Translate this page into:
Late-onset acquired dermal melanocytosis on the hand of a Chinese woman
Correspondence Address:
Bing R Zhou
Department of Dermatology, The First Affiliated Hospital of Nanjing Medical University, Guangzhou Road No. 300, Nanjing-210029
China
| How to cite this article: Permatasari F, Zhou BR, Luo D. Late-onset acquired dermal melanocytosis on the hand of a Chinese woman. Indian J Dermatol Venereol Leprol 2013;79:269 |
Sir,
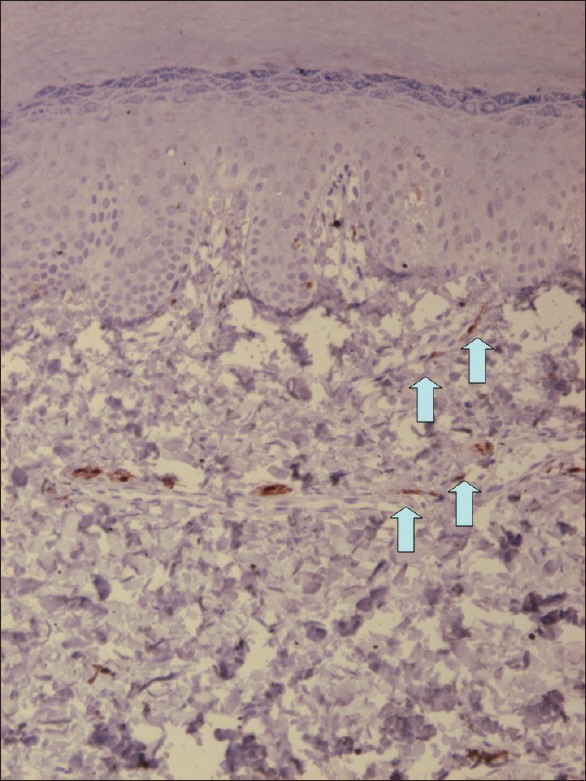
Dermal melanocytoses are characterized by a sparse population of intradermal dendritic, variably pigmented, spindle-shaped melanocytes. [1] Dermal melanocytoses result in a brown or a blue pigmentation depending on whether the melanin pigment is predominantly located in the upper or lower dermis, respectively. [1] Nevus of Ito, nevus of Ota, and Mongolian spot are 3 variants of dermal melanocytoses. [1] Here, we present a 35 year old Chinese woman with a gray-blue hyperpigmented patch on both palm and back of the right hand. The hyperpigmentation on the back of the right hand appeared about 20 years ago, and was always asymptomatic. The hyperpigmentation on the palm of the right hand appeared about 1 year ago, was also always asymptomatic, but had been progressively enlarged ever since. She denied any preceding trauma, discoloration or inflammation. There was a one year history of occupational exposure to certain chemical to clean steels, which is a kind of low-concentrated hydrochloric acid. She said she always wore rubber gloves during working. She said she was not sure whether the lesion appeared before or after she worked. Physical examination revealed macular gray-blue hyperpigmentation on the palm and back of the right hand [Figure - 1]. Histopathologic examination from the gray-blue patch on the palm and back of the right hand showed normal epidermis and a few spindle-shaped melanocytes containing melanin, which were sparsely scattered between the collagen bundles in the mid dermis, whose axis were parallel to the skin surface [Figure - 2] and [Figure - 3]. The pigmented cells were positive for S-100 [Figure - 4] and [Figure - 5] and HMB-45 staining [Figure - 6] and [Figure - 7]. Fontana-Masson silver stain revealed abundant brown pigment within the cytoplasm of the spindle cells [Figure - 8].
 |
| Figure 1: The right hand of a 35 year old Chinese woman (a) Gray-blue hyperpigmented patch on the back of the right hand which first appeared about 20 years ago (b) Gray-blue hyperpigmented patch on the palm of the right hand which first appeared about 1 year ago |
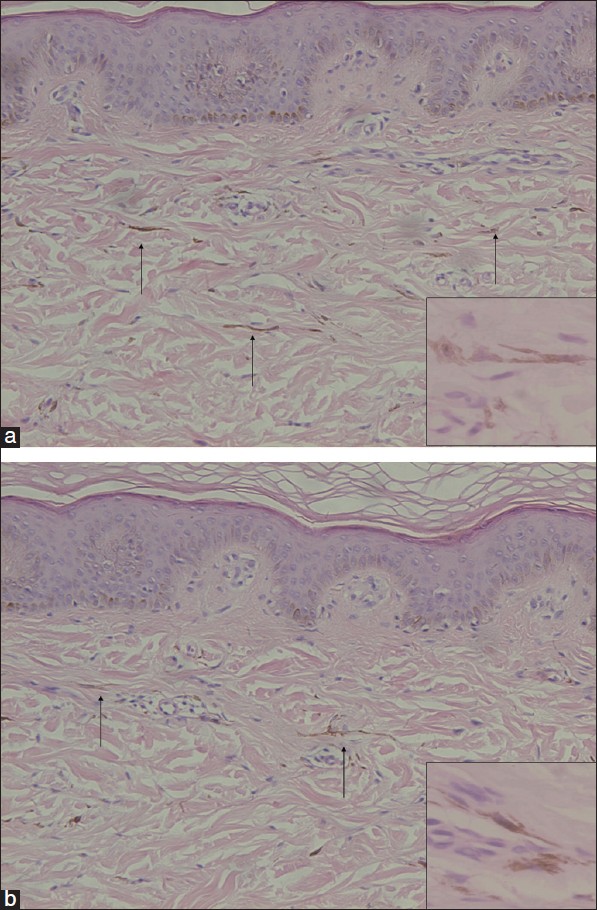 |
| Figure 2: Histopathologic examination from the gray-blue patch on the back (a) and palm (b) of the right hand showed a few spindle-shaped melanocytes containing melanin in the dermis. (H and E staining, 10 × magnification with enlarged images of 40 × magnification) |
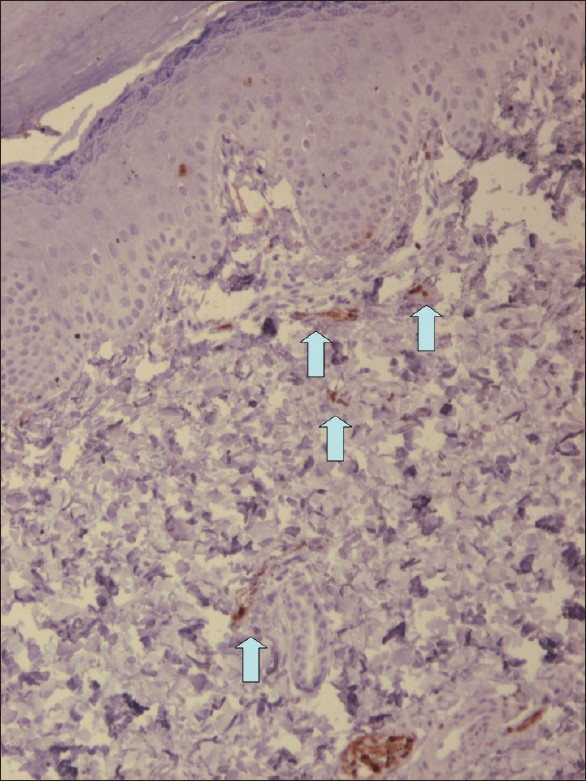 |
| Figure 3: S-100 staining shows positively stained cells in the dermis on the back of the right hand |
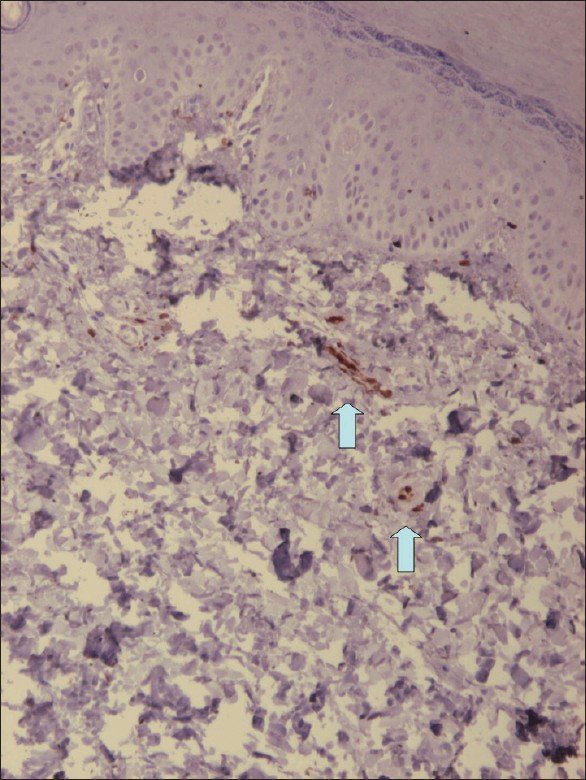 |
| Figure 4: S-100 staining shows positively stained cells in the dermis on the palm of the right hand |
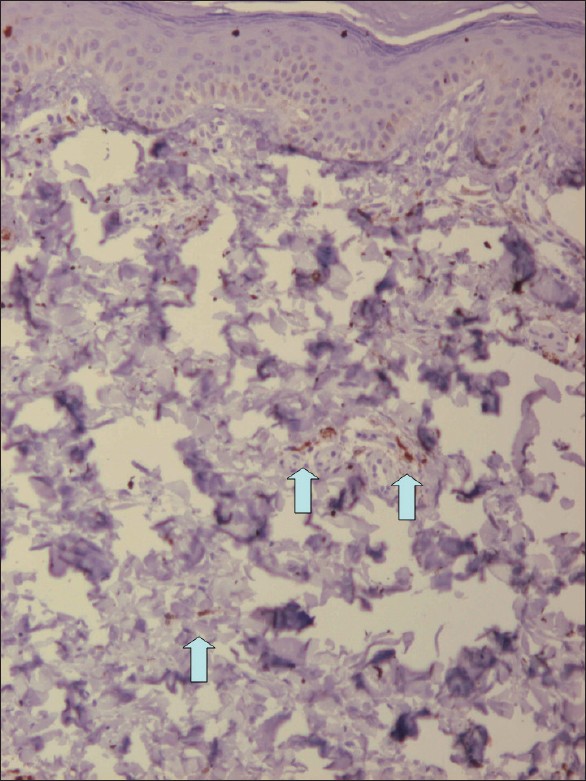 |
| Figure 5: HMB-45 staining shows positively stained cells in the dermis on the back of the right hand |
 |
| Figure 6: HMB-45 staining shows positively stained cells in the dermis on the palm of the right hand |
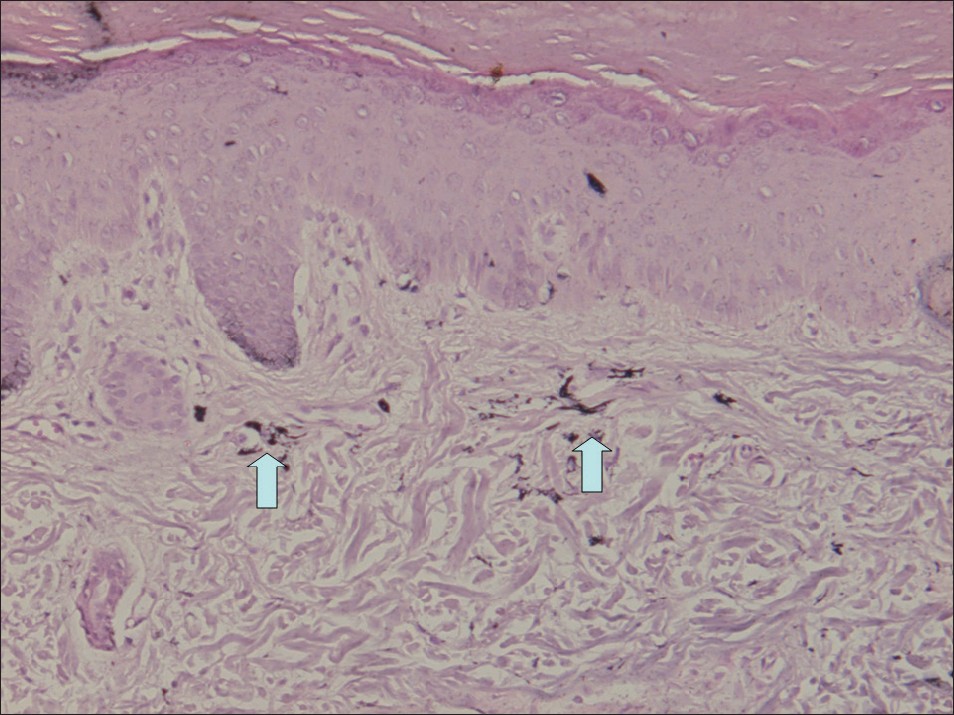 |
| Figure 7: Fontana-Masson silver staining on the back of the right hand showed a few spindle-shaped melanocytes containing melanin in the dermis |
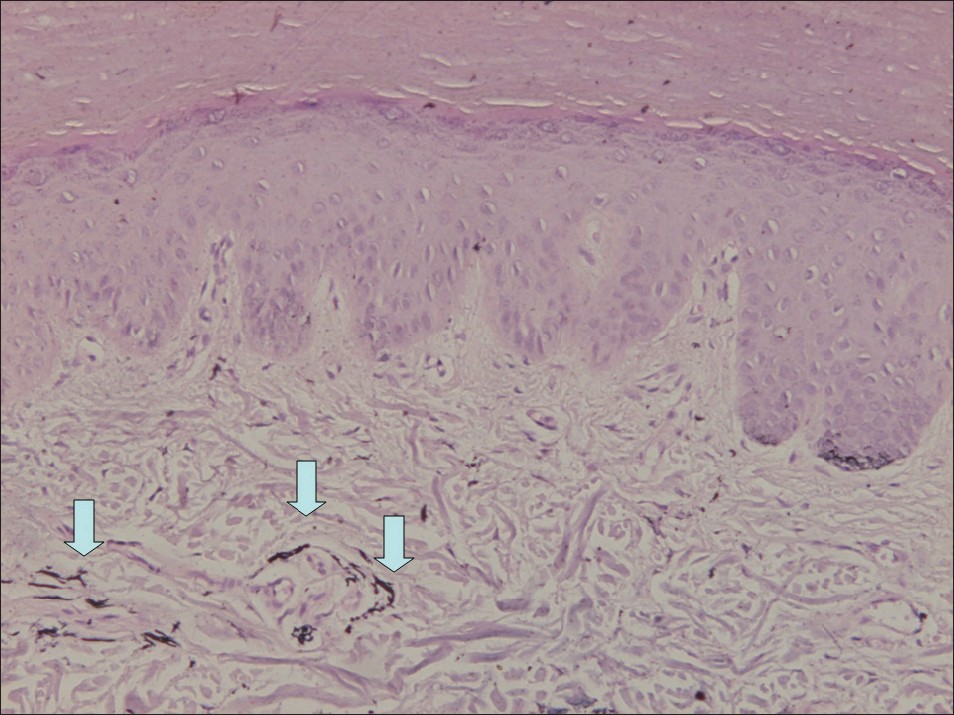 |
| Figure 8: Fontana-Masson silver staining on the palm of the right hand showed a few spindle-shaped melanocytes containing melanin in the dermis |
In the current case, the clinical presentation of hyperpigmentation and the histologic examination result of melanocytes in the dermis suggest the diagnosis of dermal melanocytoses. However, Mongolian spot is almost always located on the lumbosacral skin or on the buttocks, nevus of Ota usually follows the distribution of the first two branches of the trigeminal nerve. [1] Nevus of Ito usually follows the distribution of the lateral supraclavicular and lateral brachial nerves. [1],[2] Therefore, based on the site of involvement, this case is none of the 3 variants of dermal melanocytoses. The age of onset also exceeds the characteristic appearance period. Mongolian spots usually present at birth and generally regress spontaneously during childhood. [1] Over 50% of nevi of Ota and Ito are present at birth, most of the remainder appears around puberty, and they persist for life. [1],[2] One case reported the presence of dermal melanocytosis on the palm of left hand since birth. [3] Other than growing proportionately to the patient over the years, there had been no change in its size, colour or shape. [3] Although most dermal melanocytoses are congenital or appear during the childhood or adolescence, there is a rare group with a clearly acquired onset, known as acquired dermal melanocytosis (ADM). [2] Therefore, based on the site of hyperpigmentation and the age of onset, it is more suitable for the current case to be diagnosed as ADM on the hand.
There are 14 cases of ADM with atypical/extrafacial involvement with the age of onset above 20 years old have been reported to date, indicating the late onset [Table - 1]. Among these, there are only 3 cases of ADM on the hand. [12],[16] From these 3 cases, 2 cases reported possible associated factors, which are tanning bath and inflammation. [12],[16] The inflammation resulted from 12 year history of severe plaque-type psoriasis. [16] The distribution of the lesion over a patch of recently treated psoriasis on the back of left hand makes inflammation in the area a possible factor in the pathogenesis. [16] One case of acquired symmetrical dermal melanocytosis (ASDM) on the back of both hands also reported inflammation caused by atopic dermatitis as the associated factor. [17] However, the patient denied any history of inflammation on the hand, therefore inflammation is not the associated factor in this case.

It has been postulated that dermal melanocytes in ADM appear when melanocytes migrating from the neural crest during the embryological development fail to reach their proper location in the basal layer of the epidermis. [18] Alternatively, dermal melanocytes may migrate from the basal layer of the epidermis (dropping off) or from follicular bulbs. In addition, re-activation of preexisting latent dermal melanocytes may be triggered by unknown factors. This theory suggests that dormant dermal melanocytes may be present but unnoticed from birth. [7] This has been supported by the presence of melanocytes in the dermis of uninvolved skin adjacent to lesions. [11] The melanin synthesizing pathway is activated later by inflammation, local trauma, sex hormones or some unknown ageing stimuli. [7] A protective extracellular sheath enclosing dermal melanocytes has also been proposed as the mechanism for the stability of some these cells into adult life. [19]
The patient presented here may have had a genetic predisposition and may have already had dermal melanocytes present in this area. However, the distribution of the lesion over the palm makes exposure to chemicals in the area a possible associated factor in triggering the melanin synthesizing pathway, making the lesion progressively enlarged. We emphasize this case because it is the 1 st case of late onset ADM on the hand in Chinese ethnic group has been reported to date, with exposure to chemicals as a possible associated factor.
| 1. |
Stanford DG, Georgouras KE. Dermal melanocytosis: A clinical spectrum. Australas J Dermatol 1996;37:19-25.
[Google Scholar]
|
| 2. |
Mataix J, López N, Haro R, González E, Angulo J, Requena L. Late-onset Ito's nevus: An uncommon acquired dermal melanocytosis. J Cutan Pathol 2007;34:640-3.
[Google Scholar]
|
| 3. |
Kim S, Kim JA, Kim WS, Lee JH, Yang JM. Congenital dermal melanocytosis confined to the palm. J Eur Acad Dermatol Venereol 2007;21:1116-7.
[Google Scholar]
|
| 4. |
Pariser RJ, Bluemink GG. Acquired linear dermal melanocytosis. Nerve course distribution. Arch Dermatol 1982;118:125-8.
[Google Scholar]
|
| 5. |
Kawara S, Takata M, Hirone T, Tomita K, Hamaoka H. A new variety of neurocutaneous melanosis: Benign leptomeningeal melanocytoma associated with extensive Mongolian spot on the back. Nihon Hifuka Gakkai Zasshi 1989;99:561-6.
[Google Scholar]
|
| 6. |
Hidano A, Kaneko K. Acquired dermal melanocytosis of the face and extremities. Br J Dermatol 1991;124:96-9.
[Google Scholar]
|
| 7. |
Ono T, Egawa K, Kayashima K, Kitoh M. Late onset dermal melanocytosis: An upper back variant. J Dermatol 1991;18:97-103.
[Google Scholar]
|
| 8. |
Ono S, Hori M, Yamashita K, Yamakawa M. Generalised type of acquired dermal melanocytosis. Nihon Hifuka Gakkai Zasshi 1991;101:965-71.
[Google Scholar]
|
| 9. |
Shinohara. A case of dermal melanocytosis on the forearms and dorsal hands. Nishinihom J Dermatol 1994;56:1097.
[Google Scholar]
|
| 10. |
10 Kuniyuki S. Acquired dermal melanocytosis on the wrist. J Dermatol 1997;24:120-4.
[Google Scholar]
|
| 11. |
Mizushima J, Nogita T, Higaki Y, Horikoshi T, Kawashima M. Dormant melanocytes in the dermis: Do dermal melanocytes of acquired dermal melanocytosis exist from birth? Br J Dermatol 1998;139:349-50.
[Google Scholar]
|
| 12. |
Murakami F, Baba T, Mizoguchi M. Ultraviolet-induced generalized acquired dermal melanocytosis with numerous melanophages. Br J Dermatol 2000;142:184-6.
[Google Scholar]
|
| 13. |
Buka R, Mauch J, Phelps R, Rudikoff D. Acquired dermal melanocytosis in an African-American: A case report. J Am Acad Dermatol 2000;43:934-6.
[Google Scholar]
|
| 14. |
Rubin AI, Laborde SV, Stiller MJ. Acquired dermal melanocytosis: Appearance during pregnancy. J Am Acad Dermatol 2001; 45:609-13.
[Google Scholar]
|
| 15. |
Roth B, Grezard P, Balme B, Kanitakis J, Perrot H. Acquired dermal melanocytosis: Clinical, pathological and ultrastructural study. Ann Dermatol Venereol 2002;129:409-12.
[Google Scholar]
|
| 16. |
Kelley BP, Doherty SD, Calame A, Hsu S. Acquired dermal melanocytosis of the hand at the site of treated psoriasis. Dermatol Online J 2009;15:2.
[Google Scholar]
|
| 17. |
Murakami F, Soma Y, Mizoguchi M. Acquired symmetrical dermal melanocytosis (naevus of Hori) developing after aggravated atopic dermatitis. Br J Dermatol 2005;152:903-8.
[Google Scholar]
|
| 18. |
Fukuda M, Kitajima J, Fushida H, Hamada T. Acquired dermal melanocytosis of the hand: A new clinical type of dermal melanocytosis. J Dermatol 1993;20:561-5.
[Google Scholar]
|
| 19. |
Carmichael AJ, Tan CY, Abraham SM. Adult onset Mongolian spot. Clin Exp Dermatol 1993;18:72-4.
[Google Scholar]
|
Fulltext Views
3,700
PDF downloads
2,199





