Translate this page into:
Linear nodulo-ulcerative lesions in a child
Correspondence Address:
H Hanumanthappa
Department of Skin and STD Government Medical College, Mysore, Karnataka
India
| How to cite this article: Hanumanthappa H, Rashmi S. Linear nodulo-ulcerative lesions in a child. Indian J Dermatol Venereol Leprol 2006;72:326 |
 |
 |
 |
 |
 |
 |
 |
 |
A 11 year-old girl developed an injury due to a thorn prick to her left forearm, while working in an agricultural field. A single non-healing ulcer appeared on the medial aspect of the left forearm, 20 days later. After 4 months, multiple ulcers and nodules developed in a linear distribution along the left fore arm, upto the axilla. Few of the nodules burst open to produce ulcers and scars.
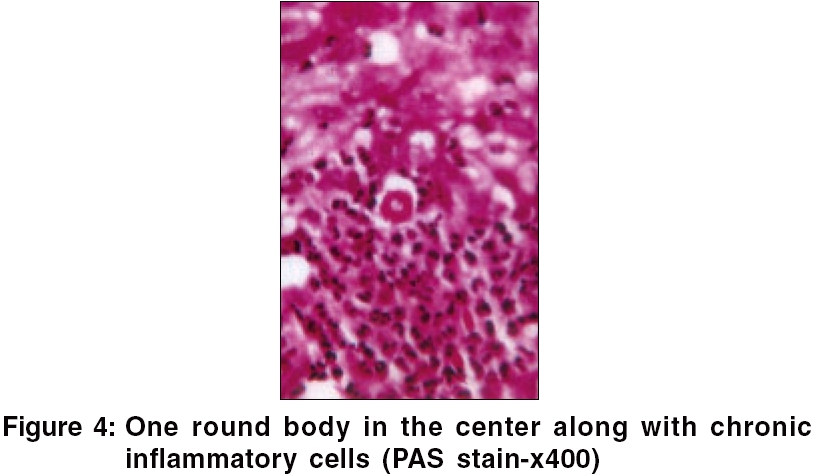
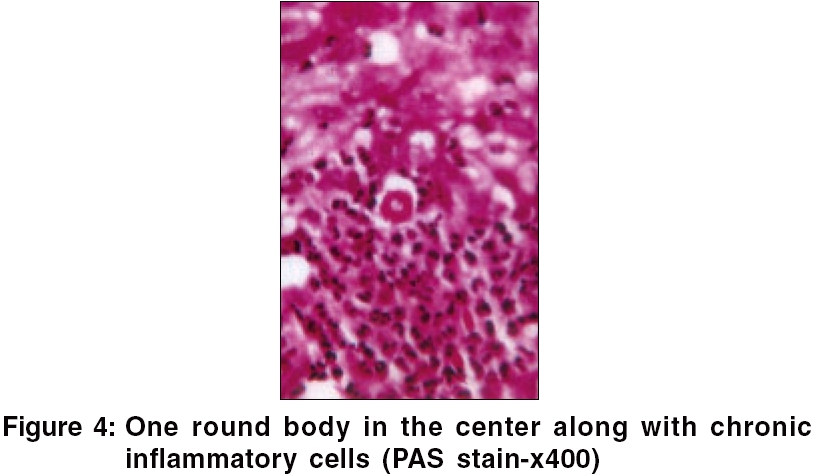
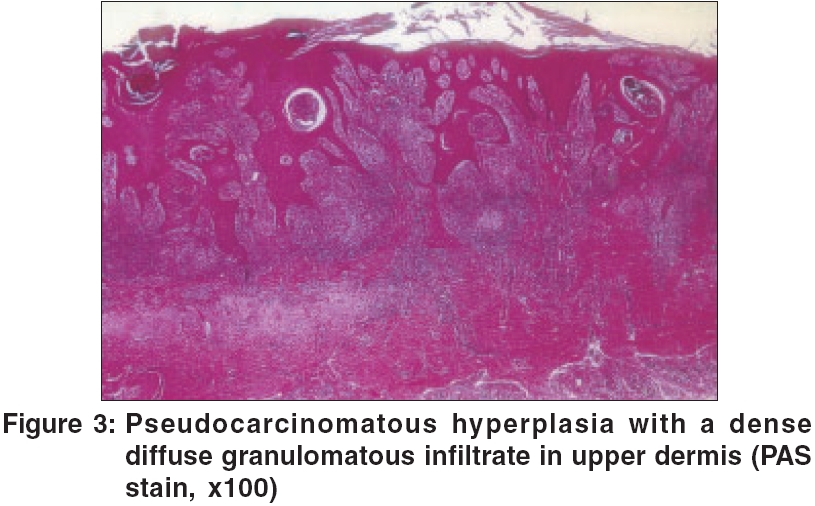
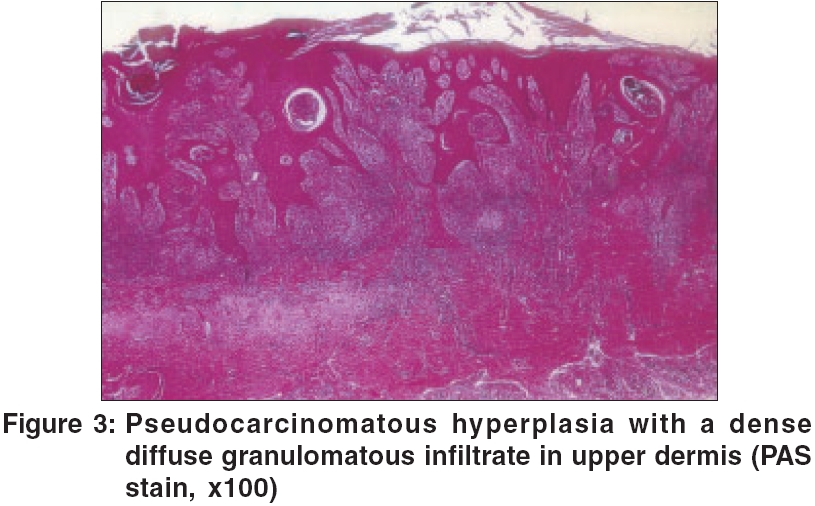
On examination; an ulcerative, papillomatous growth, puckered scars and keloids on the inner aspect of the left forearm extending up to axilla, were seen [Figure - 1][Figure - 2]. The ulcers were irregular, tender and not fixed to underlying structures. Axillary lymph nodes were enlarged, firm, slightly tender and discrete. Systemic examination was normal. Routine investigations were normal. HIV test was negative. Microscopic examination of the purulent discharge from the lesion with KOH, Gram stain and AFB stain was negative and it was sent for culture. Skin biopsy showed several round to oval bodies, [Figure - 3] and one round body in the centre along with chronic inflammatory cells [Figure - 4].
What is your diagnosis?
Diagnosis: Lymphocutaneous sporotrichosis
Culture on Sabouraud′s dextrose agar revealed growth of multiple fungal colonies, which were grayish-black in colour. Skin biopsy with PAS stain showed several round to oval spores of Sporothrix schenckii [Figure - 3]. One spore located in the centre showed single budding along with chronic inflammatory cells. [Figure - 4] The diagnosis of lympho-cutaneous sporotrichosis was made and the child was put on itraconazole 100 mg, daily. She showed good response up to two months, but did not follow-up subsequently.
Discussion
Sporotrichosis is an acute or chronic fungal infection caused by Sporothrix schenckii . Cutaneous and systemic forms of sporotrichosis exist. It is more prevalent in temperate climate. The fungus grows on decaying vegetable matter and the source is probably the soil.[1] The first case was reported by Schenk in 1898 from USA. Some cases are reported from India.[2] A number of cases have also been reported from Himachal Pradesh and adjoining areas.[3] However, the Southern part of India is considered to be relatively free from sporotrichosis and only sporadic case reports are available in literature.[4],[5]
The clinical forms of cutaneous sporotrichosis are of two types viz, lymphocutaneous and fixed cutaneous forms. Occasionally, mycetoma-like or cellulitic forms may occur. In the present case, lymphocutaneous type was described. It is important to note that multiple cutaneous lesions may occur in AIDS patients.[1]
Sometimes the culture may be negative and biopsy is non-specific.[4] But in our patient, both were confirmative of sporotrichosis. Potassium iodide is extremely effective in Iocalized forms and should be continued for 3-4 weeks after clinical cure. Itraconazole 100 mg - 200 mg/day is effective in both cutaneous and systemic cases.
A careful history and investigations lead to confirmed diagnosis in a patient presenting with linear noduloulcerative lesions.
| 1. |
Hay RJ, Moore MK. Mycology. In : Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of dermatology, 7th ed. Oxford: Blackwell Science; 2004. p. 31.76-8.
[Google Scholar]
|
| 2. |
Sanyal M, Basu N, Thammayya A, Tutakne MA, Gaind ML. Subcutaneous sporotrichosis in India. Indian J Dermatol Venereol Leprol 1973;39:88-91.
[Google Scholar]
|
| 3. |
Sharma NL, Sharma RC, Gupta ML. Sporotrichosis-Study of 22 cases from Himachal Pradesh. Indian J Dermatol Venereol Leprol 1990;56:296-8.
[Google Scholar]
|
| 4. |
Nagabhushanam P. Sporotrichosis. Indian J Dermatol 1967;33:276-7.
[Google Scholar]
|
| 5. |
Pankajalakshmi VV, Taralakshmi VV, Subramanian S. Sporotrichosis in Madras. Indian J Dermatol Venereol Leprol 1976;42:140-2.
[Google Scholar]
|
Fulltext Views
2,379
PDF downloads
3,108





