Translate this page into:
Lichenoid skin lesions: A rare manifestation in secondary syphilis
2 Department of Pathology, University of Chile Clinical Hospital, Santiago, Chile
Correspondence Address:
Daniela Armijo
999 Santos Dumont Street, Santiago 8380456
Chile
| How to cite this article: Armijo D, Valenzuela F, Stevens J, Morales C. Lichenoid skin lesions: A rare manifestation in secondary syphilis. Indian J Dermatol Venereol Leprol 2020;86:105 |
Sir,
Syphilis, known as the “great imitator,” is a diagnostic challenge because of its similarity to numerous cutaneous pathologies, in both fully immunocompetent and immunocompromised patients. Moreover, patients with human immunodeficiency virus (HIV) infection may usually be affected by multiple dermatoses, many of them atypical and more severe than those observed in non-human immunodeficiency virus infected patients.[1]
Nowadays, syphilis and human immunodeficiency virus co-infection has become more frequent, and it is well-established that the depletion of CD4+ cells and increasing viral load can modify the natural course of syphilis and its cutaneous manifestations, as well.[2]
We report a case of secondary syphilis with concomitant lichenoid skin manifestations in a patient who presented with neurologic symptoms and was diagnosed with human immunodeficiency virus infection during hospitalization.
A 26-year-old Peruvian man presented to the emergency department with painful red eye, photophobia and progressive visual acuity reduction. He also complained of moderate intensity headache, tinnitus and dizziness. Eight months before, asymptomatic skin lesions appeared on his palms, soles and genitals. The patient denied past history of genital ulcer, but he confirmed history of multiple high-risk sexual encounters over the last year.
Physical examination revealed candidal plaques in the oral cavity, a pink macular rash on the thorax and rounded reddish plaques with a slightly scaly surface on the palms and soles. On the groin, there was a brownish plaque with irregular borders, hyperkeratotic surface with no distinctive findings on dermoscopy. On genital examination, there was an extensive brownish-gray plaque on the scrotum, perineal and perianal regions with well-defined edges and lichenoid surface [Figure - 1].
 |
| Figure 1: Dark pigmented brown plaque on the groin with scaly surface and an extensive brownish-gray plaque on the scrotum and penis, with lichenoid surface and well defined borders |
Venereal disease research laboratory test titers were high (1:256) and the fluorescent treponemal antibody-absorption test was positive. Enzyme-linked immunosorbent assay for human immunodeficiency virus was positive. Hepatitis B surface antigen and hepatitis B virus DNA were positive. Lumbar puncture revealed mononuclear lymphocytosis with increased protein and cerebrospinal fluid venereal disease research laboratory test titers were positive (1:8). The CD4 cell count was 353 cells/mm[3], and the viral load was above 40,000 copies/mL. Hepatitis C virus infection, Mycoplasma pneumoniae infection, cryptococcosis, tuberculosis, toxoplasmosis and Chagas disease were ruled out. Cerebral magnetic resonance images were normal.
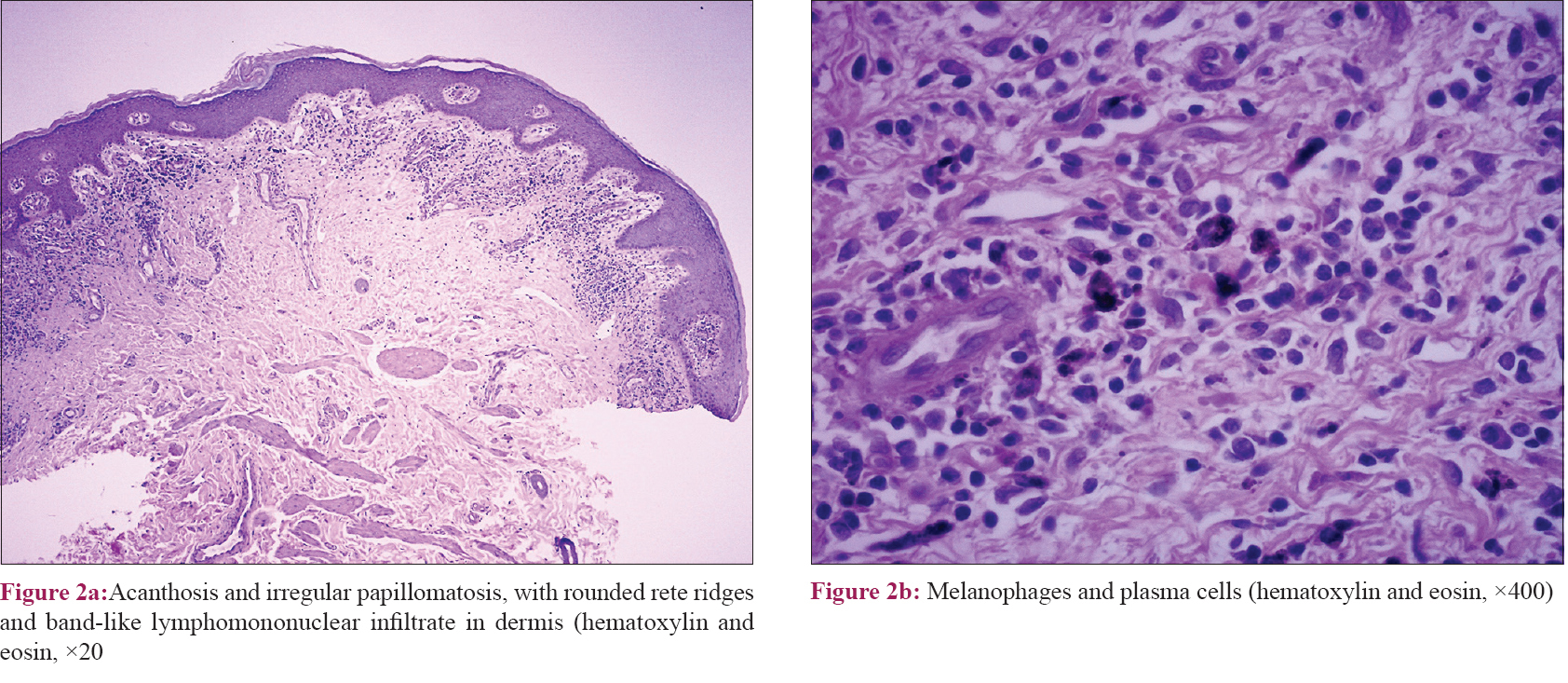
Owing to the atypical features of the lesions on the genitalia, two cutaneous biopsies were performed, one on the scrotal plaque and the other on the groin lesion. The histology of both areas was identical, and it showed acanthosis and irregular papillomatosis of the epidermis with mild hyperkeratosis and compact hypergranulosis [Figure - 2]a. There was a band-like inflammatory lymphomononuclear infiltrate with numerous melanophages and plasma cells throughout the superficial and deep dermis [Figure - 2]b. The microscopic examination for spirochetes was negative.
 |
On the basis of diagnosis of neurosyphilis, secondary syphilis and HIV, the patient was treated with sodium penicillin (4 million units every 4 hours intravenously for 14 days) and subsequently, antiretroviral therapy (emtricitabine/tenofovir + raltegravir) was started. Five hours after the onset of antibiotic treatment, he developed the Jarisch-Herxheimer reaction with myalgia, headache and fever. The symptoms were managed with acetaminophen and they resolved completely within 24 hours. During the hospitalization, the patient had an acceptable response to therapy without any adverse drug reactions. The neurological symptoms improved and the cutaneous lesions progressively started to diminish until they disappeared. The planned follow-up for the patient at discharge was serologic venereal disease research laboratory tests at 1, 3, 6, 12 and 24 months after the treatment, according to the Chilean sexually transmitted diseases guidelines, and cerebrospinal fluid examination after 6 months. He also received counselling about the correct and consistent use of latex condoms in every sexual encounter and the importance of proper treatment of the sexual partner.
The skin manifestations of secondary syphilis are so variable that they should be considered as part of many dermatological differential diagnoses. Although our patient had features of typical secondary syphilis, interestingly, the lesions on the scrotum and on the groin were atypical in morphology and location. Therefore, considering the immunosuppression, many differential diagnoses were suspected, including Bowen's disease, lichen planus, tinea, psoriasis, contact dermatitis and fixed drug reaction.
The presence of plasma cells and lichen planus-like changes on the histology confirmed the diagnosis of lichenoid lesions of syphilis.
Lichen planus-like eruptions are rare manifestations of secondary syphilis. They were more commonly described in the pre-penicillin era, and were supposed to be caused by the arsenical compounds used in the treatments of that time.
We found only few previous reports of lichenoid secondary syphilis published in the literature. Only one of them was a report of a genital lichenoid eczema-like lesion, whereas the other cases were annular lichen planus-like lesions.[3],[4],[5],[6]
Considering the HIV epidemic, it is highly advisable to pay close attention to the manifestations of any atypical skin rash, including lichenoid eruptions. Having a high level of suspicion of these symptoms is crucial to make an early diagnosis, so that we can ensure proper treatment and prevent any kind of severe complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
IvarsLleó M, ClavoEscribano P, Menéndez Prieto B. Atypical cutaneous manifestations in syphilis. ActasDermosifiliogr2016;107:275-83.
[Google Scholar]
|
| 2. |
Buchacz K, Patel P, Taylor M, Kerndt PR, Byers RH, Holmberg SD, et al. Syphilis increases HIV viral load and decreases CD4 cell counts in HIV-infected patients with new syphilis infections. AIDS 2004;18:2075-9.
[Google Scholar]
|
| 3. |
Tang MB, Yosipovitch G, Tan SH. Secondary syphilis presenting as a lichen planus-like rash. J Eur Acad Dermatol Venereol2004;18:185-7.
[Google Scholar]
|
| 4. |
Khurana A, Singal A, Gupta S. Annular lichenoid syphilis: A rare entity. Indian J Sex Transm Dis AIDS 2014;35:146-8.
[Google Scholar]
|
| 5. |
Narang T, De D, Dogra S, Kanwar AJ, Saikia UN. Secondary syphilis presenting as annular lichenoid plaques on the scrotum. J Cutan Med Surg 2008;12:114-6.
[Google Scholar]
|
| 6. |
Kang SH, Lee D, Park JH, Kang MS, Cho SH, Park SW, et al. Scrotal eczema-like lesion of secondary syphilis in an HIV-positive patient. Acta DermVenereol2005;85:536-7.
[Google Scholar]
|
Fulltext Views
3,810
PDF downloads
4,169





