Translate this page into:
Linear IgA bullous dermatosis induced by ampicillin/sulbactam
2 Department of Dermatology, Facultad de Medicina, Pontificia Universidad Cat�lica de Chile, Santiago, Chile
3 Department of Pathology, Facultad de Medicina, Pontificia Universidad Cat�lica de Chile, Santiago, Chile
Correspondence Address:
Fabiola Schafer
0868 Holandesa Ave, Temuco
Chile
| How to cite this article: Schafer F, Echeverria X, Gonzalez S. Linear IgA bullous dermatosis induced by ampicillin/sulbactam. Indian J Dermatol Venereol Leprol 2012;78:230 |
Sir,
Linear IgA bullous dermatosis (LAD) is a rare autoimmune blistering disorder characterized by subepidermal blisters with linear IgA deposition along the dermal-epidermal junction. Even though the majority of cases are idiopathic, some of them are drug-induced. Vancomycin is the medication most commonly reported in drug-induced LAD. However, other medications, such as gemcitabine, interferon-α 2a and piroxicam have also been reported. [1] As far as we know, ampicillin/sulbactam has only been reported in a case of localized LAD. [2] We describe a generalized LAD induced by ampicillin/sulbactam.
A 74-year-old woman with a medical history of hypertension was admitted for pneumococcal meningitis. On day 1, vancomycin and ceftriaxone were started. During the admission, she had serious complications such as myocardial infarction secondary to septic shock, frontal cerebral hemorrhage with neurological compromise due to septic vasculitis and nonconvulsive status′s epilepticus treated with levetiracetam, phenytoin and topiramate. On week 3, she presented with ventilator-associated pneumonia so for which ampicillin/sulbactam was started. Three days later, she developed a macular exanthem on her trunk, hips and thighs associated with tense vesicles and bullae in an annular pattern [Figure - 1]. Mucosal involvement and Nikolsky′s sign were negative. A skin biopsy of one of the bullae was performed and revealed a subepidermal blister with predominantly neutrophilic infiltration [Figure - 2]a. Direct immunofluorescence (DIF) showed linear deposits of IgA and C3 at the basement membrane zone (BMZ) [Figure - 2]b. The diagnosis of LAD was made. At the beginning, vancomycin was the suspicious drug, so it was withdrawn and a course of hydrocortisone 100 mg per day was started. However, after 3 days vancomycin was discontinued and skin lesions did not improve. Indeed, more vesicles and blisters appeared on the skin. On the other hand, a history of allergy to penicillin was obtained from a patient′s family member. Then, ampicillin/sulbactam was withdrawn and new blisters stopped within 24 hours and the eruption disappeared rapidly and completely within 2 weeks. Meanwhile, vancomycin was started again and a course of 10 days of this antibiotic was given without any skin complications.
 |
| Figure 1: Tense vesicles and bullae in an annular pattern on (a) the back and (b) the thigh |
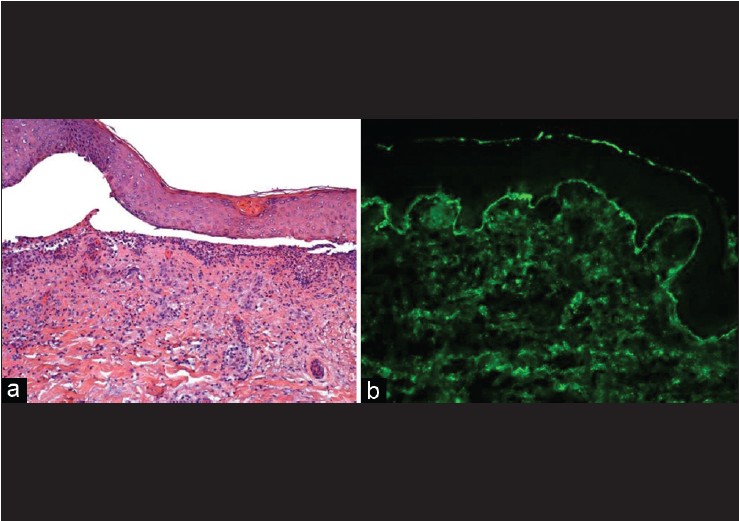 |
| Figure 2: (a) Subepidermal blister with neutrophilic infiltration (H and E, × 100). (b) Linear deposits of IgA and C3 along the dermoepidermal junction (direct immunofluorescence of perilesional skin, × 160) |
A minority of LAD cases is drug-induced, and the exact pathogenesis of drug-induced LAD remains obscure. The specificity of the autoimmune response in drug-induced LAD is not unique, and patient autoantibodies are directed to the same heterogenous group of proteins as in the idiopathic form. Probably, the drugs involved may elicit an autoimmune response by acting as haptens and producing neoautoantigens by chemical complexing with dermal/epidermal proteins. [2] These autoantigens are localized in the BMZ. BP180 is a transmembrane hemidesmosomal protein of basal keratinocytes. The extracellular domain of BP180 is converted to a 120-kd soluble fragment (LAD-1 antigen) by matrix metalloproteinases. Then, it is converted to a 97-kd protein (LAD97 antigen) by an unknown mechanism. LAD-1, LAD97, full-length BP180 and others such as BP230 and type VII collagen are the antigens most commonly recognized by circulating IgA autoantibodies. As such, LAD-1 antigen was detected in a case of localized ampicillin/sulbactam-induced LAD. [2] Interestingly, indirect immunofluorescence (IIF) on salt-split human skin does not detect circulating autoantibodies in drug-induced LAD. [3] Indeed, studies suggest that only a minority of patients with drug-induced LAD have circulating antibodies. In contrast, up to 80% of the patients with idiopathic LAD can have a positive IIF.
Interestingly, case reports have shown that not only deposits of IgA but also IgG and C3 complement can be found at the BMZ in DIF. [4],[5],[6] Indeed, Plunkett et al., [3] found that 11% of drug-induced LAD cases had deposits of IgG at BMZ and other three cases presented non-disease-specific DIF findings, suggesting that LAD may be an epiphenomenon in drug-induced blistering diseases. Moreover, Neughebauer et al., [4] reported that 32% of drug-induced LAD cases showed linear deposition of C3 at BMZ. Here we report a case of drug-induced LAD with linear deposition of both IgA and C3 along the dermal-epidermal junction. Further studies looking for C3 complement as a possible diagnostic marker that can separate drug-induced cases from idiopathic form are warranted.
Drug-induced LAD has a transient course with spontaneous remission and clearance of immune deposits after withdrawal of the drug. The interval from the administration of a drug to onset of the rash ranges from 1 to 15 days, with a mean onset of approximately 8 days. [5] Usually, a primary asymptomatic autoimmune response is induced during an early brief exposure to the drug. Renewed administration of the same medication may trigger a rapid and more potent secondary immune response resulting in blister formation. In our patient the blistering eruption occurred 3 days following the first dose of ampicillin/sulbactam. The rapid onset of our case might have been due to the previous exposure to the drug. The development of lesions after starting the ampicillin/sulbactam treatment and the gradual resolution and complete recovery after withdrawal of the drug represents the strongest evidences for our diagnosis. Even though a rechallenge of the suspicious drug can reproduce the skin eruption and identify the offending drug, a complete clearance of the skin lesions occurred in our patient when ampicillin/sulbactam was discontinued and vancomycin was started again. For ethical reasons, we did not rechallenge the patient with the drug.
Interestingly, it seems that ampicillin/sulbactam may induce two variants (localized and generalized) of LAD. However, further studies are needed in order to clarify its involvement and the possible variants related to LAD.
In addition to our patient, only one case of localized ampicillin/sulbactam-related LAD has been reported in the literature. Therefore, to our knowledge, our patient is the first case of generalized ampicillin/sulbactam-induced LAD.
In this report the diagnosis of LAD represented a challenge due to the polypharmacy of the patient and the skin lesions, which were similar to bullous pemphigoid. Nevertheless, the clinical history and the skin biopsy were key tools for the diagnosis.
| 1. |
Kocyigit P, Akay BN, Karaosmanoglu N. Linear IgA bullous dermatosis induced by interferon-alpha 2a. Clin Exp Dermatol 2009;34:123-4.
[Google Scholar]
|
| 2. |
Shimanovich I, Rose C, Sitaru C, Brocker EB, Zillikens D. Localized linear IgA disease induced by ampicillin/sulbactam. J Am Acad Dermatol 2004;51:95-8.
[Google Scholar]
|
| 3. |
Plunkett RW, Chiarello SE, Beutner EH. Linear IgA bullous dermatosis in one of two piroxicam-induced eruptions: A distinct direct immunofluoresence trend revealed by the literature. J Am Acad Dermatol 2001;45:691-6.
[Google Scholar]
|
| 4. |
Neughebauer B, Negron G, Pelton S, Plunkett R, Beutner E, Magnussen R. Bullous skin disease: An unusual allergic reaction to vancomycin. Am J Med Sci 2002;323:273-8.
[Google Scholar]
|
| 5. |
Navi D, Michael D, Fazel N. Drug-induced linear IgA bullous dermatosis. Dermatol Online J 2006;12:12.
[Google Scholar]
|
| 6. |
Onodera H, Mihm MC, Yoshida A, Akasaka T. Drug-induced linear IgA bullous dermatosis. J Dermatol 2005;32:759-64.
[Google Scholar]
|
Fulltext Views
2,757
PDF downloads
3,198





