Leprol 2005;71:293-4.
[Google Scholar]
|
| 3. |
Jacob JJ, Mathew K, Thomas N. Idiopathic sporadic tumoral calcinosis of the hip: Successful oral bisphosphonate therapy. Endocr Pract 2007;13:182-6.
[Google Scholar]
|
| 4. |
Lammoglia JJ, Mericq V. Familial tumoral calcinosis caused by a novel FGF23 mutation: Response to induction of tubular renal acidosis with acetazolamide and the non-calcium phosphate binder sevelamer. Horm Res 2009;71:178-84.
[Google Scholar]
|
| 5. |
Mohamed S, Jong-Hun J, Weon-Yoo K. Tumoral calcinosis of the foot with unusual presentation in an 11-year-old boy: A case report and review of literature. J Postgrad Med 2007;53:247-9.
[Google Scholar]
|
Fulltext Views
1,775
PDF downloads
2,287





