Translate this page into:
Keratotic papules on the margins of palms
Correspondence Address:
Nina A Madnani
Department of Dermatology, P. D. Hinduja Hospital and MRC, Mumbai - 400 016
India
| How to cite this article: Madnani NA, Khan KJ. Keratotic papules on the margins of palms. Indian J Dermatol Venereol Leprol 2011;77:249-250 |
A 38-year-old male farmer presented with rough palms since the last 5 years. His lesions were asymptomatic but cosmetically unappealing. He had been performing heavy manual labor since the past 25 years and had no history of hyperhidrosis or any systemic complaints. There was no family history of similar complaints.
On clinical examination, he had crateriform keratotic papules arranged in a single longitudinal band, 1 cm wide, along the medial and lateral margins of palms [[Figure - 1]a and b]. The dorsal surface of the hands and feet and both soles were completely spared. Hair, teeth, nails, mucous membranes, and systemic examination were normal. Hematological investigations were within the normal range. A punch biopsy from a keratotic papule was done. The histopathological features from the hematoxylin and eosin-stained (H&E) tissue section are shown in [[Figure - 2]a], while those of Verhoeff′s Van Gieson (VVG)-stained section are shown in [[Figure - 2]b].
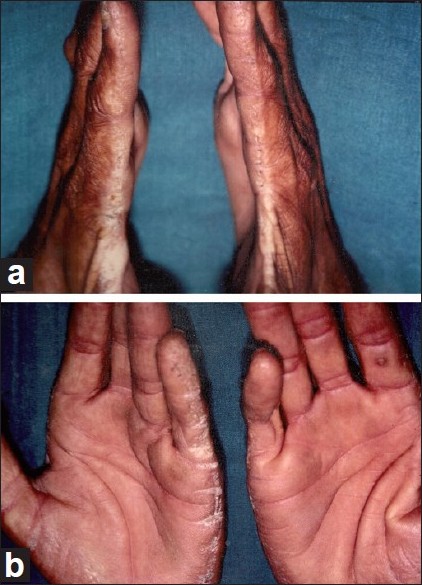 |
| Figure 1: (a,b) Keratotic papules forming a linear band along the medial margins of the palm, extending laterally onto the thenar eminences |
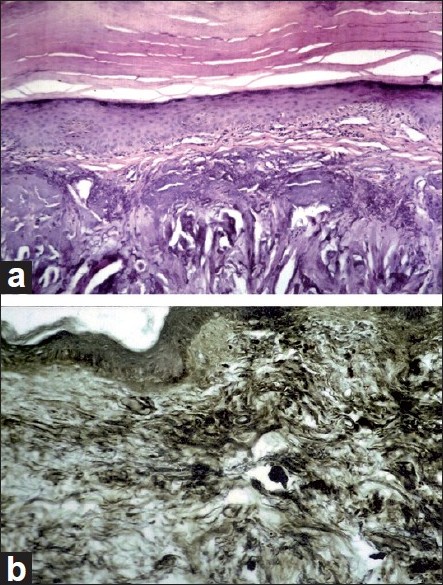 |
| Figure 2: (a) Histopathology showing gross orthokeratotic hyperkeratosis and hypergranulosis in the epidermis. Reticular dermis shows basophilic, thick curled elastic fibers and dilated capillaries (H and E, ×100). (b) Verhoeff van Giesson stain reveals thick, curled, fragmented elastic fibers in the reticular dermis (×100) |
What′s your Diagnosis?
Answer: Acrokeratoelastoidosis of Costa
Several similar entities, often share a common clinical finding of keratotic papules, usually crateriform, along the borders of the hands and feet. These conditions include acrokeratoelastoidosis of costa, focal acral hyperkeratosis, degenerative collagenous plaques of the hands, keratoelastoidosis marginalis, digital papular calcinosis, acrokeratosis verruciformis of Hopf, mosaic acral keratosis, hereditary papulo-translucent acrokeratoderma and acrokeratoderma hereditarium punctatum.
Acrokeratoelastoidosis was first described by Oswaldo Costa in 1953 as small, firm, keratotic papules with central umbilication along the borders of hands and feet. [1] Although originally described as an autosomal dominant condition occurring in young adults, many sporadic cases occurring in older individuals have now been reported. A history of both excessive sun exposure and chronic trauma to the hands is noted in these patients. [2]
Histopathological findings help to differentiate this rare genodermatosis from other clinically similar conditions. H&E-stained sections show orthokeratotic hyperkeratosis, and hypergranulosis with or without epidermal hyperplasia. The reticular dermis shows reduced number of elastic fibers which are curled and fragmented as opposed to dense deposit of collagen fibers seen in degenerative collagenous plaques of the hand. [3] The absence of either of the above dermal changes is suggestive of focal acral hyperkeratosis. [4] The changes in elastic fibers are better appreciated with special stains such as Weigert, VVG, or Orcein. The hyperkeratosis has been attributed to the overproduction of filaggrin which is seen to accumulate as a dense band above the granular layer. Fibroblasts in the dermis, which are the precursors of elastin synthesis, are seen to contain abnormal dense granules in or near their plasma membrane. This suggests that the pathology in acrokeratoelastoidosis may be that of abnormality in the secretion of elastic fibers rather than that of fiber degradation, as the name suggests. [5]
The disease is described to be localized to the acral parts of the body; however Fiallo et al showed characteristic elastorrhexis in apparently normal skin in a patient with acrokeratoelastoidosis suggesting that the disorder could be regarded as a generalized defect of elastic tissue that is somehow limited in location. [6] Acrokeratoelastoidosis-like lesions in patients with scleroderma have been reported by Tajima et al and they postulate that it can be due to the abnormal connective tissue metabolism of systemic sclerosis. [7]
Treatment for this marginal keratoderma is mainly cosmetic. Topical keratolytics like salicylic acid and tretinoin provide temporary relief with recurrences on stopping application. Oral retinoic acid (50 mg/day) has not proved to be of benefit. [8] Er:YAG laser surgery has been tried but with limited clinical improvement. [9] Counseling regarding the benign nature of this lesion is essential.
| 1. |
Costa OG. Akrokerato-elastoidosis (a hitherto undescribed skin disease). Dermatologica 1953;107:164-8.
[Google Scholar]
|
| 2. |
Highet AS, Rook A, Anderson JR. Acrokeratoelastoidosis. Br J Dermatol 1982;106:337-44.
[Google Scholar]
|
| 3. |
Jeevankumar B, Thappa DM, Jayanthi S. Nail involvement in degenerative collagenous plaques of the hands. Indian J Dermatol Venereol Leprol 2003;69:309-10.
[Google Scholar]
|
| 4. |
Ballambat SP, Pai K. Acquired crateriform hyperkeratotic papules of the feet: An unusual variant of focal acral hyperkeratosis. Indian J Dermatol Venereol Leprol 2007;73:359-61.
[Google Scholar]
|
| 5. |
Meziane M, Senouci K, Ouidane Y, Chraïbi R, Marcil T, Mansouri F, et al. Acrokeratoelastoidosis. Dermatol Online J 2008;14:11.
[Google Scholar]
|
| 6. |
Fiallo P, Pesce C, Brusasco A, Nunzi E. Acrokeratoelastoidosis of Costa: A primary disease of the elastic tissue. J Cutan Pathol 1998;25:580-2.
[Google Scholar]
|
| 7. |
Tajima S, Tanaka N, Ishibashi A, Suzuki K. A variant of acrokeratoelastoidosis in systemic scleroderma: Report of 7 cases. J Am Acad Dermatol 2002;46:767-70.
[Google Scholar]
|
| 8. |
Bogle A, Hwang Y, Tschen A. Acrokeratoelastoidosis. J Am Acad Dermatol 2002;47:448-51.
[Google Scholar]
|
| 9. |
Erbil H, Sezer E, Koc E, Tunca M, Tastan HB, Demiriz M. Acrokeratoelastoidosis treated with the erbium: YAG laser. Clin Exp Dermatol 2008;33:30-1.
[Google Scholar]
|
Fulltext Views
3,655
PDF downloads
3,369





