Translate this page into:
Multicentric calcified trichilemmal cysts with alopecia universalis affecting siblings
Correspondence Address:
Haneef N Sadath
7/202, Kalyani, Sahara States, LB Nagar, Hyderabad-500 068
India
| How to cite this article: Sadath HN, Ramachandra S, Kumar MA, Haritha K. Multicentric calcified trichilemmal cysts with alopecia universalis affecting siblings. Indian J Dermatol Venereol Leprol 2013;79:88-91 |
Abstract
Trichilemmal cyst, also known as "pilar cyst," is a benign cyst containing keratin and its breakdown products with a wall resembling external root sheath of hair. It occurs mostly in females as a solitary firm nodule over scalp. Occurrence of multiple trichilemmal cysts in areas other than scalp is extremely rare. We are reporting a case of a 40-years-old female who presented with multiple calcified trichilemmal cysts in multicentric distribution associated with alopecia universalis. Similar complaints were present in elder sister of the patient, indicating a genetic background. Multicentric distribution of trichilemmal cysts, calcification, familial occurrence, and association with alopecia universalis seen in our case are all rare and intriguing features.Introduction
Trichilemmal cyst, also known as "pilar cyst," is a benign cyst containing keratin and its breakdown products with a wall resembling external root sheath of hair. [1] It is a relatively common condition, occurring predominantly in middle-aged females. It can be familial and may be associated with autosomal-dominant inheritance. [2] It presents as asymptomatic or mildly painful, solitary, smooth, mobile, firm nodule, mainly over scalp. [3] Occasionally, other hair bearing sites such as neck, trunk, limbs, or groin may be affected. [4] Multiple trichilemmal cysts are known to occur within the scalp, but occurrence in a multicentric distribution is extremely rare. [5] One such rare case of multicentric trichilemmal cysts associated with dystrophic calcification and familial occurrence is reported here and the literature reviewed.
Case Report
A 40-years-old female labourer presented with multiple, yellowish white, raised, solid skin lesions over scalp, both forearms, and buttocks since 20 years. The lesions initially appeared over buttocks and then spread to scalp and forearms over a period of 2 years. The lesions were largely asymptomatic, though mild pain and itching were perceived at times. Some lesions were associated with chalky white discharge for past 2 years. The discharge was non-foul smelling and not blood-tinged. There was sudden onset loss of hair all over the body at the age of 10 years. Hair growth was apparently normal before the age of 10 years. There was history of similar skin lesions and loss of hair in sister of the patient, who was 3 years elder to the index patient. The elder sister died 1 year ago due to pneumonia. There were no other siblings. Both the index patient and sibling were non-diabetic.
Cutaneous examination showed multiple, 2 mm - 2 cm sized, skin-colored to yellowish cysts along with firm to hard papules and nodules on scalp, extensor aspect of forearms, elbows, and gluteal region [Figure - 1] and [Figure - 2]. Few larger (up to 4 cm), tender nodules and cysts with occasional white pultaceous discharge were seen over gluteal region and left thigh [Figure - 3]. Mucosae, palms, and soles were not involved. There was non-scarring loss of hair all over the body including scalp, eyebrows, eyelashes, axillary, and pubic hair [Figure - 1]. Nails were normal. General physical and systemic examination was unremarkable.
 |
| Figure 1: Multiple, skin colored to yellowish cysts, firm to hard papules and nodules on scalp with non-cicatrical alopecia |
 |
| Figure 2: Multiple, skin colored to yellowish cysts, firm to hard papules and nodules on extensor aspect of forearm and elbow |
 |
| Figure 3: Few large (up to 4 cm), tender nodules and cysts with white pultaceous discharge over gluteal region |
Steatocystoma multiplex, xanthomatosis, trichilemmal cysts, calcinosis cutis, and trichoepithelioma were considered under differential diagnosis of the cysts. Various causes for diffuse hair loss like alopecia universalis, congenital atrichia with papular lesions, systemic lupus erythematosus, alopecia neoplastica (associated with breast cancer), and chemotherapy-induced alopecia were considered.
All routine investigations, biochemical parameters including lipid profile and serum calcium were normal. HIV was non-reactive. Histopathology of lesions over scalp and forearm showed dermal cystic lesions lined by stratified squamous epithelium undergoing abrupt keratinization with no evident granular layer (trichilemmal keratinization) along with palisading of basal layer [Figure - 4]. These features are characteristic of trichilemmal cyst. Biopsy of lesions over gluteal region showed sub-epidermal cystic masses of calcium deposits surrounded by histiocytes and multinucleated giant cells of foreign body type [Figure - 5]. These features were suggestive of dystrophic calcinosis within the trichilemmal cysts.
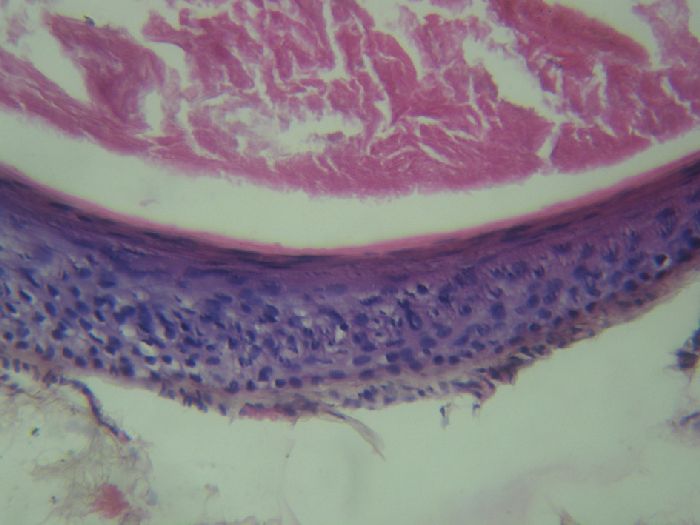 |
| Figure 4: Cyst wall epithelium undergoing abrupt keratinization with no evident granular layer - "trichilemmal keratinization" (H and E, 40X) |
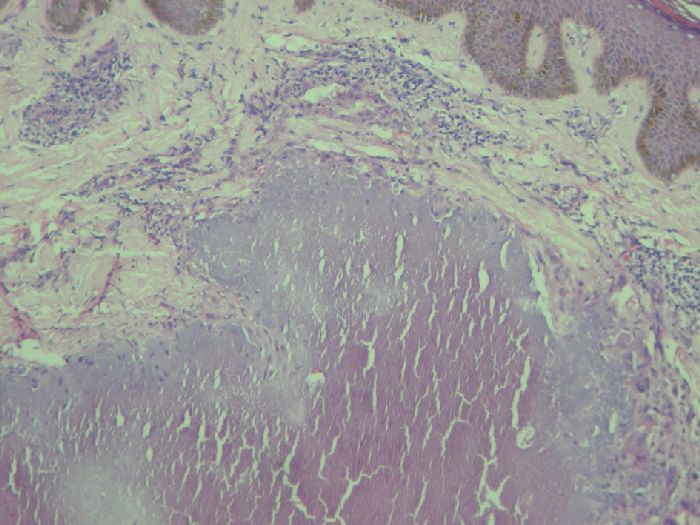 |
| Figure 5: Subepidermal cystic masses of calcium deposits surrounded by histiocytes and multinucleated giant cells (H and E, 10X) |
Based on the clinical and histopathological features, a final diagnosis of multicentric, calcified trichilemmal cysts with alopecia universalis was made. Surgical excision of larger lesions was carried out to provide relief to the patient. Patient was not willing for treatment of alopecia after understanding the prognosis of the same.
Discussion
Trichilemmal cyst is a benign cyst containing keratin and its breakdown products with a wall showing characteristic trichilemmal keratinization (absent granular layer). [1] It is commonly seen in middle-aged females, sometimes with autosomal-dominant inheritance. [2] It occurs mainly over scalp. [3] Occasionally, other hair bearing sites such as neck, trunk, limbs, or groin may be affected. [4] There are anecdotal reports of finger pulp, vulval, and intra-oral involvement also. [6],[7] Sometimes, rapidly multiplying trichilemmal cyst called as "proliferating trichilemmal cyst" can be seen. Usually, it is benign but may become malignant very rarely. A case of multiple trichilemmal cysts following Blaschko′s lines and associated with filiform hyperkeratosis and referred to as trichilemmal cyst nevus (nevus trichilemmocysticus) has been published. [8]
Multiple trichilemmal cysts are known to occur within the scalp, but occurrence in a multicentric distribution affecting areas other than scalp is extremely rare. [5] Our patient reported here showed multiple trichilemmal cysts of varying sizes, both over the scalp as well as other sites, namely upper limbs, gluteal region, and thighs. Also, some lesions had gradually grown to a size of up to 4 cm with development of calcinosis cutis (dystrophic calcification), with an occasional discharge of the calcific material. Calcification in trichilemmal cysts is very rarely reported. [9]
The patient had diffuse non-scarring alopecia all over the body including scalp, eyebrows, eyelashes, axillary, and pubic hair since early childhood. Based on the typical clinical features, we diagnosed it as alopecia universalis, though histopathology features were inconclusive. Alopecia universalis is known to persist into late adulthood, especially if the onset is in childhood, as in our case. [10] Diffuse alopecia similar to alopecia universalis along with milia or keratinous cysts are known to occur in "congenital atrichia with papular lesions." [11] But, here alopecia occurs soon after birth, and occurrence of trichilemmal cysts is not described. Moreover, there are additional diagnostic features for this condition like whitish streaks over scalp, which were not seen in our case. Trichilemmal cysts have been earlier reported in association with leukonychia and ciliary dystrophy (FLOTCH syndrome), glomus tumor, melanocytic nevus, and nevus sebaceous, but no case in association with alopecia universalis has been described earlier. [12],[13]
Patient′s elder sister also had skin swellings as well as loss of hair, apparently similar to the index patient, indicating a genetic background. Exact pattern of inheritance could not be ascertained, since the patient was not sure about involvement of other members of her family tree. But familial cases of trichilemmal cysts are known to occur with autosomal-dominant inheritance. [2],[9],[14] A genetic background can be further supported by presence of trichilemmal cysts in FLOTCH syndrome, their association with Gardner syndrome and nevoid occurrence in some cases. [12],[15],[16] The candidate gene is still not known. But Eiberg et al. mapped a probable locus for a candidate gene ′TRICY1′ (for trichilemmal cysts) on chromosome 3p24-p21.2. [14]
Friedel et al. reported F amilial occurrence of total L euk O nychia, T richilemmal cysts, C iliary (eyelash) dystrophy with dominant autosomal Heredity as FLOTCH syndrome. [12] Leukonychia was seen from infancy or early childhood itself in the previously reported cases of FLOTCH syndrome. [15] Our patient did not have leukonychia even at the age of 40 years. Presence or absence of leukonychia in the deceased sibling of the patient could not be confirmed. But, presence of trichilemmal cysts and alopecia universalis with possible genetic background makes our case very intriguing, as this may be a variant of FLOTCH syndrome. Abnormal keratinization has been hypothesized as a mechanism for occurrence of trichilemmal cysts and leukonychia in FLOTCH syndrome. [15] Whether the association of trichilemmal cysts and generalized alopecia in our case has a similar pathological link or is a chance association needs to be explored. We hope this rare case report throws more light on understanding the etiopathogenesis of trichilemmal cyst.
| 1. |
McGavran MH, Binnington B. Keratinous cysts of the skin. Identification and differentiation of pilar cysts from epidermal cysts. Arch Dermatol 1966;94:499-508.
[Google Scholar]
|
| 2. |
Leppard BJ, Sanderson KV, Wells RS. Hereditary trichilemmal cysts: Hereditary pilar cysts. Clin Exp Dermatol 1977;2:23-32.
[Google Scholar]
|
| 3. |
Kavak A, Aydogan I, Alper M. Shall we add trichilemmal cyst to painful skin tumours? J Eur Acad Dermatol Venereol 2006;20:238.
[Google Scholar]
|
| 4. |
Nakamura S, Nakayama K, Ito F, Hoshi K. A case of trichilemmal cyst on the leg. J Dermatol 1987;14:178-9.
[Google Scholar]
|
| 5. |
Hendricks DL, Liang MD, Borochovitz D, Miller T. A case of multiple pilar tumors and pilar cysts involving the scalp and back. Plast Reconstr Surg 1991;87:763-7.
[Google Scholar]
|
| 6. |
Ikegami T, Kameyama M, Orikasa H, Yamazaki K. Trichilemmal cyst in the pulp of the index finger: A case report. Hand Surg 2003;8:253-5.
[Google Scholar]
|
| 7. |
Perez LM, Bruce JW, Murrah VA. Trichilemmal cyst of the upper lip. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;84:58-60.
[Google Scholar]
|
| 8. |
Tantcheva-Poor I, Reinhold K, Krieg T, Happle R. Trichilemmal cyst nevus: A new complex organoid epidermal nevus. J Am Acad Dermatol 2007;57:S72-7.
[Google Scholar]
|
| 9. |
Mommers XA, Henault B, Aubriot MH, Trost O, Malka G, Zwetyenga N. Multiple ossifying trichilemmal cysts of the scalp: A familial case. Rev Stomatol Chir Maxillofac 2012;113:53-6.
[Google Scholar]
|
| 10. |
Anderson I. Alopecia areata: A clinical study. Br Med J 1950;2:1250-2.
[Google Scholar]
|
| 11. |
Thomas M, Daniel S. Atrichia congenita with papular lesions. Indian J Dermatol Venereol Leprol 2011;77:70-2.
[Google Scholar]
|
| 12. |
Friedel J, Heid E, Grosshans E. The FLOTCH syndrome. Familial occurrence of total LeukOnychia, Trichilemmal cysts and Ciliary dystrophy with dominant autosomal Heredity. Ann Dermatol Venereol 1986;113:549-53.
[Google Scholar]
|
| 13. |
Rahbari H, Mehregan AH. Development of proliferating trichilemmal cyst in organoid nevus. Presentation of two cases. J Am Acad Dermatol 1986;14:123-6.
[Google Scholar]
|
| 14. |
Eiberg H, Hansen L, Hansen C, Mohr J, Teglbjaerg PS, Kjaer KW. Mapping of hereditary trichilemmal cyst (TRICY1) to chromosome 3p24-p21.2 and exclusion of beta-CATENIN and MLH1. Am J Med Genet A 2005;133:44-7.
[Google Scholar]
|
| 15. |
Rodríguez-Lojo R, Del Pozo J, Sacristán F, Barja J, Piñeyro-Molina F, Pérez-Varela L. Leukonychia totalis associated with multiple pilar cysts: Report of a five-generation family: FLOTCH syndrome? Eur J Dermatol 2011;21:484-6.
[Google Scholar]
|
| 16. |
Larralde M, Boggio P, Abad ME, Corbella C, Happle R. Nevus trichilemmocysticus: Report of a new case of a recently recognized entity. Pediatr Dermatol 2011;28:286-9.
[Google Scholar]
|
Fulltext Views
7,074
PDF downloads
1,516





