Translate this page into:
Multiple cutaneous mastocytomas
2 Department of Pathology, Lady Hardinge Medical College and Associated Hospitals, New Delhi, India
Correspondence Address:
Taru Garg
Department of Dermatology, Venereology and Leprology, Lady Hardinge Medical College and Associated Hospitals, New Delhi - 110 001
India
| How to cite this article: Garg T, Chander R, Gaur N, Singh A, Nangia A. Multiple cutaneous mastocytomas . Indian J Dermatol Venereol Leprol 2014;80:547-549 |
Sir,
Cutaneous mastocytosis is defined by abnormal infiltration of mast cells limited to the skin. Urticaria pigmentosa and mastocytoma are the most common clinical types while diffuse cutaneous mastocytosis is a rare entity. Mastocytoma is a solitary nodular lesion which may be present at birth or appears within the first 3 months of life and resolves spontaneously with age. [1]
A 3-month-old boy presented with skin-colored raised lesions, progressively increasing in number and scattered all over the body noted a few hours after birth. He had history of multiple episodes of blistering within these raised skin lesions. There were no systemic complaints. Antenatal, birth and developmental history were normal.
On cutaneous examination, there were 11 discrete, well-defined, nodulo-plaques over face, trunk, and extremities [Figure - 1]. A few serous fluid-filled bullae were present on top of the lesions on the back. Darier′s sign was positive [Figure - 2]a. While the child was being evaluated as an in-patient, he started developing episodes of flushing, which lasted for 3-4 minutes [Figure - 2]b. These were not associated with hypotension or tachycardia.The child also developed two new lesions over the scalp.
 |
| Figure 1: Multiple nodulo-plaques, also showing bullae, at various sites |
 |
| Figure 2: (a) Darier's sign. (b) Generalized erythema during an episode of flushing |
The histopathological examination of one of the nodules revealed sheets of mast cells in the dermis [Figure - 3]a. On toluidine blue staining, intracellular metachromatic granules were seen [Figure - 3]b.
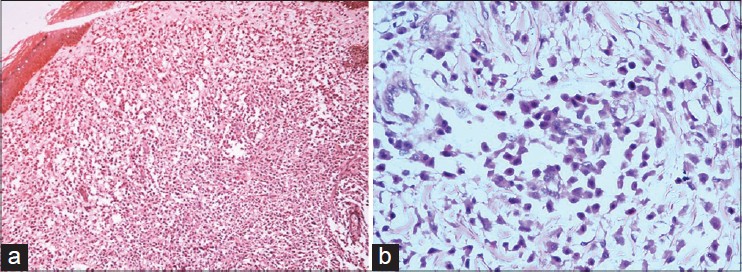 |
| Figure 3: (a) Sheets of mast cells in dermis (H and E, ×10), (b) Toludine blue stain showing mast cells with granular cytoplasm (×40) |
Hematological parameters were normal except for slightly low hemoglobin (11 gm/dl) and eosinophilia (absolute eosinophil count 500/microliter). His serum biochemistry was normal. Radiological investigations and bone marrow examination were normal.
The parents were advised regarding avoidance of potential triggers of mast cell degranulation. The child was treated with various oral H1 antihistamines (cetirizine, dexchlorpheniramine, promethazine, hydroxyzine). Fluticasone propionate 0.05% ointment application was advised over the nodules. No other drugs were started in view of the age of the child and the doubtful safety profile of mast cell stabilizers in children less than 2 years of age. The episodes of flushing became infrequent, no new lesions appeared, and there was some flattening of skin lesions after 3 months. Subsequently, the child was lost to follow-up.
A majority (65%) of patients with cutaneous mastocytosis present in childhood, among which, 55% do so before the age of 2. Mastocytomas are present in 10-35%. Most mastocytomas appear during the first year of life with around 42% presenting at birth. Vesiculation and bulla formation are observed in 33% of mastocytomas. [2] Our patient had multiple mastocytomas which is rare. [1]
Flushing occurs in 6.5% of patients and abdominal pain has also been described in cases with mastocytomas. Our patient experienced multiple episodes of flushing which were not associated with hypotension. Systemic symptoms are rare in pediatric cutaneous mastocytosis. These are seen more often in those with extensive skin involvement, episodes of flushing, early onset of disease and bullous lesions. These patients have a potential risk for experiencing shock or sudden death. [3]
Plasma tryptase and histamine concentrations reflect the increased proliferation of mast cells and/or their activation. [4] Bone marrow biopsy in those with childhood-onset cutaneous disease is not recommended unless there is evidence of systemic disease such as unexplained peripheral blood abnormalities, hepatosplenomegaly, and lymphadenopathy. [5] It has been suggested that a serum tryptase level exceeding 100 ng/ml or more is an indication for bone marrow examination regardless of age. [2] Due to monetary constraints, the plasma tryptase levels could not be done in our patient. As he had frequent flushing episodes, appearance of new skin lesions and multiple mastocytomas, bone marrow examination was carried out, which turned out to be normal.
The therapy for mastocytosis is focused on providing symptomatic relief and avoidance of triggering factors. H1 antihistamines control pruritus, flushing and urticaria. In spite of receiving antihistamines, our patient had, an initial, increase in the duration of flushing episodes. We assume that this was because triggering factors like friction could not be avoided due to the multiplicity of lesions.The other reason could be an inadequate dose of antihistamines due to lack of sufficient data on dosage in the very young. Sometimes, flushing can be caused by chemical mediators other than histamine.To add to the problem, the safety profile of drugs with mast cell stabilizing properties like ketotifen and azelastine in infants and the very young has not been established. [6] Surgical excision of solitary mastocytoma, topical calcineurin inhibitors and topical corticosteroids are among the other modalities of treatment.
The course of the disease in children is often benign and there is usually no progression to systemic disease. The occurence of multiple mastocytomas with bullous lesions as a presenting feature is unusual. The control of flushing in such an instance may be difficult. There is need for more therapeutic options and guidelines for the treatment of pediatric mastocytosis, especially in very young infants.
| 1. |
Lange M, Nedoszytko B, Górska A, Zawrocki A, Sobjanek M, Kozlowski D. Mastocytosis in children and adults: Clinical disease heterogeneity. Arch Med Sci 2012;8:533-41.
[Google Scholar]
|
| 2. |
Ben-Amitai D, Metzker A, Cohen HA. Paediatric cutaneous mastocytosis: A review of 180 Patients. Isr Med Assoc J 2005;7:320-2.
[Google Scholar]
|
| 3. |
Murphy M, Walsh D, Drumm B, Watson R. Bullous mastocytosis: A fatal outcome. Pediatr Dermatol 1999;16:452-5.
[Google Scholar]
|
| 4. |
Schwartz LB, Sakai K, Bradford TR, Ren SL, Zweiman B, Worobec AS, et al. The alpha form of human tryptase is the predominant type present in blood at baseline in normal subjects and is elevated in those with systemic mastocytosis. J Clin Invest 1995;96:2702-10.
[Google Scholar]
|
| 5. |
Kettelhut BV, Metcalfe DD. Plasma histamine concentrations in evaluation of pediatric mastocytosis. J Pediatr 1987;111:419-21.
[Google Scholar]
|
| 6. |
Carter MC, Metcalfe DD. Pediatric mastocytosis. Arch Dis Child 2002;86:315-9.
[Google Scholar]
|
Fulltext Views
3,316
PDF downloads
1,745





