Translate this page into:
Malassezia furfur onychomycosis in an immunosuppressed liver transplant recipient
Correspondence Address:
Ilgen Ertam
Ege University Medical Faculty Department of Dermatology, 35040 Bornova-Izmir
Turkey
| How to cite this article: Ertam I, Aytimur D, Alper S. Malassezia furfur onychomycosis in an immunosuppressed liver transplant recipient. Indian J Dermatol Venereol Leprol 2007;73:425-426 |
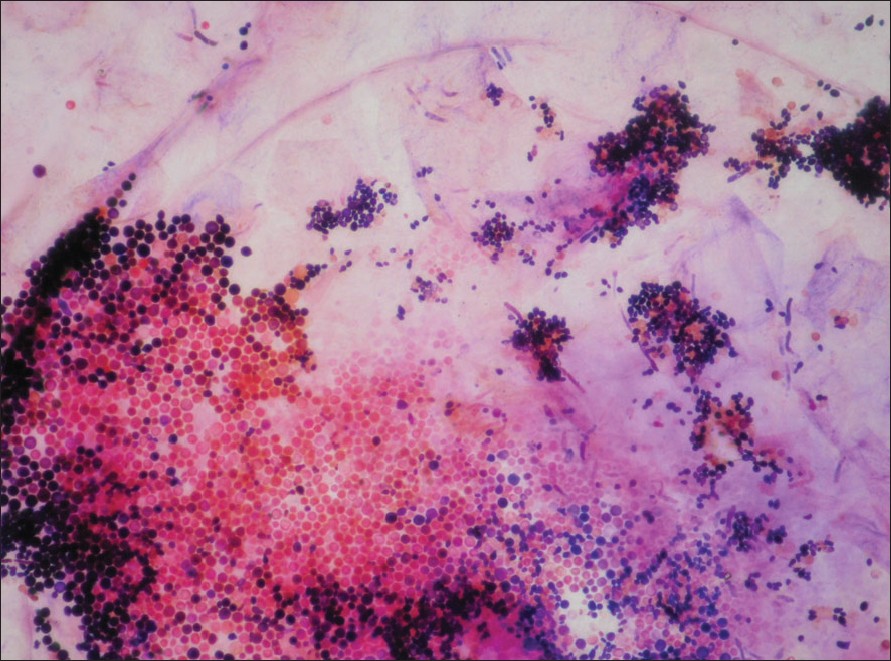 |
| Figure 2: Clusters of yeast cells of Malassezia furfur in culture |
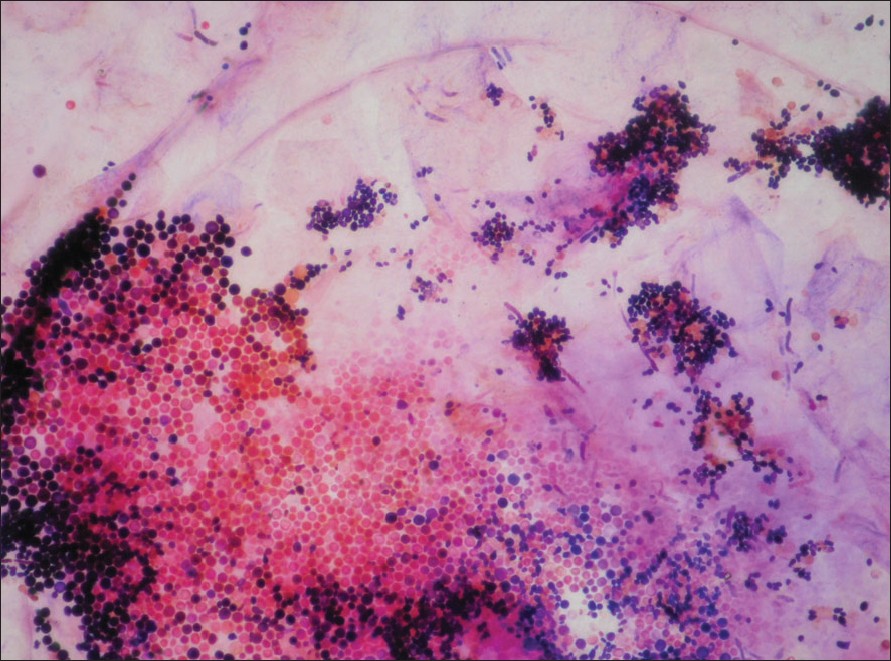 |
| Figure 2: Clusters of yeast cells of Malassezia furfur in culture |
 |
| Figure 1: Subungual hyperkeratosis and onycholysis of toe nails |
 |
| Figure 1: Subungual hyperkeratosis and onycholysis of toe nails |
Sir, It has been asserted that Malassezia spp . may be associated with seborrheic dermatitis, pityriasis versicolor, atopic dermatitis, psoriasis and confluent and reticular papillomatosis. [1] It is debatable whether Malassezia spp . is a real onychomycosis agent or a colonizer. In the literature, there are limited number of reports of onychomycosis cases in which Malassezia spp. is claimed as the agent. [2],[3] Malassezia furfur (M. furfur) isolated in toe nails of a liver transplant patient is presented here.
A 55 year-old male patient consulted us with a complaint of thickness in his toe nails for three months. The patient had had no previous onychomycosis treatment. He was undergoing therapy with multiple immunosuppressive agents for a liver transplant that he had undergone a year ago because of Hepatitis B virus (HBV)-related liver cirrhosis. In the examination of the toe nails, distal-lateral subungual hyperkeratosis and brown discoloration were detected in all of his toe nails. Periungual skin was normal [Figure - 1]. His skin and finger nails were normal.
Alcohol was used to remove the normal flora before the nail scrapings were taken. A cluster of yeast cells and short irregular hyphae were observed in the direct microscopic examination. They were incubated in Sabouraud and modified Dixon agar at 31° C for two weeks. The colonies that were grown showed round and spherical spore groups and short hyphae [Figure - 2]. They were also incubated in Tween 20-80. The organism, Malassezia furfur was identified by its morphological features and physiological tests, including catalase reaction, Tween assimilation test and splitting of esculin. Corn meal agar was used to differentiate from Candida spp . There were no findings related to dermatophytic and nondermatophytic fungi, either direct microscopic or stained preparate examination. Topical ciclopirox olamine nail solution was prescribed to the patient as treatment. Complete resolution was achieved after eight months of therapy.
Malassezia spp . is a lipophilic yeast that is a member of the normal flora found on the skin of warm-blooded animals. It can lead to disease if there is degeneration of skin structure and immunosuppression. Nine different species of Malassezia spp . were defined recently. [1],[3] Among these species, Malassezia furfur is an , oval, lipophilic yeast which is thought to play a role in the causation of the following conditions: pityriasis versicolor, seborrheic dermatitis, atopic dermatitis, Malassezia folliculitis, confluent and reticulate papillomatosis, otitis, onychomycosis and neonatal pustulosis. [1]
Although most of the cases of onychomycosis are caused by dermatophytes, there have been several literature reports [2],[4],[5] of patients with onychomycosis from whom Malassezia has been isolated. Yeasts lack keratolytic ability and do not normally colonize nails, as they are not a good source of lipids. There are conflicting reports as to whether Malassezia is a real pathogenic agent. [2],[3],[4],[5]
Chowdhary et al. , isolated Malassezia furfur from the nail scrapings obtained from the nail lesions of distal and lateral onycholysis with subungual hyperkeratosis on the hands and feet of a 13 year-old male patient. [2] Crespo-Erchiga et al. , asserted that they encountered Malassezia spp . with Candida spp . as subungual flora elements. Thus, because of its low incidence in the subungual debris, they contested the claim that Malassezia, is a true agent in onychomycosis. [3]
Existence of Malassezia in the subungual debris is important, particularly because it serves as a source of systemic infections in intensive care units and is contagious. [1] It is therefore imperative that patients who receive immunosuppressive therapy should be carefully evaluated for their initial nail findings and subsequent, direct examination and culture of the nails.
In our case, neither dermatophytic nor nondermatophytic mold invasion was detected in foot nail scraping samples. We assume that M. furfur was the etiological agent in our case because no other agent grew in culture.
| 1. |
Gupta AK, Batra R, Bluhm R, Boekhout T, Dawson TL. Skin diseases associated with Malassezia species. J Am Acad Dermatol 2004;51:785-98.
[Google Scholar]
|
| 2. |
Chowdhary A, Randhawa HS, Sharma S, Brandt ME, Kumar S. Malassezia furfur in a case of onychomycosis: Colonizer or etiologic agent? Med Mycol 2005;43:87-90.
[Google Scholar]
|
| 3. |
Crespo-Erchiga V, Florencio VD. Malassezia species in skin diseases. Curr Opin Infect Dis 2002;15:133-42.
[Google Scholar]
|
| 4. |
Silva V, Noreno GA, Zaror L, De-Oliveira E, Fischman O. Isolation of Malassezia furfur from patients with onychomycosis. J Med Vet Mycol 1997;35:73-4.
[Google Scholar]
|
| 5. |
Crozier WJ, Wise KA. Onychomycosis due to Pityrosporum. Australas J Dermatol 1993;34:109-12.
[Google Scholar]
|
Fulltext Views
3,690
PDF downloads
2,420





