Translate this page into:
IgA Vasculitis in adults: Importance of recognising diverse cutaneous and systemic manifestations and associations
Corresponding author: Dr. Anuradha Bishnoi, Department of Dermatology, Venereology and Leprology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. dranha14@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh S, Bishnoi A, Hemalatha M, Mehta H, Meena A, Keshavamurthy V, et al. IgA Vasculitis in adults: Importance of recognising diverse cutaneous and systemic manifestations and associations. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_518_2024
Dear Editor,
IgA vasculitis (IgAV) refers to IgA1 immune complex-mediated inflammation of cutaneous, renal, and gastrointestinal (GIT) microvasculature. Recognised primarily in children as Henoch Schonlein Purpura/ anaphylactoid purpura; it presents with a tetrad of palpable purpura, arthritis, haematuria, and abdominal pain. The adult counterpart is less well characterised with an incidence of 1.3-1.4/1,00,000/year.1 It can be triggered by upper respiratory infections, vaccinations, and drugs like ampicillin, quinine, and infliximab.2
It is imperative for dermatologists to acknowledge this condition, as they have a heightened risk of developing end-stage kidney disease (ESKD) compared to children who experience self-limiting trajectory..2,3 A one-year retrospective record review was conducted on patients over 18-years of age diagnosed with IgAV based on European league against rheumatism (EULAR) criteria [Table 1].4
| Criteria | Definition |
|---|---|
| 1. Purpura | Palpable purpura, often in crops over-dependent areas, non-thrombocytopenic |
| 2. Gastrointestinal (GIT)# | Abdominal pain (acute onset, colicky), other features include GIT bleeding and intussusception |
| 3. Biopsy (Either Skin or renal) | Leukocytoclastic vasculitis/ proliferative glomerulonephritis AND predominant mesangial IgA deposition |
| 4. Joint | Acute onset arthritis (swelling, pain, restriction of motion) or arthralgia (pain) |
| 5. Renal |
Proteinuria >0.3gm/day Hematuria (>5 red blood cells/high power field or red cell casts) |
Atypical- refers to non-dependent areas and lesions above the waist
# Only GIT symptoms are required for diagnosis of GIT involvement. Biopsy showing vasculitis or the presence of IgA deposits is not defined in the criteria for GI involvement.
A total of six cases were reviewed for clinical and investigation details [Table 2]. Their mean age was 28 years with a male-to-female ratio of 5:1. All patients had cutaneous onset with joint involvement in 4 patients; GIT and renal involvement were present in 3 patients.
| Case | Age/Sex | Organ involvement | Skin lesions | Biopsy and investigations | Treatment* | Outcome# | Recurrence |
|---|---|---|---|---|---|---|---|
| 1 | 33/M | Skin-Joints-Renal | Palpable purpura, targetoid lesions over elbows and lower limbs | LCV in dermal capillaries along with granular IgA deposits on DIF | Prednisolone* and Dapsone |
Skin lesions and joint complaints resolved in 3 weeks Renal parameters normalised by 1 month |
No |
| 2 | 35/F | Skin-Joints-GIT |
Purpuric lesions, hemorrhagic necrotic and pustular lesions over both upper and lower extremities and trunk Erosions over tongue |
LCV in dermal capillaries, IgA, IgM, C3 deposition on DIF |
Prednisolone and cyclosporine Initially managed with Dapsone, which was stopped due to development of DRESS |
Lesions healed in 2 months GIT symptoms and joint complaints resolved in 2 weeks |
No, maintained on treatment |
| 3 | 22/M | Skin-GIT |
Palpable purpura over upper and lower limbs, urticated papules over the trunk. Gingival hypertrophy with sterile pustules over dental apices |
LCV in dermal blood vessels, DIF-granular IgA and IgM deposition CT abdomen revealed circumferential thickening of jejunum and ileum, colonoscopy revealed ileal erosions and nodularity with dense infiltrate without any granulomas. |
Prednisolone and Dapsone | Skin lesions and GIT complaints initially resolved in 3 weeks |
Yes (cutaneous relapse) at 3 months, managed with prednisolone and dapsone. Treatment stopped after one year after a symptom-free period of 6 months. |
| 4 | 25/M | Skin-Joints-GIT | Palpable purpura, urticated papules over lower and upper limbs | LCV in upper dermal capillaries, IgA granular deposits on DIF | Prednisolone and Dapsone |
Lesions cleared by one month Joint and GIT complaints resolved by 1 month |
No |
| 5 | 25/M | Skin-Joints-Renal | Purpuric, hemorrhagic, and necrotic lesions over both upper and lower extremities | Lymphocytic infiltrate with LCV, IgA 3+ positivity in dermal capillaries on DIF |
Prednisolone, telmisartan, furosemide |
Skin lesions resolved without treatment, Improvement in frothuria and proteinuria | No |
| 6 | 29/M | Skin-Renal | Purpuric lesions over legs | LCV with IgA 2+ positivity in dermal capillaries |
Prednisolone, telmisartan, furosemide |
Skin lesions resolved within 14 days of therapy. Improvement in frothuria noticed over 2 months | No, maintained on treatment |
LCV-Leukocytoclastic vasculitis, DIF-Direct immunofluorescence, CT-Computed Tomography, DRESS- Drug reaction with eosinophilia and systemic symptoms, GIT- Gastrointestinal involvement
#ANA: Antinuclear antibodies, ANCA: antineutrophilic cytoplasmic antibodies, CXR: chest radiographs, Antibodies for HIV, hepatitis B and Hepatitis C, protein electrophoresis were normal in all patients.
#All patients were followed up with urine analysis every 2 monthly in those without renal involvement, and monthly at every visit for those with renal involvement.
Adult-onset IgAV has cutaneous manifestations in 75% cases, mainly asymmetrical palpable purpura involving gravity-dependent areas, sometimes extending to the upper limbs and trunk. It presents with diverse morphologies, including bullous, ulcerative, pustular, hemorrhagic purpura, and urticated papules.5 All our cases had cutaneous onset with extensive purpuric lesions on extremities with targetoid lesions [Figure 1a–1c]. Mucosal involvement was observed in two patients (oral erosions, sterile gingival pustules).

- Presence of typical purpuric lesions and erythema multiforme-like targetoid lesions (white arrow) over both legs in case 1.

- Purpuric macules and papules over both lower limbs (white circle), dusky hemorrhagic lesions (white star), and necrotic lesions (white square) in case 2.

- Healing of necrotic lesions with scarring and dyspigmentation in patient 2 after 3 months of cyclosporine (inset shows the presence of necrotic lesion at onset).
The diagnosis of IgAV requires either skin or renal biopsy for evidence of LCV (leukocytoclastic vasculitis).4 Skin biopsy shows LCV in postcapillary venules along with IgA and C3 deposition with a sensitivity of 81%, specificity of 83-85%, and positive and negative predictive values of 81% and 84%, respectively [Figure 2a–2b].5 In a study, IgAV was the commonest diagnosis (31%) among 198 analysed cases of cutaneous small-vessel-vasculitis; clinical diagnosis of IgAV could be confirmed in 61.5% cases by direct immunofluorescence (DIF), and in remaining unsuspected cases, diagnosis of IgAV was based solely on DIF findings.6
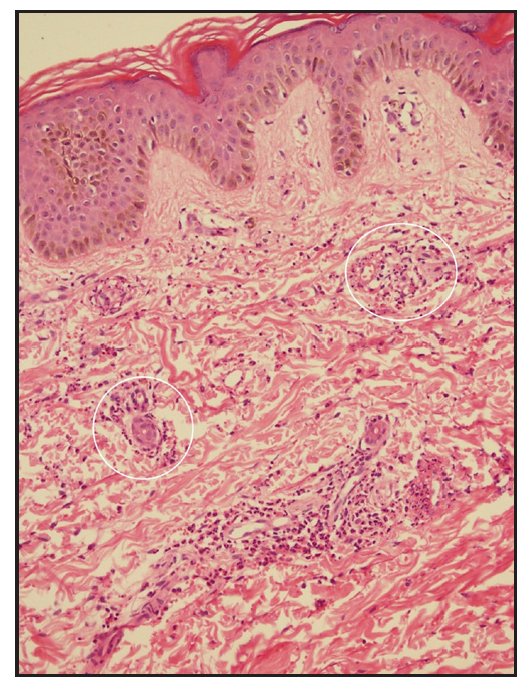
- Skin biopsy in patient 3 showing dermal oedema, red cell extravasation, endothelial swelling, and leukocytoclasia (white circle, Haematoxylin and eosin, 200x).
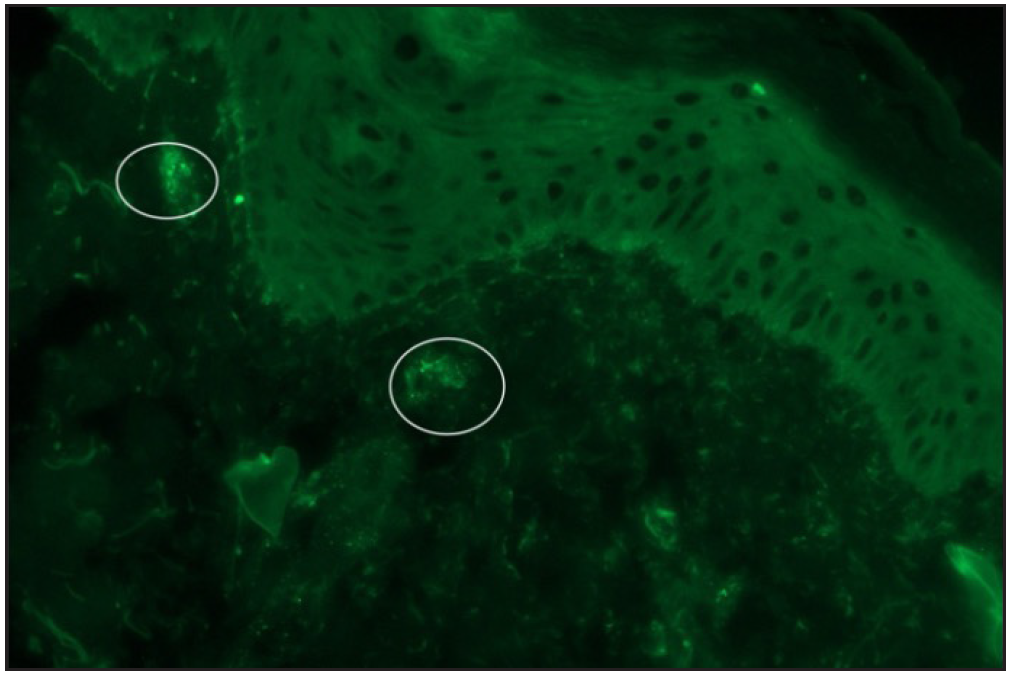
- Direct immunofluorescence of skin biopsy of patient 2 showing granular immunoglobulin A deposits around dermal vessels.
Regarding extracutaneous manifestations, an Asian cohort demonstrated renal involvement in 56%, joint and GIT involvement in 31% each.7 Joint involvement is transient, oligoarticular, and non-deforming, affecting large joints of lower limbs. GIT involvement includes abdominal pain, intestinal bleeding, diarrhoea, and acute abdomen. Rarely associated with Crohn’s disease, IgAV usually presents with mucosal erythema or ulcerations in the duodenum/ileum, sometimes manifesting as isolated terminal ileitis (patient 3). Crohn’s disease, on the other hand, presents with fissures, small bowel strictures, transmural inflammation, and non-caseating granulomas.
Renal involvement in IgAV presents with severe proteinuria, haematuria, or renal failure.3,5 Risk factors include female gender, older age of onset, haemorrhagic lesions above the waistline, GIT symptoms, relapses, leukocytosis, and low C3 levels.2,3,5 Non-invasive biomarkers like neutrophil-lymphocyte ratio, urinary IgA, and interleukins-6, 8 can predict renal involvement.8 The presence of additional IgM and C3 deposits in the skin may predict renal and joint involvement, respectively.8
Renal biopsy is reserved for persistent proteinuria, nephrotic or nephritic syndrome, and renal failure. It helps to differentiate from other pathologies and is not meant for initial diagnosis. Skin biopsy and DIF are recommended by EULAR for use in initial diagnosis.4,8
IgAV should be differentiated from IgA nephropathy (IgAN), a renal-limited form, mandating renal biopsy, presenting with macroscopic hematuria and often being diagnosed at ESKD. Skin biopsy in IgAV may rarely show IgA deposits, which are considered non-diagnostic and lack sensitivity as a diagnostic tool.
Treatment is recommended for all adults due to a higher risk of severe renal disease (35-69%) compared to children (5-20%). Non-steroidal-anti-inflammatory drugs should be avoided due to the risk of renal disease and GIT bleeding.5 Management of skin-limited IgAV involves rest, leg elevation, low-dose prednisolone, and colchicine in patients without GIT symptoms.5 In non-responsive cases, dapsone or azathioprine can be added. For joint involvement, oral acetaminophen is advocated along with steroids in severe disease.
For renal disease, angiotensin-receptor blockers targeting 24-hr urine protein <1 gm, and blood pressure <130/80 mm Hg are recommended with limited use of immunosuppressants for persistent proteinuria. Elderly adults have unfavourable prognosis, with 7-fold mortality, often due to associated solid organ or hematological malignancy.3 Relapse (in 15%) is associated with early onset, joint involvement, and lack of immunomodulatory treatment; it is most often a cutaneous relapse, as observed in patient 3 in our series. Long-term follow-up with symptom screening, urine analysis, and serum creatinine fortnightly for 1 month followed by 2 monthly for 1 year is prudent.
To conclude, adult IgAV needs extensive literature contributions from diverse medical specialties and geographical regions for more information to optimise management strategies. Adults can present with diverse and extensive cutaneous lesions above the waistline. Additionally, patients have an increased propensity for renal and GIT involvement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Update from medicine: Henoch–Scho€nlein purpura nephritis. Int J Dermatol. 2003;42:170-7.
- [CrossRef] [PubMed] [Google Scholar]
- A Review of IgA Vasculitis (Henoch-Schönlein Purpura) Past, Present, and Future. Med Sci Monit. 2024;30:e943912.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical characteristics of biopsy-proven IgA vasculitis in children and adults: A retrospective cohort study. Mayo Clin Proc. 2019;94:1769-80.
- [CrossRef] [PubMed] [Google Scholar]
- Applicability of the 2006 European League against Rheumatism (EULAR) criteria for the classification of Henoch-Schönlein purpura. An analysis based on 766 patients with cutaneous vasculitis. Clin Exp Rheumatol. 2015;33:S-44–7.
- [Google Scholar]
- IgA Vasculitis in adults: A rare yet challenging disease. Curr Rheumatol Rep. 2021;23:50.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Role of Direct Immunofluorescence in cutaneous small-vessel vasculitis: Experience from a tertiary center. Am J Dermatopathol. 2018;40:661-6.
- [CrossRef] [PubMed] [Google Scholar]
- The profile of adult onset Henoch-Schönlein purpura in an Asian population. Int J Dermatol. 2015;54:1236-41.
- [CrossRef] [PubMed] [Google Scholar]
- Could serum pentraxin 3 levels and IgM deposition in skin biopsies predict subsequent renal involvement in children with Henoch-Schönlein purpura? Pediatr Nephrol. 2015;30:969-74.
- [CrossRef] [PubMed] [Google Scholar]






