Translate this page into:
Metastasizing squamous cell carcinoma arising from chronic discoid lupus erythematosus plaque of recent onset
2 Department of Pathology, Government Medical College and Hospital, Sector 32, Chandigarh, India
Correspondence Address:
Mandeep Dhingra
Department of Dermatology, B Block, Government Medical College and Hospital, Sector 32, Chandigarh - 160030
India
| How to cite this article: Dhingra M, Bhalla M, Thami GP, Mittal P. Metastasizing squamous cell carcinoma arising from chronic discoid lupus erythematosus plaque of recent onset. Indian J Dermatol Venereol Leprol 2011;77:626 |
Sir,
Squamous cell carcinoma (SCC) is a well-recognized, long-term complication of chronic discoid lupus erythematosus (CDLE). Hypertrophic lupus erythematosus (HLE) is a distinct variant of CDLE characterized by its chronic course, sometimes destructive scarring, and poor response to treatment. In the present communication, we describe a case of rapid malignant transformation in a CDLE plaque of recent onset over the upper lip, which was initially diagnosed as HLE.
A 36-year-old housewife from North India, a known case of CDLE for last 2 years, presented with a single asymptomatic, slowly progressive, warty lesion over the upper lip since 1 year. There was no history of fever, photosensitivity, joint pain or Raynaud′s phenomenon. Cutaneous examination revealed a large, verrucous, non-adherent plaque, 3 Χ 6 cm, involving right side of the upper lip and extending across the midline and into the oral mucosa [Figure - 1]a, along with multiple, discrete, scaly, erythematous plaques with central atrophy over the face, V area of neck, upper back and arms. Histopathologic examination of the lip lesion did not reveal any signs of malignancy [Figure - 1]b and was provisionally diagnosed as HLE. Haemogram showed anemia. Chest X-ray, electrocardiogram and urine examination were within normal limits. Antinuclear antibody (ANA) and anti-dsDNA tests were negative. Therapy with hydroxychloroquine and topical steroids along with intralesional steroids over the verrucous lesion was initiated. As the lip lesion reduced in size over the next 11 months, surgical debulking was done for cosmetic reasons. Other lesions responded favorably to therapy.
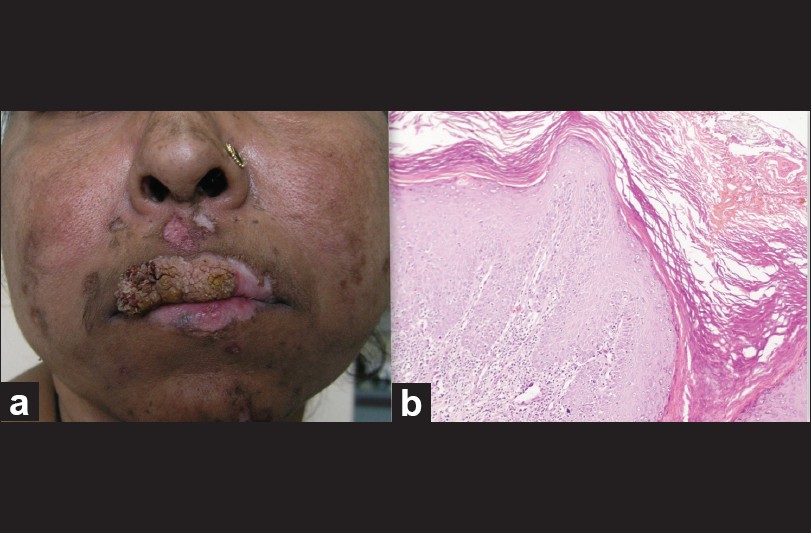 |
| Figure 1: (a) A large verrucous plaque, 3 × 6 cm, approximately involving right side of the upper lip and also extending across the midline. (b) Marked hyperkeratosis, papillomatosis, focus of follicular plugging and vacuolar degeneration of basal cell layer. The papillary dermis shows lymphomononuclear cells (H and E, ×200) |
Within a month of excision, the patient developed a distinct growth over the debulked lesion, starting as a small nodule, which rapidly progressed to a large mass with central ulceration [Figure - 2]a. The nodule was tender, adherent to the underlying muscle and bled on touch. Right submandibular lymph nodes were enlarged, firm, mobile and non-tender. Histopathologic examination confirmed the diagnosis of poorly differentiated SCC [Figure - 2]b. Fine needle aspiration cytology from the lymph nodes showed malignant cells along with tissue necrosis. Surgical debulking was done and chemotherapy in the form of cisplatin and 5-flurouracil was started.
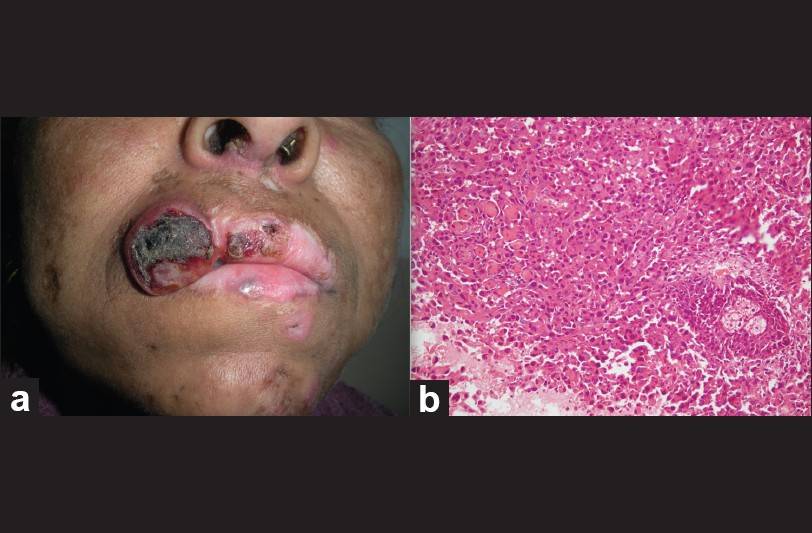 |
| Figure 2: (a) A single nodule measuring 2 × 2 cm, approximately arising from right lateral border of upper lip with area of central necrosis. (b) Anaplastic sheets of cells lying in the subepidermal soft tissues. Numerous mitotic figures are seen (H and E, ×200) |
CDLE lesions may develop malignant transformation; an incidence of 3.3% was reported by Millard and Barker, with a delay of 26-41 years (mean 30.8 years) between initiation of the CDLE and the appearance of SCC. [1] In another review of 10 African-American patients by Sherman et al., [2] it was observed that SCC in depigmented CDLE lesions occurred only in sun-exposed areas with a male predisposition and a history of CDLE for an average of approximately 18 years (range 7-30 years). Although the above-mentioned studies [1],[2] indicate a long latent period, Parikh et al. [3] have reported a case of SCC in a CDLE plaque over sun-protected area of only 1 year duration. In the present case, the SCC occurred after an interval of 3 years on photoexposed upper lip CDLE plaque with chronic scarring. Hence, a high index of suspicion is warranted in cases of CDLE even if the plaque is of recent onset, especially with risk factors like photoexposed area and chronic scarring.
Early SCC may be difficult to differentiate from HLE, posing a significant clinical as well as histopathologic dilemma. Eruption of nodules within heavily scarred areas of the scalp, lips and nose in association with bleeding and ulceration favor the development of SCC within the lesions of CDLE. [4] Histologically, pseudo-epitheliomatous hyperplasia may be a feature of HLE, and the distinction between this and SCC is important. The presence of predominantly lichenoid interface dermatitis, thickened basement membrane, and perivascular and periappendageal mononuclear infiltrate associated with epidermal hyperplasia may help in differentiating SCC from HLE. [4],[5] Presence of epidermal hyperplasia with atypical keratinocytes and breach of the basement membrane are characteristic of neoplasia. Immunoflourescence may also be helpful to differentiate between SCC and HLE. [4]
In the present case, it is very likely that the initial lesion diagnosed as HLE might have been early invasive SCC at the first instance which may not have been picked on histopathologic examination. Also, the presence of single lesion of HLE in a patient with so many classic CDLE lesions is unlikely. The rapid recurrence of lesions within 1 month after surgery again suggests that it may have been an early invasive SCC from the very onset. In retrospect, biopsies from multiple quadrants and histopathologic examination of the excised lesion might have helped.
This case has been presented to highlight that malignant transformation may occur even in a recent plaque of CDLE and also the diagnostic dilemma that verrucous lesions may pose in CDLE patients.
| 1. |
Millard LG, Barker DJ. Development of squamous cell carcinoma in chronic discoid lupus erythematosus. Clin Exp Dermatol 1978;3:161-6.
[Google Scholar]
|
| 2. |
Sherman RN, Lee CW, Flynn KJ. Cutaneous squamous cell carcinoma in black patients with chronic discoid lupus erythematosus. Int J Dermatol 1993;32:677-9.
[Google Scholar]
|
| 3. |
Parikh N, Choi J, Li M, Sharma R, Fernandez-Peñas P. Squamous cell carcinoma arising in a recent plaque of discoid lupus erythematous, in a sun-protected area. Lupus 2010;19:210-2.
[Google Scholar]
|
| 4. |
Vinciullo C. Hypertrophic lupus erythematosus: Differentiation from squamous cell carcinoma. Australas J Dermatol 1986;27:76-82.
[Google Scholar]
|
| 5. |
Daldon PE, Macedo de Souza E, Cintra ML. Hypertrophic lupus erythematosus: A clinicopathological study of 14 cases. J Cutan Pathol 2003;30:443-8.
[Google Scholar]
|
Fulltext Views
1,294
PDF downloads
836





