Translate this page into:
Langerhans cell histiocytosis of the mandible in a six-year-old child
2 Department of Oral and Maxillofacial Surgery, Saveetha Dental College and Hospitals, Chennai, Tamil Nadu, India
3 Saveetha Dental College and Hospitals, Chennai, Tamil Nadu, India
Correspondence Address:
Pratibha Ramani
C/O Dr.V.R. Janaki, #3, Sri Ram Bhavan, 19, 3rd street, Abhiramapuram, Chennai-18, Tamil Nadu
India
| How to cite this article: Ramani P, Chandrasekar T, Baig MF, Muthusekar M R, Thomas S, Manyam R, Senthil M S. Langerhans cell histiocytosis of the mandible in a six-year-old child. Indian J Dermatol Venereol Leprol 2007;73:114-116 |
Abstract
Histiocytosis is a term applied to a group of rare disorders of the reticuloendothelial system. Eosinophilic granuloma, the most benign and localized of the three Langerhans cell histiocytosis entities, may be solitary or multiple. Eosinophilic granuloma can affect almost any bone, but commonly involves the mandible when the jaws are affected. Conventional treatment of LCH is with surgery, radiotherapy, chemotherapy and steroid injections, alone or in combination. Spontaneous regression of localized disease has also been reported. We report a six and a half-year-old patient with Langerhans cell histiocytosis - solitary eosinophilic granuloma of the mandible that initially regressed but rapidly recurred even after radical treatment and had a fatal outcome.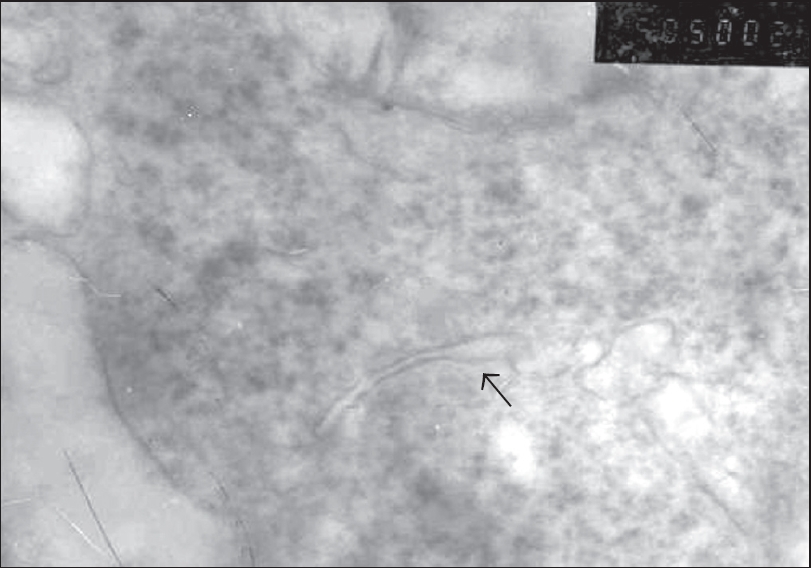 |
| Birbeck granules with terminal bulging giving a characteristic tennis racquet appearance |
 |
| Birbeck granules with terminal bulging giving a characteristic tennis racquet appearance |
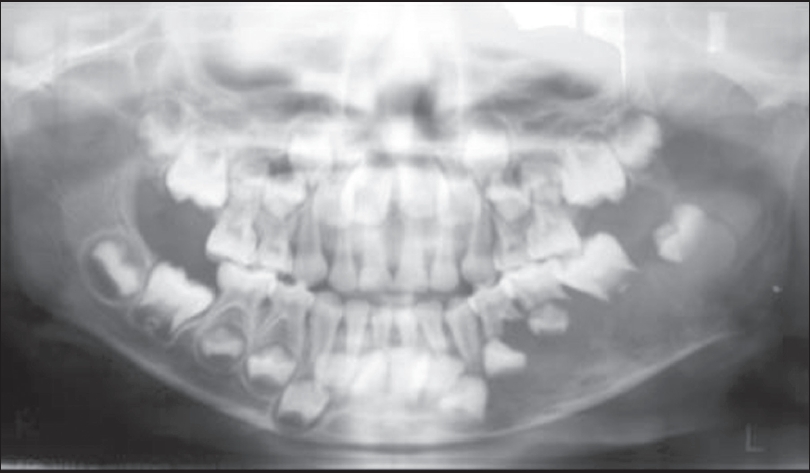 |
| Orthopantomogram revealed multilocular osteolytic lesion of the left mandible with fl oating teeth |
 |
| Orthopantomogram revealed multilocular osteolytic lesion of the left mandible with fl oating teeth |
 |
| Diffuse swelling of the left mandible |
 |
| Diffuse swelling of the left mandible |
INTRODUCTION
Histiocytosis is a term applied to a group of rare disorders of the reticuloendothelial system. Lichtenstein first suggested it in 1953. [1] Eosinophilic granuloma, the most benign and localized of the three Langerhans cell histiocytosis (LCH) entities might be solitary or multiple. It occurs most often in young adults and children. As many as half the patients with solitary lesions are younger than 10 years. [2] Eosinophilic granuloma can affect almost any bone, but commonly involves the mandible when the jaws are affected. [3] Conventional treatment of LCH is with surgery, radiotherapy, chemotherapy and steroid injections, alone or in combination. [4] Spontaneous regression of localized disease has also been reported. [5]
We report a patient of Langerhans cell histiocytosis - solitary eosinophilic granuloma of the mandible that initially regressed but rapidly recurred even after radical treatment and ultimately had a fatal outcome.
CASE REPORT
A six and a half-year-old girl was referred to the Department of Oral and Maxillofacial Surgery with the complaint of pain and swelling in the left lower jaw. The swelling was noticed a month back and an incisional biopsy was suggestive of fibroxanthoma.
On examination, a single, diffuse swelling measuring about 6 x 6 cm in size extending beyond the lower border of the left mandible was noted [Figure - 1]. On palpation, the swelling was tender, hard, immobile and attached to the underlying structures. Intraoral examination revealed a proliferating mass with both buccal and lingual expansion extending between deciduous left canine to the retromolar region of the mandible with well-defined margins. The submandibular lymph nodes were palpable, tender and mobile. The clinical differential diagnosis included reticuloendotheliosis, intraosseous sarcoma and hyperparathyroidism.
An orthopantomogram revealed a multilocular, osteolytic lesion of the left mandible with floating teeth [Figure - 2]. Complete hemogram showed a raised ESR. The differential leukocyte count revealed a moderately raised eosinophil count. Liver function and renal function tests were normal. An incisional biopsy was performed under local anesthesia. The specimen was friable and resembled granulation tissue. Histopathology showed proliferation of histiocytic cells and infiltration of eosinophils and neutrophils along with increased vascularity. Immunohistochemical staining showed that the histiocyte cells were positive for S100 protein. These features were consistent for eosinophilic granuloma.
To evaluate the possibility of systemic involvement, a radiographic skeletal survey and thallium 201 scintillography were done, but did not reveal any abnormality. Ultrasound of the abdomen did not reveal any organomegaly. The final diagnosis was solitary eosinophilic granuloma of the mandible.
To facilitate a peripheral ostectomy of the mandible, chemotherapy was started. Vincristine 1 mg was injected once a week for four weeks and oral prednisolone 25 mg daily was given for six weeks. On 8th July 2003, a peripheral ostectomy of the left mandible was performed under general anesthesia. The postoperative histopathology report was consistent with Langerhans cell histiocytosis. Transmission electron microscopic examination (TEM) of a small tissue sample of the postoperative specimen revealed straight or curved rod shaped granules arising from the cell membrane and growing into the cytoplasm. They showed terminal bulging, giving a characteristic tennis racquet appearance, which is diagnostic for Birbeck granules, confirming the diagnosis of Langerhans cell histiocytosis [Figure - 3]. The patient was discharged following an uneventful recovery.
The patient was rehospitalized after two months with complaints of headache, vomiting and worsening of the mandibular swelling with purulent discharge from it. Culture of pus from the swelling did not grow any organisms. Raised intracranial tension was clinically suspected but a CT scan of the brain (with contrast) ruled this out. The patient was given antibiotics, analgesics, anti-emetic drugs and intravenous/oral fluids. A subsequent radiograph showed a pathologic fracture with recurrence of the lesion. Injection ciprofloxacin 100 mg twice daily and injection metronidazole 100 mg twice daily with intravenous fluids was administered for five days, followed by mandibular resection. The histopathology and electron microscopy of the resected specimen confirmed LCH.
The patient was placed under intensive medical care as she was progressively losing weight and her general condition was deteriorating. However, she finally succumbed within twenty days to the disease.
DISCUSSION
Treatment of LCH of the jaws poses many problems, as shown by the history of our patient. Our patient clinically, radiographically as well as histopathologically had the features of Langerhans cell histiocytosis - solitary eosinophilic granuloma.
Along with Birbeck granules, LCH lesions may also contain lysosomes [6] as seen in our case in TEM. These lysosomes are said to be activated in response to steroids and causes apoptosis following radiation and chemotherapy [7] and does not indicate the reason for recurrence of the lesion.
The common side effects after chemotherapy including nausea, vomiting, hair loss, increased risk of infection, tiredness and diarrhea are very unusual, as mild treatment is generally recommended for LCH. A few children may develop recurrence many years later. [8] However, our patient had recurrence within one month of initial treatment. A hazard ratio of 7.1 and 11.6 for reactivation of LCH after initial treatment, implicating higher chances in multiple organ and bone involvement than solitary lesions. [9] Thus the chances for recurrence are higher in patients with multiple lesions when compared with patients with solitary lesion.
Langerhans cell histiocytosis - eosinophilic granuloma may be a benign, self-limited disease. However, in very rare instances, a solitary LCH may recur rapidly within a short duration and lead to a fatal outcome as seen in our patient.
| 1. |
Lichtenstein L. Histiocytosis X: Integration of eosinophilic granuloma of bone, Letterer-Siwe disease and Schuller-Christian disease as related manifestations of a single nosologic entity. Arch Pathol 1953;56:84-102.
[Google Scholar]
|
| 2. |
Gnanasekar JD, Ahmed MS, Reddy RR. Multifocal langerhans cell histiocytosis of the jaws: A case report. Quintessence Int 1991;22:559-64.
[Google Scholar]
|
| 3. |
Ardekian L, Peled M, Rosen D, Rachmiel A, Abu el-Naaj I, Laufer D. Clinical and radiographic features of eosinophilic granuloma in the jaws: Review of 41 lesions treated by surgery and low-dose radiotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:238-42.
[Google Scholar]
|
| 4. |
Roychoudhury A, Shah N, Parkash H, Mukhopadhyay S, Chopra P. Eosinophilic granuloma of the jaws. Br J Oral Maxillofac Surg 1998;36:380-3.
[Google Scholar]
|
| 5. |
Broadbent V, Pritchard J, Davies EG, Levinsky RJ, Heaf D, Atherton DJ, et al. Spontaneous remission of multi-system histiocytosis X. Lancet 1984;1:253-4.
[Google Scholar]
|
| 6. |
Miser JS, Pappo AS, Triche TJ, Merchant TE, Rao BN. Other soft tissue sarcomas of childhood. In: Pizzo PA, Poplack DG, editors. Principles and practice of pediatric oncology. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2002. p. 302.
[Google Scholar]
|
| 7. |
Ball A, Baratt GM, Wills ED. Activation of lysosomal enzymes and tumour regression caused by irradiation and steroid hormones. Eur J Cancer Clin Oncol 1982;18:489-94.
[Google Scholar]
|
| 8. |
Schepman KP, Radden BG, Van der Waal I. Langerhans' cell histiocytosis of the jaw bones: Report of 11 cases. Aust Dent J 1998;43:238-41.
[Google Scholar]
|
| 9. |
Predictors of outcome in children with Langerhan cell Histiocytosis. ASG, Annual meeting proceedings (post meeting edition). J Clin Oncol 2004;22:8550.
[Google Scholar]
|
Fulltext Views
3,354
PDF downloads
1,700





