Translate this page into:
Incidental finding of skin deposits of corticosteroids without associated granulomatous inflammation: Report of three cases
Correspondence Address:
Rajiv Joshi
14 Jay Mahal, A Road, Churchgate, Mumbai - 400 020
India
| How to cite this article: Joshi R. Incidental finding of skin deposits of corticosteroids without associated granulomatous inflammation: Report of three cases. Indian J Dermatol Venereol Leprol 2008;74:44-46 |
Abstract
Three cases are described in whom deposits of depot steroids were seen in skin biopsies done for diagnostic purposes. In the first case the skin lesion was clinically suspected to be due to the steroid injected more than a year ago and a diagnosis of pseudo-morphea due to steroid injection was made by the clinician. The other cases had clinical diagnoses of dermatofibroma and morphea with no clinical suspicion of previous steroid injection. The steroid deposits were present in the subcutaneous fat in all three cases. Histologically the findings were distinctive with collections of acellular, amorphous, fuzzy basophilic material surrounded by lipophages and disrupted adipocytes (in Case 2) and without any significant inflammatory infiltrate or granulomatous reaction (in Cases 1 and 3). The absence of inflammatory and granulomatous responses were the findings at variance with the cases described earlier in the literature.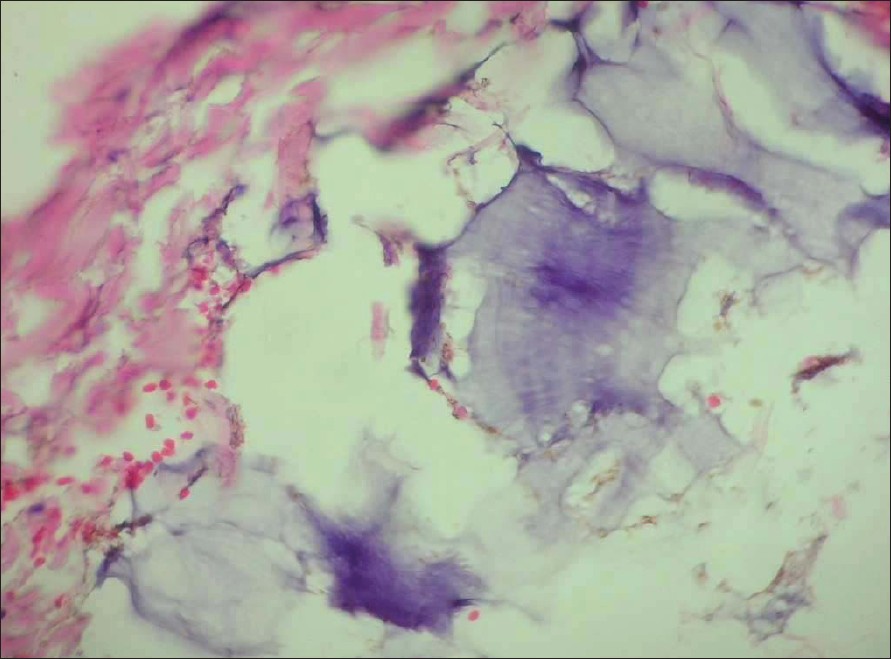 |
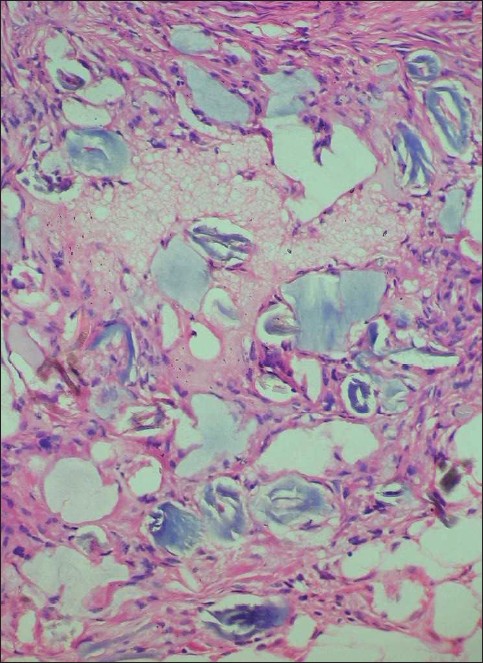
| Figure 4: Blue-gray deposits of steroids without any surrounding inflammation in Case 3 (H and E, X400) |
 |
| Figure 4: Blue-gray deposits of steroids without any surrounding inflammation in Case 3 (H and E, X400) |
 |
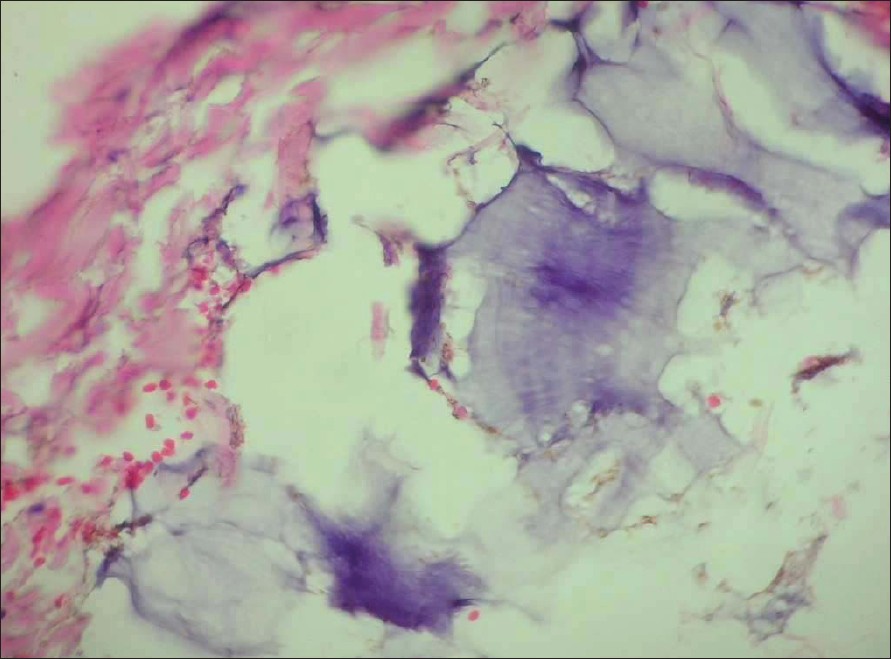
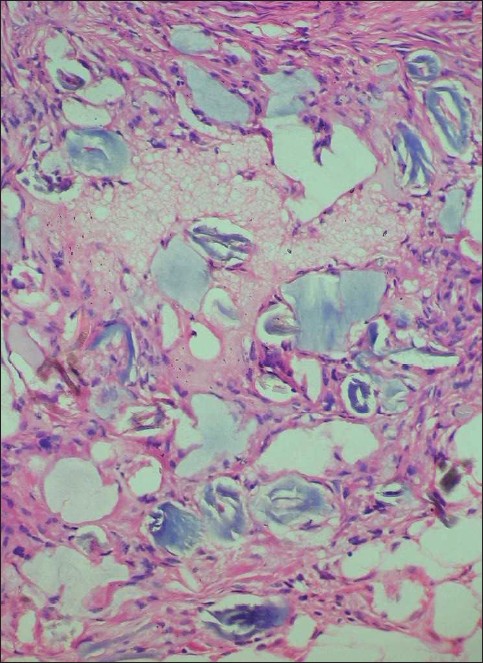
| Figure 3: Deposits of steroids seen in a sleeve of adipose tissue in Case 3 (H and E, X400) |
 |
| Figure 3: Deposits of steroids seen in a sleeve of adipose tissue in Case 3 (H and E, X400) |
 |
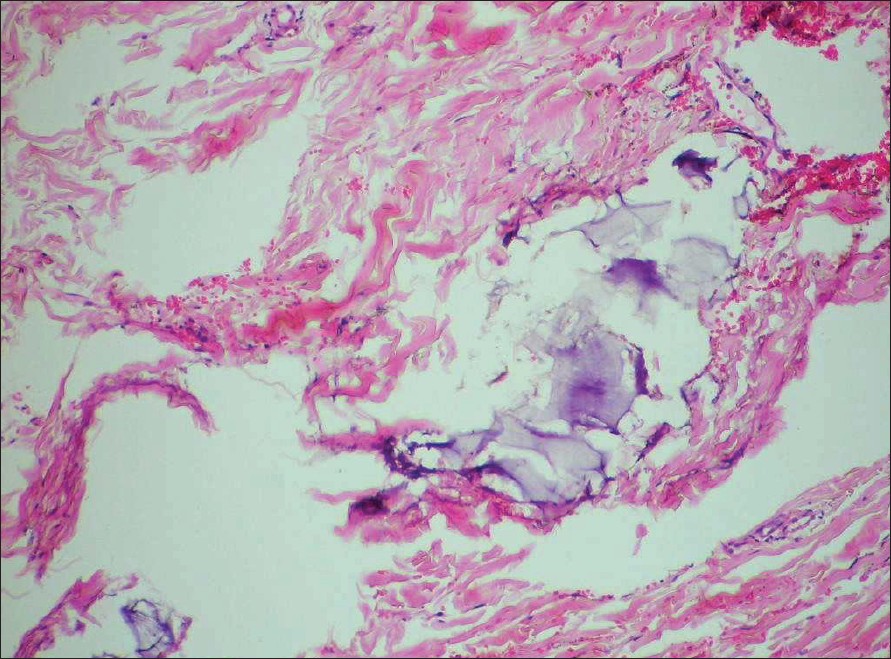
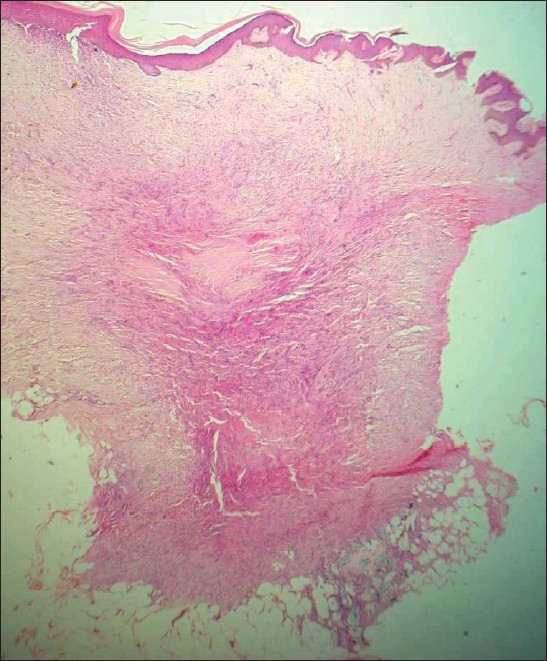
| Figure 2: Bluish deposits of steroids in the subcutis beneath the dermatofibroma surrounded by abundant extracellular lipids in Case 2 (H and E, X200) |
 |
| Figure 2: Bluish deposits of steroids in the subcutis beneath the dermatofibroma surrounded by abundant extracellular lipids in Case 2 (H and E, X200) |
 |
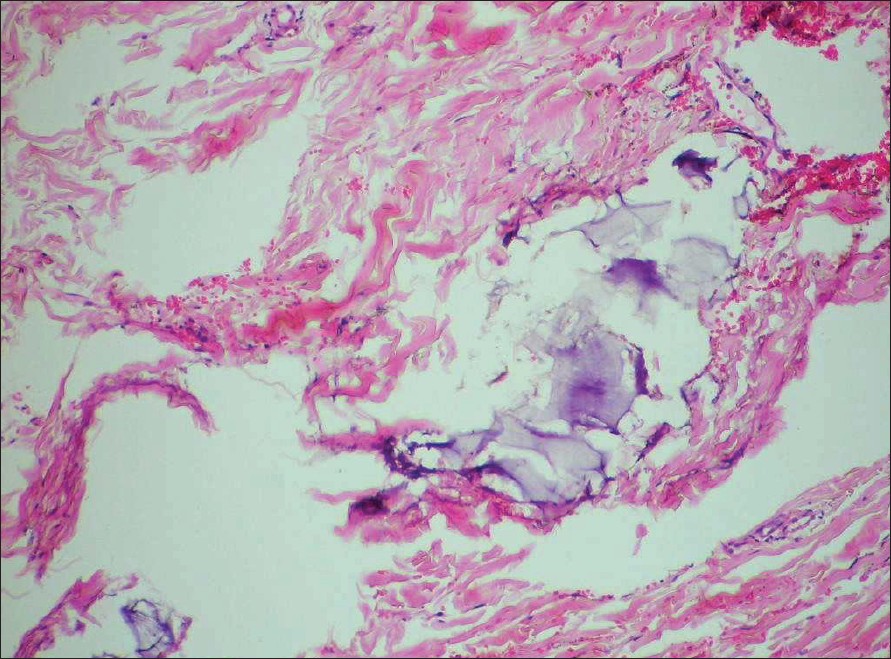
| Figure 1: Dermatofibroma with deposits of steroids in the subcutis in the right lower part of the sections in Case 2. (H and E, X40) |
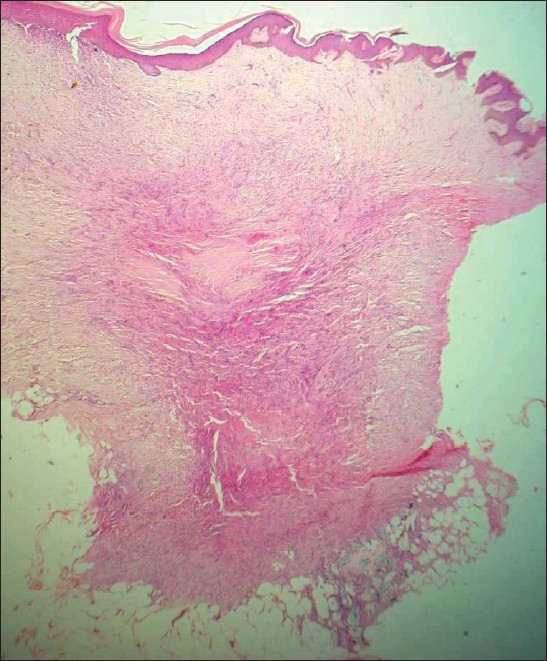 |
| Figure 1: Dermatofibroma with deposits of steroids in the subcutis in the right lower part of the sections in Case 2. (H and E, X40) |
Introduction
Intralesional steroids (usually triamcinolone acetonide) are commonly used by dermatologists for the treatment of various dermatological conditions including keloids and hypertrophic scars, chronic lichenified eczemas and stubborn patches of alopecia areata etc. Side-effects can be minimized with the judicious use of intradermal depot preparations of steroids in optimal concentration. However, cutaneous side-effects do occur and include depigmentation, atrophy and pseudo-morphea-like changes. [1] The intradermally injected steroid can remain in the skin for variable periods of time and may be seen as an incidental histological finding when that site is biopsied in future.
A variety of histological changes induced by intradermally injected steroids have been described. [2],[3],[4],[5],[6] The steroid preparation itself is seen either in the dermis or subcutis as acellular, basophilic, mucin-like material and may be mistaken for focal cutaneous mucinosis. [2],[4] The bluish amorphous material is usually surrounded by an inflammatory infiltrate containing lymphocytes, histiocytes and foreign body type of giant cells. [3] A florid granulomatous response may be observed around the pools of mucin-like material and may resemble changes seen in a rheumatoid nodule. [2],[3] Angulated empty spaces may be seen within the bluish material and probably represent corticosteroid crystals that dissolved during tissue processing. [3]
The bluish amorphous deposits of steroid need to be differentiated from focal cutaneous mucinosis, gouty tophi, pseudogout and myxoma. [6] Unlike mucin the steroid deposits do not take up the stains normally used to demonstrate mucin. Cutaneous deposits of urate crystals in gout look very similar to depot steroid but are invariably surrounded by palisades of histiocytes.
Case Reports
Case 1
The first case was a 38-year-old woman who presented with a persistent hypopigmented, mildly atrophic patch of about 4 cm x 3 cm on the upper back of several months duration. The lesion was asymptomatic but had been gradually increasing in size. There was a history of a single intradermal injection of corticosteroid at the site more than a year ago for a persistent pruritic lesion that cleared after the intradermal injection. A few months after the injection, she noticed the development of hypopigmentation at the site, which had progressively increased. There was no loss of sensation over the lesion. The clinical diagnoses considered were lichen sclerosus et atrophicus and because of the history of previous intralesional steroid injection, pseudo-morphea following intradermal steroid injection.
A skin biopsy from the lesion showed an atrophic epidermis with diminished melanin in the basal layer. The entire dermis, both papillary and reticular was thickened and showed altered collagen that was fuzzy and bedraggled in appearance with indistinct appearance of individual collagen bundles. In the subcutaneous fat were seen deposits of basophilic amorphous material surrounded by lipophages. Based on the history of previous intralesional steroid injection at the site and the presence of steroid deposits in the subcutaneous fat a diagnosis of pseudo-morphea following intralesional steroid injection was made.
Case 2
Case 2 was a 28-year-old woman who had a slowly growing pigmented firm to hard nodule near the left cubital fossa which was biopsied for histologic diagnosis. The biopsy showed features of a dermatofibroma, but in addition showed several smooth-bordered pale blue amorphous and acellular deposits of depot steroid surrounded by a few histiocytes and abundant extracellular lipid deposits [Figure - 1],[Figure - 2]. On inquiry she admitted to having received a steroid injection in the lesion several months previously.
Case 3
Case 3, a young male was biopsied for suspected morphea. The biopsy taken from the arm, had features suggestive of morphea, namely thickened and mildly sclerotic collagen throughout the dermis and a sparse to moderately dense perivascular and interstitially scattered lymphoplasmacytic infiltrate. The epidermis was flattened with prominent melanin in the basal layer. Seen additionally, within a sleeve of subcutaneous fat were collections of blue gray fuzzy material without any surrounding inflammation [Figure - 3],[Figure - 4]. The biopsy was reported as consistent with morphea with subcutaneous steroid deposits. On inquiry, the patient gave a history of being treated for the same lesion by intralesional steroid injection about six months ago.
Discussion
Depot steroid preparations, usually triamcinolone acetonide may remain in the skin for prolonged periods of time, even over a year as was seen in our first case. The persistence of the steroid may depend on factors like solubility, concentration of steroid and the development of an inflammatory response. Some authors have suggested that the foreign body type of granulomatous reaction is time-dependent and that with the passage of time the injected steroid either diffuses or is absorbed into the circulation without any tissue reaction, but small amounts may remain behind in the skin and then act as a foreign body to evoke a granulomatous reaction. [5] Pseudo-morphea-like changes have been described at sites of intradermally injected corticosteroids [1] and our first case fits into that category.
All references on skin deposits of corticosteroids refer to the inflammatory response, often granulomatous, that surrounds corticosteroid deposits. No reference was found that mentions the absence of inflammatory response and this report is to the best of our knowledge, the first report that skin deposits of corticosteroid do not as a rule induce a granulomatous response. Most prior reports relate to keloids and hypertrophic scars and it is possible that the trauma of injection or the fibrosing inflammation that led to the formation of keloids and scars itself could lead to the changes described and not the mere presence of steroid itself. Case 2 in our report had fibrosing dermatitis, namely a dermatofibroma and it did show a mild histiocytic response. The other two patients had no inflammatory response at all.
All cases with granulomatous changes reported in the past were probably biopsied because of clinical changes noticed at the injection sites which could have been induced by the granulomatous inflammation, unlike our cases which were biopsied for confirming diagnoses of suspected clinical diagnoses, namely dermatofibroma, morphea and in Case 1 to differentiate between lichen sclerosus and pseudo-morphea and the finding of corticosteroid deposits in our cases was incidental.
Thousands of patients all over the world receive intralesional steroids but almost no patient undergoes a biopsy of that site thereafter. Only those patients are biopsied who develop signs of inflammation and probably some of these are published giving rise to the assumption that deposits of corticosteroids in the skin are always associated with granulomatous inflammation. It is likely a matter of clinical bias that only patients with abnormal reactions are biopsied and it is a matter of conjecture that if one were to biopsy all sites of intralesional steroids injections, the majority would, like in our cases, not show any inflammatory changes at all! Logically the anti-inflammatory effects of the steroids should mitigate such inflammation and it is most probable that the previous inflammatory condition (scar or keloid) contributes to the granulomatous inflammation. Therefore, in conclusion, an inflammatory response does not appear to be the rule in dermal deposits of steroids.
| 1. |
Holt PJ, Marks R, Waddington E. 'Pseudomorphea': A side effect of subcutaneous corticosteroid injection. Br J Dermatol 1975;92:689-91.
[Google Scholar]
|
| 2. |
Weedon D, Gutteridge BH, Hockly RG, Emmet AJ. Unusual cutaneous reactions to injections of corticosteroids. Am J Dermatopathol 1982;4:199-203.
[Google Scholar]
|
| 3. |
Balogh K. The histologic appearance of corticosteroid injection sites. Arch Pathol Lab Med 1986;110:1168-72.
[Google Scholar]
|
| 4. |
Santa Cruz DJ, Ulbright TM. Mucin like changes in keloids. Am J Clin Pathol 1981;75:18-22.
[Google Scholar]
|
| 5. |
Bhawan J. Steroid induced 'granulomas' in hypertrophic scar. Acta Derm Venereol (Stockh) 1983;63:560-3.
[Google Scholar]
|
| 6. |
Kaur S, Amanjeet, Thami GP, Mohan H. Intralesional steroid induced histological changes in the skin. Indian J Dermatol Venereol Leprol 2003;69:232-4.
[Google Scholar]
|
Fulltext Views
3,858
PDF downloads
2,358





