Translate this page into:
Multifocal tuberculous gummas and bilateral scrofuloderma followed by papulonecrotic tuberculids developing during anti-tubercular therapy
Correspondence Address:
Kinjal Deepak Rambhia
B-105, Kalpataru Classic, Chincholi Bunder Road, Malad West, Mumbai - 400 064, Maharashtra
India
| How to cite this article: Rambhia KD, Kharkar V, Mahajan S, Khopkar US. Multifocal tuberculous gummas and bilateral scrofuloderma followed by papulonecrotic tuberculids developing during anti-tubercular therapy. Indian J Dermatol Venereol Leprol 2016;82:424-426 |
Sir,
A 20-year-old man presented with multiple asymptomatic, reddish, raised and exudative lesions on the neck, chest and axillae for 9 years. He also had complaints of evening rise in temperature, weight loss and loss of appetite. Cutaneous examination revealed multiple, well-defined, erythematous, indurated plaques, some showing erosions with hemorrhagic crusts on the neck, trunk and axillae [Figure - 1]. Some plaques had advancing margins, while others showed pustules at the periphery. There were multiple discharging sinuses in the axillae and the cervical area. Multiple atrophic cord-like scars were noted on the neck and trunk. General examination showed pallor with signs of poor nutrition while the systemic examination was normal.
 |
| Figure 1: Multiple indurated plaques with erosions and hemorrhagic crusts on the neck and trunk |
Hematological and biochemical investigations were within normal limits except for reduced hemoglobin (6.9 g/dl), leukocytosis (18,100/μl) and raised erythrocyte sedimentation rate of 60 mm. Mantoux test was strongly positive with an induration of 52 mm at 48 h. Microscopic examination of sputum for acid-fast bacilli was negative. Culture for Mycobacterium tuberculosis on Lowenstein–Jensen medium did not reveal any growth. Enzyme-linked immunosorbent assay for human immunodeficiency virus and hepatitis B surface antigen were negative. Radiograph of the chest revealed bilateral parenchymal opacities. Fine-needle aspiration cytology of the axillary lymph nodes did not reveal acid-fast bacilli. High resolution computed tomography scan confirmed the presence of opacities in the lung. Ultrasonography of the abdomen was normal.
Skin biopsy from one of the discharging sinuses revealed well-defined granulomas with Langhans giant cells and lymphocytes involving the entire dermis. Taking into account these findings and the clinical picture, the lesions were suggestive of scrofuloderma [Figure - 2]. A biopsy from one of the plaque lesions revealed necrosis and tuberculoid granulomas with a variable mantle of lymphocytes in the dermis. Therefore, the patient was diagnosed to have multifocal tuberculous gummas with bilateral scrofuloderma. He was started on treatment with isoniazid, rifampicin, ethambutol and pyrazinamide for a period of 6 months. However, 3 weeks following the initiation of treatment, the patient developed multiple asymptomatic erythematous papules with central necrosis on the trunk [Figure - 3]a. Skin biopsy from the lesion revealed a wedge-shaped area of necrosis with a broad base toward the epidermis [Figure - 3]b. There were multiple epithelioid and Langhans giant cells surrounding the area of necrosis, suggesting a diagnosis of papulonecrotic tuberculid. Anti-tubercular treatment was continued and there was complete resolution of all the lesions at the end of treatment [Figure - 4].
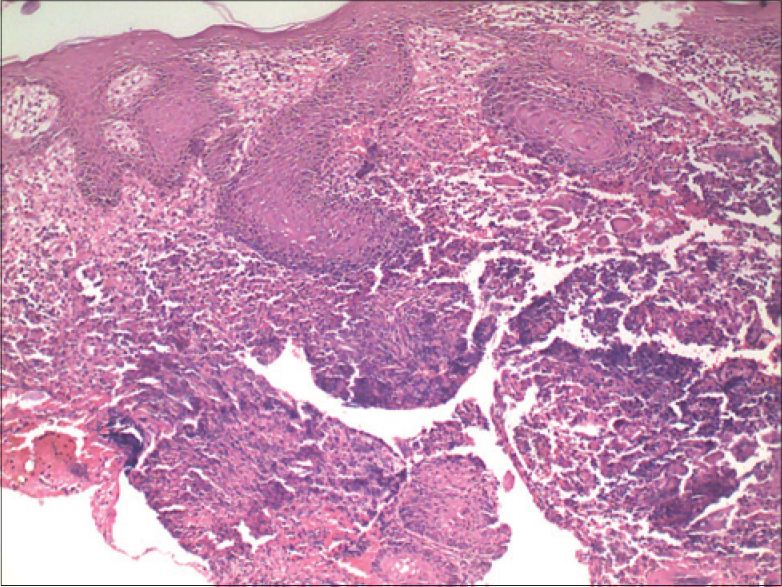 |
| Figure 2: Granuloma with Langhans giant cells and lymphocytes involving the entire dermis (H and E, ×400) |
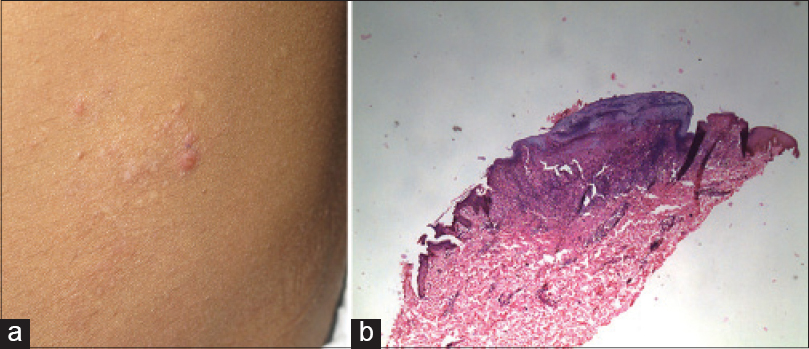 |
| Figure 3: (a) Erythematous papules with central necrosis on the trunk. (b) Wedge-shaped area of necrosis with a broad base toward the epidermis (H and E, ×100) |
 |
| Figure 4: Resolution of lesions with scarring following treatment |
Cutaneous tuberculosis can present with varied clinical manifestations which may be dependent on the route of infection (endogenous or exogenous), the immune status of the patient and previous sensitization with tuberculosis.[1] Tuberculous gummas, also called metastatic tuberculous abscesses, are usually seen in malnourished children and in immunocompromised states. They are the result of hematogenous dissemination of tubercle bacilli from an underlying focus and occur during periods of lowered immunity. The lesions may be single or multiple. Clinically, they appear as subcutaneous nodules or soft cold abscesses on the extremities or trunk. These gummas later evolve into ulcers with undermining edges or discharging sinuses. Scrofuloderma results from contiguous involvement of the skin overlying tuberculosis in a deeper structure (lymph node, bone, or joint). Clinically, it presents as a nodule which later breaks down to form discharging sinuses and progresses to form puckered scars. Tuberculids are thought to represent a response to the hematogenous spread of tubercle bacilli in patients with a better immune response against M. tuberculosis. They are characterized by a positive tuberculin test, evidence of current or past tuberculosis and a positive response to antituberculous therapy.
Co-existence of different types of cutaneous tuberculosis has been described; various authors have reported scrofuloderma with tuberculosis verrucosa cutis, lupus vulgaris with tuberculosis verrucosa cutis, papulonecrotic tuberculid with lichen scrofulosorum and lupus vulgaris with papulonecrotic tuberculid, with the time gap between the development of the forms ranging from simultaneous to 3 months and even 5 years.[2] Interestingly, this patient also developed papulonecrotic tuberculid in addition to scrofuloderma and multifocal tuberculous gummas.
The cause of multiplicity of lesions in this patient may be attributed to poor nutritional status, chronicity of the disease (9 years), hematogenous spread and lack of treatment for a long duration in the course of disease. It is known that fluctuations in the immunological state of the patient may determine the development and features of cutaneous tuberculosis. With initiation of specific treatment in patients with tuberculosis, there is an upgradation in immunity. In this patient, lesions of papulonecrotic tuberculid developed after initiation of anti-tubercular therapy which may have caused a favorable shift in cell-mediated immunity. A similar phenomenon of occurrence of lichen scrofulosorum after initiation of anti-tuberculous treatment has been reported previously.[3] Similarly, papulonecrotic tuberculid was also reported to occur in a patient with human immunodeficiency virus infection as a consequence of the increase in the CD4 T-lymphocyte count following the addition of a second antiretroviral drug.[4]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Yates VM. Mycobacterial infections. In: Burns T, Breathnach S, Cox N, Griffith C, editors. Rook's Textbook of Dermatology. 8th ed. Massachusettes: Wiley-Blackwell; 2010. p. 31.10
[Google Scholar]
|
| 2. |
Rao AG. Scrofuloderma associated with tuberculosis verrucosa cutis. Indian J Dermatol Venereol Leprol 2014;80:76-8.
[Google Scholar]
|
| 3. |
Smith NP, Ryan TJ, Sanderson KV, Sarkany I. Lichen scrofulosorum. A report of four cases. Br J Dermatol 1976;94:319-25.
[Google Scholar]
|
| 4. |
Alsina M, Campo P, Toll A, Martinez E, Palou J, Herrero C. Papulonecrotic tuberculide in a human immunodeficiency virus type 1-seropositive patient. Br J Dermatol 2000;143:232-3.
[Google Scholar]
|
Fulltext Views
5,487
PDF downloads
2,912





