Translate this page into:
Low dose intravenous immunoglobulins and steroids in toxic epidermal necrolysis: A prospective comparative open-labelled study of 36 cases
2 Department of Community Medicine, Government Medical College, Kottayam, Kerala, India
Correspondence Address:
K Sobhanakumari
Department of Dermatology, Government Medical College, Kottayam, Kerala - 686008
India
| How to cite this article: Jagadeesan S, Sobhanakumari K, Sadanandan SM, Ravindran S, Divakaran MV, Skaria L, Kurien G. Low dose intravenous immunoglobulins and steroids in toxic epidermal necrolysis: A prospective comparative open-labelled study of 36 cases. Indian J Dermatol Venereol Leprol 2013;79:506-511 |
Abstract
Background: Toxic epidermal necrolysis (TEN) is a severe adverse drug reaction associated with high mortality. Though different modalities of treatment are advocated, there is no consensus regarding specific therapy. Corticosteroids have shown conflicting results and for high dose intravenous immunoglobulins (IVIG), cost is a limiting factor. Aim: To find out the effectiveness of combination therapy with low-dose IVIG and steroids versus steroids alone in our TEN patients. Methods: After obtaining Ethical Committee approval, 36 consecutive TEN patients (2008-2012) were alternately allocated to 2 groups - Group A was given combination of low-dose IVIG (0.2-0.5 g/kg) and rapidly tapering course of steroids (intravenous dexamethasone 0.1- 0.3 mg/kg/day tapered in 1-2 weeks) while Group B was given same dose of steroids alone. Outcome parameters assessed were time taken for arrest of disease progression, time taken for re-epithelization, duration of hospital stay and mortality rates. Results: Both groups had 18 patients. Baseline characteristics like age, sex ratio, SCORTEN, body surface area involvement and treatment interval were comparable. Time for arrest of disease progression and for re-epithelization was significantly lowered in Group A (P = 0.0001, P = 0.0009 respectively). Though duration of hospital stay and deaths were less in Group A, difference was not statistically significant. SCORTEN based standardized mortality ratio (SMR) analysis revealed that combination therapy reduced the probability of dying by 82% (SMR = 0.18 ± 0.36) and steroids by 37% (SMR = 0.63 ± 0.71). Difference in SMR was statistically significant (P = 0.00001). No significant side effects due to either modality were found in any of the patients. Conclusion: Combination therapy with low-dose IVIG and steroids is more effective in terms of reduced mortality and faster disease resolution when compared to steroids alone in TEN.Introduction
Toxic epidermal necrolysis (TEN) is a life threatening severe cutaneous adverse drug reaction. It is caused by widespread keratinocyte apoptosis mediated by the Fas- Fas ligand and the perforin - granzyme pathway. [1] Beyond immediate cessation of the offending drug and adequate supportive care preferably in a burns unit, a lack of clarity prevails regarding specific management. The available studies reveal a dichotomy of opinion regarding the effectiveness of both corticosteroids and intravenous immunoglobulin (IVIG) in the treatment of TEN. [2] Furthermore, the increased cost of high dose IVIG, the more recently favored biologic, preclude their use in most of our patients.
This situation prompted us to try a combination therapy with IVIG and steroids as they target the disease at different levels of pathogenesis. The exact dose of IVIG effective in TEN differs in various studies with most of them employing a total cumulative dose between 1.5 g/kg and 3.5 g/kg. [3] A few studies have reported improvement even with a low-dose of 0.1 - 0.5 g/kg. [4],[5] As the inhibition of Fas-Fas ligand interaction by IVIG is not an ′all or none′ phenomenon, and the lower cumulative dosing considerably increased the affordability of IVIG in our patients, we considered it worthwhile to probe its effect.
To the best of our knowledge, the combination of low-dose IVIG and steroids is a novel therapeutic option in TEN, not reported in any trials previously. We hypothesize that while the lower dose of IVIG improves the safety and affordability, the addition of steroids might increase the effectiveness by a possible synergistic effect.
Methods
A prospective open labeled study was conducted in the Dermatology ward of our center, which is an 837-bedded tertiary care teaching hospital. Ethical clearance for this study was obtained from the Institutional Review Board. Informed consent was taken from all the patients/guardians after detailed explanation of study procedures. The study subjects were all consecutive patients diagnosed and admitted as TEN in the 4 year time interval between February 2008 and January 2012. The diagnosis was based on the history of drug ingestion (WHO causality definition - certain/probable), [6] clinical findings with body surface area (BSA) involvement of > 30% as per Bastuji- Garin classification [7] and exclusion of similar disorders, especially autoimmune bullous disorders. Tzanck smear examination was done in all patients. Skin biopsy was performed only in doubtful cases to avoid further trauma. Complete blood investigations, urine microscopy and cultures, chest X-rays, Venereal Disease Research Laboratory test, ELISA for HIV, antinuclear antibody, blood cultures and pus cultures were also done.
Out of the total 38 patients who were admitted with TEN during the study period, two patients with contraindications to steroid/IVIG treatment were excluded from the study. The remaining 36 patients were alternately allocated to two groups of 18 each. The patients in the combination therapy group (Group A) were treated with IVIG in a cumulative dose of 0.2 - 0.5 g/kg (Trade name - GAMMA I.V., manufactured by Bharat Serums and Vaccines Limited) divided over 3 days along with systemic steroids. The preferred systemic steroid preparation used was intravenous dexamethasone in a dose of 0.1-0.3 mg/kg/day and rapidly tapered within 1-2 weeks according to response. Group B patients were treated with the same dose of steroids alone. Patients in both groups were given intensive supportive treatment along with prompt and meticulous ophthalmic care and care of oral and genital mucosa. Since there is no test to identify the offending drug beyond doubt, all ongoing medications were stopped/substituted. Immediate complications and side effects of the treatment modalities, if any, were noted in all patients. After discharge, all patients were scheduled for follow-up visits until 6 months and long-time complications, if any were recorded.
Scorten
SCORTEN, a severity-of- illness score for TEN patients described by Bastuji- Garin et al. [7] was calculated for each patient at the time of admission. Each point is allotted for one of the following parameters - age > 40, malignancy, heart rate > 120/min, initial % of epidermal detachment > 10 %, Blood urea > 28 mg/dl, RBS > 252mg/dl and serum bicarbonate < 20 mEq/L. The score ranges from a minimum of 0 to a maximum of 7 and is thought to accurately predict risk of death in TEN patients. A score of 0-1 is associated with a 3.2% risk of mortality whereas if the score is ≥ 5, the risk of death is 90%. [8]
Statistical analysis
Data was entered in Microsoft Excel and analyzed by the software SPSS, version 16.0. The measures of outcome determined were - the time taken for arrest of disease progression (no new lesions, Nikolsky turned negative, exudation reduced), time taken for re-epithelization, duration of hospital stay and the mortality rates. The analysis of mortality rates was done on the basis of SCORTEN; the actual death rates were compared to SCORTEN predicted mortality rates by standardized mortality ratio (SMR) analysis (SMR = total observed deaths/total expected deaths). The statistical comparisons of the qualitative data were done using Chi- square test and quantitative data using Student′s t - test. Statistical significance was defined as P < 0.05. Multivariate analysis using multiple linear regression was also performed wherever appropriate.
Results
The average age was 37 years (6 - 68years) of which 6 were children. Females dominated (20/36). The most common drugs implicated were aromatic anticonvulsants (24/36, 66.67%) with carbamazepine responsible in 12 cases, phenytoin in 9, both together in 2 and phenobarbitone in 1 case. The most common indication for starting these drugs was seizure disorder followed by head injury. One patient had malignancy with brain metastasis and another had an astrocytoma. There were 2 patients with HIV in this cohort, both with CD4 counts < 200, who were started on anti retroviral treatment containing nevirapine within the last 2 months.
The mean incubation period was 16.02 ± 6.80 days. The mean percentage of BSA involved (detached/ detachable) was 51.16%. There were a total of four deaths (11.11%); 1 in Group A and 3 in Group B. The death in Group A occurred in a 68 year old patient with multiple co-morbidities, on the 4 th day of admission. The cause of death was attributed to sepsis, not responding to antibiotic treatment. Of the three deaths in Group B, 2 occurred as a result of pneumonitis with acute respiratory failure and the 3 rd patient suffered from multi-organ failure. The three deaths occurred on the 8 th , 7 th and 9 th day of admission respectively. All the deaths occurred despite intensive critical care treatment supervised by a panel of specialists.
During the clinical course of the disease, commonest complications encountered were bacterial infections; which were noted in 15 patients (skin - 6, urinary tract -3, respiratory tract -6, positive blood cultures - 5)
all of whom responded to broad spectrum systemic antibiotics except one who succumbed to septicemia. Furthermore, there was one patient who developed thrombocytopenia and another who developed agranulocytosis. The long term complications noted were - pigmentary alteration in seven patients, vulvar synechiae in one, ocular symblepharon in one and corneal epithelial defects in two patients. No major immediate or long term treatment related side effects were noted in any of the patients.
Of the six pediatric patients in this cohort, all were females except one. The causative drug was aromatic anticonvulsants in five of them (started for seizure disorder in four and following head injury in one). Mean incubation period was 15 days, mean BSA involvement was 43.83%, and median SCORTEN was two. Three of them were treated with combination therapy and the others with steroids alone. No deaths occurred. Average time taken for arrest of progression was 5.33 days, for re-epithelization was 9.67 days and mean duration of hospital stay was 15.5 days. No long term complications were seen except for pigmentation.
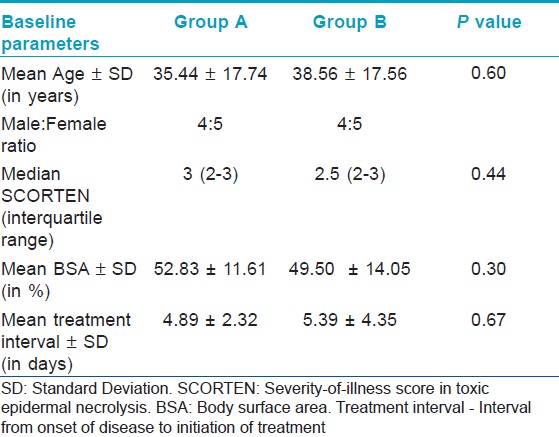
On comparing the baseline characteristics of group A and group B, i.e., age, sex, SCORTEN, BSA involvement and interval between onset of disease and initiation of treatment [Table - 1], all were found to be comparable (P > 0.05) in both the groups.
On comparing the outcome parameters of Groups A and B [Table - 2], a statistically significant difference was noted between the two groups in the time taken for arrest of disease progression, and time taken for epithelization [Figure - 1] and [Figure - 2]. This means that the addition of low-dose IVIG to steroids resulted in an earlier clinical improvement. The duration of hospital stay and mortality rate even though less in the combination group, the difference was not statistically significant. Multivariate analysis with all explanatory variables were done by multiple linear regression model using dependent variables as time taken for arrest of progression of disease and time for epithelization. Only the treatment given was found to be a significant explanatory variable in the regression model in both.
 |
| Figure 1: A patient with phenytoin induced toxic epidermal necrolysis treated with combination therapy (a, b) on the 2nd day of admission. (c, d ) The same patient on day 9 |
 |
| Figure 2: A patient with carbamazepine induced toxic epidermal necrolysis treated with intravenous dexamethasone alone (a) on the 1st day of admission. (b) on the 2nd day. (c) The same patient on day 12 |
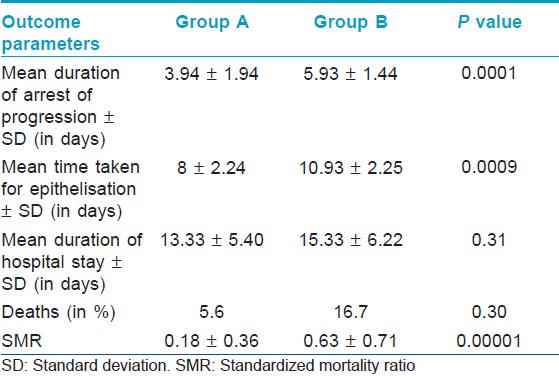
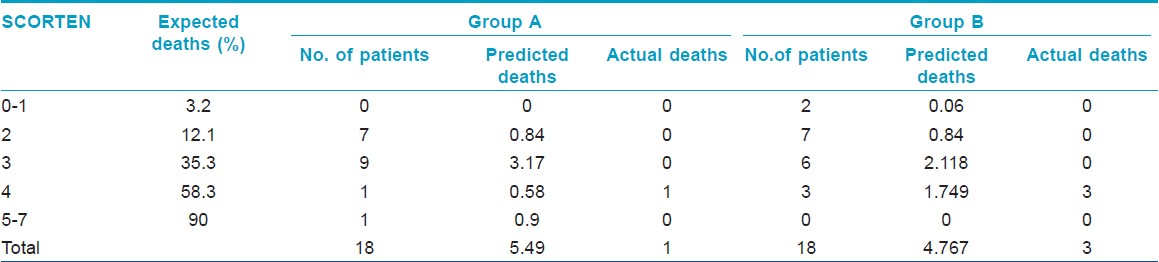
On comparing the actual mortality rates to SCORTEN predicted mortality rate [Table - 3], it was found that combination therapy highly reduced the chances of death. While the SCORTEN predicted mortality in Group A patients was 5.49 deaths, in fact only 1 death occurred. SMR analysis revealed that there is an 82 % less probability of dying when treated with combination therapy. In the steroid group, SCORTEN predicted mortality was 4.76 deaths while actually there were only three deaths. SMR analysis revealed that steroids lower the probability of dying by 37%. Thus, though not as effective as the combination therapy, steroids alone also tended to reduce the mortality rates of our TEN patients. However, the difference in SMR between the groups was found to be statistically significant (P = 0.00001) indicating a superiority for combination therapy in terms of mortality also.
Discussion
Although TEN has been a well-recognized clinical entity since it was described by Lyell in 1956, there is no formally established systematic protocol for its treatment. [2] Corticosteroids have been routinely used in our center for the management of TEN since the past decade and we have found it useful in achieving early control of the disease despite many studies claiming otherwise. The general negative opinion about corticosteroids is probably because they are often given too late, in too low a dose and for too long. [9] Many studies from India have claimed beneficial effects with systemic corticosteroids [10],[11] and according to the therapeutic guidelines published by the Indian Association of Dermatologists, Venereologists and Leprologists, corticosteroids have a place in the management of TEN if given early in the disease and tapered promptly. [12] Corticosteroids are thought to act by having suppressive effects on the cytotoxic T lymphocytes and also inhibit interferon gamma mediated apoptosis. Moreover, they have pleomorphic effects on the immune system including inhibition of chemokines and numerous cytokines like TNF-alpha. [9]
IVIG on the other hand, is a highly purified Immunoglobulin G prepared from pooled plasma with trace amounts of Immunoglobulin A or Immunoglobulin M. [3] It possesses anti-Fas activity and inhibits keratinocyte apoptosis by blocking the binding of Fas - ligand to Fas receptors. [1] Additionally, IVIG has anti infective properties and also corrects protein and fluid loss. Potential side effects include thromboembolism, aseptic meningitis, hemolysis, vasomotor symptoms and anaphylactic reactions but is generally well tolerated by patients who have adequate renal function. [13]
A number of retrospective and prospective studies have been conducted to examine the efficacy and safety of IVIG in TEN patients. Viard et al., Metry et al. and Tristani - Firouzi et al. found IVIG to have a beneficial effect in TEN whereas the study by Brown et al. and the EuroSCAR study demonstrated no benefit. [1],[14],[15],[16],[17] It seems impossible to draw a consensus regarding the effectiveness of IVIG in the absence of prospective, controlled, multi-centric trials. But one inference that may be drawn regarding the contrasting results is that Fas - Fas ligand interactions may not be the only mechanism of apoptosis active in TEN; other pathogenic mechanisms may be responsible for the damage. In view of the accumulating experimental evidence for the role of cytotoxic T lymphocytes in the destruction of the epithelium, there may be a rationale for the effectiveness of steroids in Stevens-Johnson Syndrome / TEN. [2]
In this context, combination therapy seems an attractive choice. Combining steroids with IVIG is a feasible option as they do not have a similar adverse effect profile, and may have a synergistic action targeting the different pathways of apoptosis active in TEN. Very few authors have studied the beneficial effects of combination of IVIG and steroids. [18],[19] But the dose of IVIG used in most studies is around 2 g/kg.
The increased cost takes high-dose IVIG out of reach of the common man in India. A study by Mangla et al. has proposed low-dose IVIG (0.05 - 0.1 g/kg/day for 5 days) to be a safe and effective treatment option in children. [4] Viard et al. found benefit with IVIG in a dose as low as 0.8 g/kg. [1] The dose used by us was a cumulative dose of 0.2-0.5 g/kg divided over 3 days and the approximate cost incurred by the patient was between Rs. 18,000-30,000 in contrast to approximately Rs. 1.5-2 lakh, which is the average cost of the high-dose regimen.
Based on the SCORTEN predicted mortality rate analysis, our study showed that the combination therapy significantly reduced the mortality rates. Steroids alone also reduced mortality, but not as significantly as in combination. Moreover, the combination therapy arrested the disease progression earlier than corticosteroids. The onset of epithelization was also faster. This indicates that corticosteroids could be tapered earlier and the total steroid dose could be reduced. Finally, it is also noteworthy that no serious adverse effects of either treatment modality were found in any of our patients.
We are not unaware of the limitations of our study. In view of the rarity of the disease and the small sample size expected, we did not go for a randomized study design. Also histopathological confirmation of all cases could not be performed. We intend for our study to be taken as a pilot project and hope that more researchers will conduct further elaborate trials to confirm or refute our findings.
In conclusion, our study supports the use of combination therapy with low dose IVIG and steroids in TEN. Even though treatment with steroids alone also has a definite role, our study indicates that combination therapy has a superior therapeutic effect when compared to steroids alone. As similar studies are lacking in the literature, more multi-centric randomized controlled trials are needed to confirm the findings of this study.
| 1. |
Viard I, Wehrli P, Bullani R, Schneider P, Holler N, Salomon D, et al. Inhibition of toxic epidermal necrolysis by blockade of CD95 with human intravenous immunoglobulin. Science 1998;282:490-3.
[Google Scholar]
|
| 2. |
Pereira FA, Mudgil AV, Rosmarin DM. Toxic epidermal necrolysis. J Am Acad Dermatol 2007;56:181-200.
[Google Scholar]
|
| 3. |
Smith DI, Swamy PM, Heffernan MP. Off-label uses of biologics in dermatology: Interferon and intravenous immunoglobulin (part 1 of 2). J Am Acad Dermatol 2007;56:e1-54.
[Google Scholar]
|
| 4. |
Mangla K, Rastogi S, Goyal P, Solanki RB, Rawal RC. Efficacy of low dose intravenous immunoglobulins in children with toxic epidermal necrolysis: An open uncontrolled study. Indian J Dermatol Venereol Leprol 2005;71:398-400.
[Google Scholar]
|
| 5. |
Habib A, Pasha W, Raza N. Treatment of toxic epidermal necrolysis (TEN) with low dose intravenous immunoglobulin in child. J Coll Physicians Surg Pak 2010;20:205-7.
[Google Scholar]
|
| 6. |
Tantikul C, Dhana N, Jongjarearnprasert K, Visitsunthorn N, Vichyanond P, Jirapongsananuruk O. The utility of the World Health Organization-The Uppsala Monitoring Centre (WHO-UMC) system for the assessment of adverse drug reactions in hospitalized children. Asian Pac J Allergy Immunol 2008;26:77-82.
[Google Scholar]
|
| 7. |
Bastuji-Garin S, Rzany B, Stern RS, Shear NH, Naldi L, Roujeau JC. Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol 1993;129:92-6.
[Google Scholar]
|
| 8. |
Bastuji-Garin S, Fouchard N, Bertocchi M, Roujeau JC, Revuz J, Wolkenstein P. SCORTEN: A severity-of-illness score for toxic epidermal necrolysis. J Invest Dermatol 2000;115:149-53.
[Google Scholar]
|
| 9. |
Kardaun SH, Jonkman MF. Dexamethasone pulse therapy for Stevens-Johnson syndrome/toxic epidermal necrolysis. Acta Derm Venereol 2007;87:144-8.
[Google Scholar]
|
| 10. |
Pasricha JS. Corticosteroids in toxic epidermal necrolysis. Indian J Dermatol Venereol Leprol 2008;74:493.
[Google Scholar]
|
| 11. |
Dhar S. Systemic corticosteroids in toxic epidermal necrolysis. Indian J Dermatol Venereol Leprol 1996;62:270-1.
[Google Scholar]
|
| 12. |
Sharma VK. Guidelines for Stevens Johnson syndrome and Toxic epidermal Necrolysis, and Psoriasis. Delhi: Therapeutic Guidelines Committee IADVL; 2007. p. 7-19.
[Google Scholar]
|
| 13. |
Rütter A, Luger TA. High-dose intravenous immunoglobulins: An approach to treat severe immune-mediated and autoimmune diseases of the skin. J Am Acad Dermatol 2001;44:1010-24.
[Google Scholar]
|
| 14. |
Metry DW, Jung P, Levy ML. Use of intravenous immunoglobulin in children with stevens-johnson syndrome and toxic epidermal necrolysis: Seven cases and review of the literature. Pediatrics 2003;112:1430-6.
[Google Scholar]
|
| 15. |
Tristani-Firouzi P, Petersen MJ, Saffle JR, Morris SE, Zone JJ. Treatment of toxic epidermal necrolysis with intravenous immunoglobulin in children. J Am Acad Dermatol 2002;47:548-52.
[Google Scholar]
|
| 16. |
Brown KM, Silver GM, Halerz M, Walaszek P, Sandroni A, Gamelli RL. Toxic epidermal necrolysis: Does immunoglobulin make a difference? J Burn Care Rehabil 2004;25:81-8.
[Google Scholar]
|
| 17. |
Schneck J, Fagot JP, Sekula P, Sassolas B, Roujeau JC, Mockenhaupt M. Effects of treatments on the mortality of Stevens-Johnson syndrome and toxic epidermal necrolysis: A retrospective study on patients included in the prospective EuroSCAR Study. J Am Acad Dermatol 2008;58:33-40.
[Google Scholar]
|
| 18. |
Yang Y, Xu J, Li F, Zhu X. Combination therapy of intravenous immunoglobulin and corticosteroid in the treatment of toxic epidermal necrolysis and Stevens-Johnson syndrome: A retrospective comparative study in China. Int J Dermatol 2009;48:1122-8.
[Google Scholar]
|
| 19. |
Chen J, Wang B, Zeng Y, Xu H. High-dose intravenous immunoglobulins in the treatment of Stevens-Johnson syndrome and toxic epidermal necrolysis in Chinese patients: A retrospective study of 82 cases. Eur J Dermatol 2010;20:743-7.
[Google Scholar]
|
Fulltext Views
5,299
PDF downloads
1,810





