Translate this page into:
Nail cosmetics
Correspondence Address:
Nina A Madnani
Department of Dermatology, P.D. Hinduja Hospital and MRC, Mumbai
India
| How to cite this article: Madnani NA, Khan KJ. Nail cosmetics. Indian J Dermatol Venereol Leprol 2012;78:309-317 |
Abstract
The nail as an anatomic structure protects the terminal phalanx of the digit from injury. Historically, it has served as a tool for protection and for survival. As civilizations developed, it attained the additional function of adornment. Nail beautification is a big industry today, with various nail cosmetics available, ranging from nail hardeners, polishes, extensions, artificial/sculpted nails, and nail decorations. Adverse events may occur either during the nail-grooming procedure or as a reaction to the individual components of the nail cosmetics. This holds true for both the client and the nail technician. Typically, any of the procedures involves several steps and a series of products. Separate "nail-bars" have been set up dedicated to serve women and men interested in nail beautification. This article attempts to comprehensively inform and educate the dermatologist on the services offered, the products used, and the possible/potential adverse effects related to nail-grooming and nail cosmetics.Introduction
The earliest use of nail coloring dates back to ancient Egypt and China. The first nail polish was made from egg white, flowers, and wax. Natural henna was also used as a nail colorant. Specific colors like red, gold, and silver were chosen for royalty, and the common folk had to use lighter shades. In ancient China, gold and silver represented royalty. While red and black represented strength and boldness, pale colors denoted feebleness. Artificial nails date back as far as 600 BC to the Chou dynasty in China, where nails were made from gold, silver, and precious stones. [1]
Modern day nail polish was formulated in 1920 by the Charles Revson Company, which today is known as Revlon. They were inspired by the enamel paint used on cars to formulate something similar for the nails. The modern day nail polish became commercially available in 1932.
What is An Attractive Nail ?
Attractiveness of a nail is a subjective phenomenon. A nail is generally considered aesthetically pleasing if it has:
- A smooth glossy surface.
- No overhanging or ragged cuticle.
- A tip extending beyond the nail.
- An oval contour to the nail plate.
- A gentle curve when visualized from the side.
- Translucency so that the pink nail bed is clearly visualized.
The beauty of the nail can be further enhanced using various shades and colors of nail polish.
The most popular nail-grooming procedure is known as a manicure (for fingernails) and pedicure (for toenails).
Steps of A Manicure/Pedicure
Prior to applying the nail polish, the hands/feet and nails undergo the following:
- The previous polish is cleaned off with a chemical remover and the nails are cut to the required length with nail cutters or clippers.
- The hands/feet are soaked in warm water with a mild detergent to soften the nail plate and cuticle and to remove any dirt or grease from the surface.
- A foot scraper or a pumice stone is used to buff away any rough skin or thick callus.
- A cuticle softener (alkaline substances like 0.4% sodium and potassium hydroxide) is applied to the cuticles for 5-10 min. They dissolve the di-sulfide keratin bridges.
- The cuticle is pushed back with a specially designed metallic or wooden stick, and then trimmed off with a cuticle cutter.
- The surface of the nail is buffed with an emery board to smoothen any ridges.
- The hands/feet are rinsed and dried, and an emollient cream is massaged to soften the skin and trap moisture into the nail plate.
- The cream is cleaned off from the nail plate.
Now, the nails are considered suitable for nail polish application.
The ideal nail polish application procedure includes three layers:
- Base coat: This is the first layer to be applied. It is transparent with a strong adhering capability due to higher resin content. It protects the nail plate from staining.
- Nail polish: A plethora of colors are available, with or without a metallic finish. The expertise of the nail technician provides various styles of nail polish application, of which the "French nail manicure" is very popular.
- Top coat: This transparent layer contains more of nitrocellulose and less resin, so as to protect the varnish from chipping.
Each product is applied consecutively with a 10-min gap in between applications [Figure - 1].
 |
| Figure 1: Bright-colored nail polish adds to the beauty of the hand |
Nail Polish/Varnish/Paint
Nail polish serves the purpose of:
- Beautification.
- Strengthening weak brittle nails.
- Camouflaging surface irregularities or discolorations. It can provide a youthful appearance to aged ridged nails. [2]
Nail polish is a complex combination of:
- Film-forming agents (most commonly, nitrocellulose).
- Resins (e.g., tosylamide-formaldehyde) for adherence.
- Plasticizers (e.g., dibutyl pthalate) for flexibility.
- Solvents (butyl stearate and acetate compounds) for keeping the polish in fluid state and to help in quick-drying once applied.
- Thixotropic agents (e.g., bentonite) for keeping the ingredients uniformly suspended.
- Various mineral pigments (calcium carbonate, zinc oxide, titanium dioxide, iron oxides), synthetic pigments (D and C red 6/7/19, FDC yellow).
- Natural agents (guanine, bismuth, oxychloride, and micatitanium) for the color and shine of the nail polish.
Hypoallergenic Nail Polish
The most common allergen in nail polish is tosylamide formaldehyde resin (TSFR). Because of growing awareness, "toxin-free" nail polish is getting popular. This variety contains cellulose, acetate, butyrate, and polyester resin, [3] with plasticizers such as dibutyl phthalate for softness and pliability, dissolved in solvents (N-butyl acetate or ethyl acetate). Some manufacturers claim to have "toxic-free nail polish," which is free of toluene, pthalate, and formaldehyde and contains natural pigments in a water base. Argan oil, which has a high content of amino acids, has also been used as an important ingredient.
Nail Hardeners
These are applied as a base coat for the purpose of strengthening the nail plate. They may contain titanium-silicone-zirconium polymers, polytef, nylon, calcium, and biotin. [4] Those containing formaldehyde may cause paronychia and irritant dermatitis, and are not in common use anymore. Nail hardeners need to be cleaned off every 2-3 days to prevent onycholysis and chromonychia. [5]
Nail Polish Remover
With the innumerable color choices available, nail polish is constantly changed to suit women′s moods and clothes. This involves cleaning off the existing one with removers. The following varieties are available:
- Acetone - the most commonly available. It has been reported to cause an irritant dermatitis.
- Acetone-free nail polish removers containing ethyl acetate, butyl acetate, or ethyl lactate.
- Nail polish remover pads containing gammabutyrolactone, which are safe and convenient to use. Rarely they get converted to GHB (gamma-hydroxybutyrate) resulting in systemic toxicity.
French Nail Manicure
This method is used to provide a "natural" appearance to the nail. A pink color is applied to the main nail plate, while a white color is applied to the free edge, simulating a natural un-painted nail, picturing good health [Figure - 2].
 |
| Figure 2: French Manicure - It stems from the idea of a healthy nail where the free edge of the nail is bright white and the proximal nail has a pink hue |
Nail Adornment
- The cosmetic appeal of nail polish can be enhanced with the application of ready-use plastic or metal artifacts immediately before the polish dries.
- The design pieces are skillfully lifted from a template with forceps and placed on the freshly applied wet nail polish, in a planned pattern [Figure - 3]a and b.

Figure 3: (a and b) Nail adornment - This is then covered by a top coat, which prevents it from getting dislodged.
- Nail design can also be made, allowing the first layer of color polish to dry completely and subsequently painting a second contrasting color on top of the first, with a design template.
Artificial Nails
Artificial nails evolved from the need for lengthening or reinforcing soft, brittle, or damaged nails. These can be partially attached as nail tips or used to reinforce the entire length as sculpted nails (acrylic or gel based).
Nail Tips
Ready-to-use plastic plates, shaped like nail tips are available at nail salons. These are glued to the free edge of the nails with adhesives containing methacrylate or ethyl 2-cyanoacrylate. The nail surface is filed roughly prior to gluing the nail tip, in order to improve adhesion. The glued-on tips are then painted or decorated with nail art and finally coated with acrylic or gel [Figure - 4]a and b. Entire plastic nails can be stuck on. The tips can be removed with acetone.
 |
| Figure 4: (a and b) Nail art - Decorative art along with sparkles add to the final effect of the nail |
Sculptured Nails
These are either acrylic or gel based and are sculpted over the existing un-aesthetic nail. Both acrylic or gel-based nails involve a mix of a powder and a solution, applied to the nail. A disposable foil with a printed grid is used as a template for the application of materials.
Acrylic nails
A few drops of ethyl methacrylate mixed with powdered poly-methacrylate results in a polymerized mixture that needs to be applied quickly due to the instant setting potential. A uniformly thin layer is applied to achieve the desired effect. The powder contains benzyl peroxide, which acts as a catalyst, while hydroquinone acts as an inhibitor of polymerization. Individual brands may add titanium dioxide and permitted colors. A further modification of the process is the gluing of pieces of silk, linen, or fiber glass to the nail, prior to the acrylic application. These are called "nail wraps" and add strength to the nails. Acrylic nails can be removed with acetone.
Gel nails
The powder and the liquid phase of gels is akin to dental resin and requires specific UV-light exposure to set and cure (harden) the gel after application on the nail. These nails appear glossy, are aesthetically appealing, have greater strength for endurance to physical wear and tear, and need less after-care [Figure - 5]. Gel nails can be removed only by completely buffing them off the nail plate. This results in physical damage to the nail plate during each removal. "Touch-up" procedures are required for both acrylic and gel nails. As the nail plate grows, a gap appears at the proximal end between the nail fold and the artificial nail [Figure - 6] that needs to be filled up at regular intervals, usually every 2-3 weeks.
 |
| Figure 5: Gel nails - These look similar to acrylic nails but are stronger and appear more glossy |
 |
| Figure 6: Development of a clear area at the proximal nail fold as the nail grows out. Note also the onycholysis in the little finger |
Adverse Effects
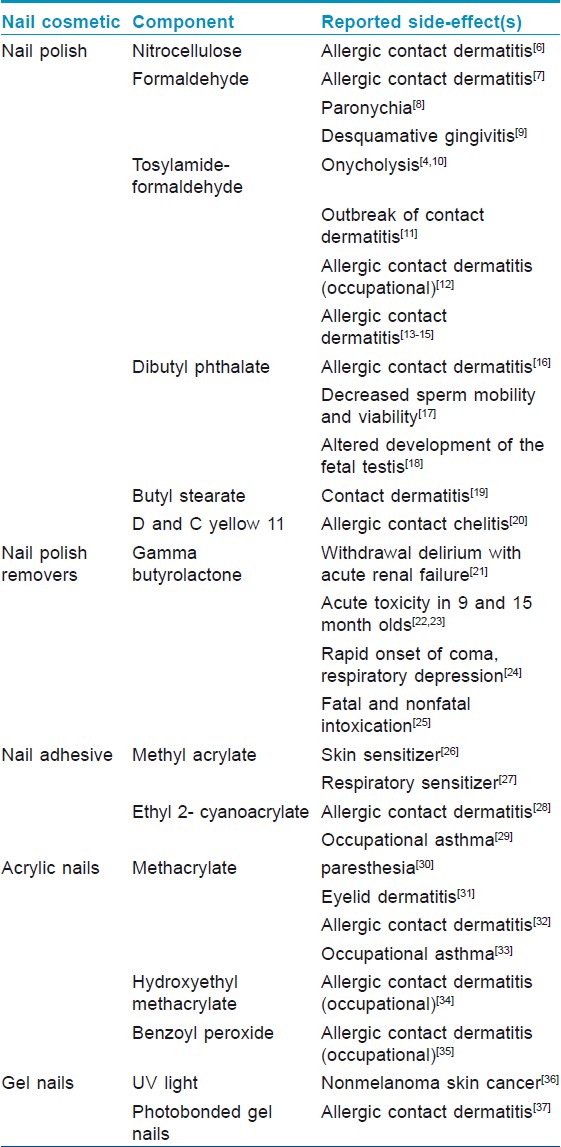
These can be broadly categorized as those due to the chemical components or complications during or subsequent to the nail-grooming procedure. Most reported adverse reactions due to the chemical components have been tabulated in [Table - 1].
Procedural complications of a manicure/pedicure
These may occur in the periungual tissue, the nail plate, or at distant sites due to an allergic contact dermatitis.
- Cuticular cuts and "hang" nails are common with the cuticle-trimming procedure and can be very painful.
- Irritant reactions or chemical burns following use of the cuticle softener are usually seen around the proximal paronychial fold.
- Clipping nails when dry can cause onychoschizia, with horizontal splitting of the nail plate in layers, making it brittle.
- Over-zealous buffing of the nail plate can thin the nail plate and cause fragility.
- Paronychias, bacterial, fungal, and viral infections, especially verrucae, can be inoculated or spread between patients with the use of non-sterile implements.
- Pedicure tubs in which hands and feet are soaked have been reported to cause Mycobacterium fortuitum infections from a nail salon in California. [38]
The physical process of nail beautification has its own set of adverse events, as have been enumerated earlier. Softening/pushing back/cutting of the cuticle, in nail parlance, is a very important step. Anatomically, the cuticle has a very important role in sealing the potential dead space below the proximal nail fold. A damaged cuticle exposes this walled-off space to external agents like detergents and bacterial, viral, and fungal pathogens. Subsequently, acute-over-chronic paronychia ensues, which, over time, results in nail dystrophy. Cuticle softeners contain alkaline chemicals that cause an irritant dermatitis. Dombrowski and Llyod reported a case of chemical damage to the cuticle and nail plate by application of a callus remover instead of a cuticle softener, under occlusion, resulting in arrest of cuticle formation. [39]
Separation of the nail plate from the nail bed can result from over-zealous clipping of the hyponychium or as a consequence of a "lever effect" following minimal trauma, especially in long "strengthened" sculpted nails.
Hapalonychia, the thinning of the nail plate postbuffing, results in weak foldable nails.
Onychoshizia may be attributed to faulty trimming when the nails are dry, leading to horizontal layering of the nail plate.
Repeated use of nail polish, especially deep colors like red, often stain the nail plate. Staining was reproduced with D and C red no 7, D and C red no 34, D and C red no 6 and FD and C yellow no 5 lake. The likelihood of staining increases if the pigments are dissolved and not suspended [Figure - 7].
 |
| Figure 7: Prominent staining of nail plate along with onycholysis results from regular and repeated use of nail polish and nail polish removers |
Patients may develop delayed hypersensitivity reactions around the painted nail and rarely present with acute contact dermatitis. Allergic contact dermatitis from nail polishes has been seen to affect distant sites like face and neck commonly, especially on the eyelids and around the mouth. Unusual involvement of other distant sites like the genitals and perianal region have also been reported. [40] TSFR was the seventh most common ingredient causing contact dermatitis in patients with a cosmetic allergy. [2]
Baran described surface friability of the nail plate, mimicking a white superficial onychomycosis, following the use of nail products [Figure - 8]. The keratin granulations occurred more commonly when the nail polish was kept on for several months or when it was re-applied without removing the first coat and also when a primer base coat was not applied. [41]
 |
| Figure 8: Keratin granules simulating superficial onychomycosis |
Nickel-sensitive patients may develop an allergic contact dermatiis due to the adornments. In such patients, adornments chosen may be of gold or may be nickel free. [42]
Relevance of Nail Cosmetics in a Healthcare Setting
Long fingernails harbor bacteria, and antimicrobial soaps/gels may not be sufficient for complete elimination. Long nails are cumbersome, reduce grip, and tend to puncture gloves. Hence, they are best avoided by medical professional in healthcare settings. Wynd et al. in their study on 102 perioperative nurses concluded that chipped nail polish or nail polish worn for more than 4 days increased bacteria on fingernails. [43] Opaque nail polish can mask nail signs during a clinical examination. The possible role of nail varnish in altering pulse oximeter reading has long been debated. However, it has now conclusively been seen that there is no effect in the measurements from healthy or hypoxic subjects. Chan et al. suggest placing the probe in a side-to-side position on the finger to preclude any disparity in the measurements. [44]
Nail Cosmetics in Nail Disease
Many dermatological diseases cause disfigurement of the nail plate, which may be cosmetically unacceptable to the patient and reduce his or her quality of life. The duration of treatment for most intractable nail disorders is long, with poor efficacy. While waiting for the therapeutic response, cosmetic camouflage helps the patients tide over the mental discomfort. [45] Nail polish application may be adequate for camouflaging dyschromias and mild dystrophies. Gel or acrylic nails may be helpful in concealing moderate nail dystrophy. For cases of anonychia or severe nail dystrophy, a nail prosthesis may be the only option. This prosthesis consists of a false nail attached to a silicone finger glove molded to the specifications of the corresponding finger of the opposite hand. [46]
Nail Cosmetics in Children
Nail cosmetics are generally not recommended for use in children. However, the author has seen mothers using it on their children′s nails in order to break the nail-biting habit, the deterrent being the taste. This is not advisable, as there is always a possibility to develop adverse reactions. [47]
Occupational Hazards for Nail Technicians
Nail technicians are at a risk of occupational hazards due to constant exposure to chemicals used for various nail cosmetic procedures. Increasing number of technicians are sensitized to acrylate monomers used on sculpted nails. Some are at risk for developing occupational asthma due to the cyanoacrylates used. [29] McNary and Jackson concluded in their study that neither nail technicians nor consumers are at any additional risk when exposed to formaldehyde and toulene at their work place compared with exposure from commercial products at home. [48]
Unusual Adverse Effects
Nail polish remover pads were reported to have caused bilateral pneumothoraces, pneumomediastinum, and respiratory obstruction in a 15-month-old child who accidently sucked on them. Fortunately, with medical treatment, the child recovered completely. [23] Turgut et al. reported a case of bacterial endocarditis developing as a consequence of a pedicure. [49] A series of patients developing candidal osteomyelitis and diskitis, narrowed down to a nurse who was wearing artificial nails, was reported by Parry et al. [50]
Testing for Adverse Reactions to Nail Cosmetics
- Nail polish should be tested as it is.
- A specific resin can be tested in 10% petrolatum.
- Nail acrylate allergy should be tested with 2-hydroxy methacrylate, ethyl cyanoacrylate, and methyl methacrylate monomer 10% in olive oil. [51]
- Patch testing for nail polish removers should be an open patch test, at a concentration of 10%, dissolved in olive oil.
- Cuticle removers tested as a 2% aqueous concentration as an open patch test.
Tips to Provide to Patients Visiting a Nail Salon
- The nail salon should have a clean environment.
- The nail technicians should be neatly attired and have clean nails.
- Check how the nail implements are cleaned and sterilized. Implements like nail clippers, nail cutters, foot scrapers, callus removers, and electric drills are sterilized best with autoclaving or soaking in 7.5% stabilized hydrogen peroxide for 6 h or in >2.4% gluteraldehyde-based formulations for 10 h to remove all pathogenic organisms and spores. The trend at the parlors is to soak the instruments for 10 min in disinfectants like benzalkonium chloride. [52] These may still harbor bacteria, fungi, yeast, and viruses. [51]
- Carrying one′s own implements is a wise decision.
- Nails should be cut only after soaking for 10-20 min in water to prevent onychoschizia. [4]
- Over-zealous pushing back the cuticle or nipping the cuticle by the technician should be avoided, as it leads to infection and inflammation of the nail folds.
- Nail polish should be left on for few days only, and cleaned off with acetone-free cleansers. Nail hardeners too need to be cleaned off every 2-3 days. Inform the patient about the probable staining effect of dark nail polish. Avoid layering on nail polish without cleaning off the old one.
- Inform the patients about nail plate damage with application of artificial nails.
- Any swelling, pain, redness, and growths around the nails should be attended to by a medical practitioner.
Conclusion
Although nail cosmetics are advantageous for "beautifying" or concealing various nail disorders, adverse effects are a definite possibility. As dermatologists, a complete knowledge of various nail products, nail-enhancement procedures, and anticipated complications and their management can result in better patient care.
| 1. |
Nail polish. Available from: http://en.wikipedia.org/wiki/Nail_polish. [accessed on 2011 Jun 10].
[Google Scholar]
|
| 2. |
Rich P. Nail cosmetics. Dermatol Clin 2006;24:393-9.
[Google Scholar]
|
| 3. |
Schlossman ML. Nail enamel resins. Cosmet Technol 1979;1:53.
[Google Scholar]
|
| 4. |
Dahdah MJ, Scher RK. Nail diseases related to nail cosmetics. Dermatol Clin 2006;24:233-9.
[Google Scholar]
|
| 5. |
Helsing P, Austad J, Talberg HJ. Onycholysis induced by nail hardener. Contact Dermatitis 2007;57:280-1.
[Google Scholar]
|
| 6. |
Castelain M, Veyrat S, Laine G, Montastier C. Contact dermatitis from nitrocellulose in a nail varnish. Contact Dermatitis 1997;36:266-7.
[Google Scholar]
|
| 7. |
de Groot A, Geier J, Flyvholm MA, Lensen G, Coenraads PJ. Formaldehyde-releasers: Relationship to formaldehyde contact allergy: Metalworking fluids and remainder. Part 1. Contact Dermatitis 2010;63:117-28.
[Google Scholar]
|
| 8. |
Moossavi M, Scher RK. Nail care products. Clin Dermatol 2001;19:445-8.
[Google Scholar]
|
| 9. |
Staines KS, Felix DH, Forsyth A. Desquamative gingivitis, sole manifestation of tosylamide/formaldehyde resin allergy. Contact Dermatitis 1998;39:90.
[Google Scholar]
|
| 10. |
Brauer EW. Onycholysis secondary to toluene sulfonamide formaldehyde resin used in a nail hardener mimicking onychomycosis. Cutis 1980;26:588.
[Google Scholar]
|
| 11. |
de Wit FS, de Groot AC, Weyland JW, Bos JD. An outbreak of contact dermatitis from toluenesulfonamide formaldehyde resin in a nail hardener. Contact Dermatitis 1988;18:280-3.
[Google Scholar]
|
| 12. |
Koch P. Occupational allergic contact dermatitis from epoxy resin systems and possibly acetone in a shoemaker. Contact Dermatitis 2002;46:362-3.
[Google Scholar]
|
| 13. |
Jacob SE, Stechschulte SA. Tosylamide/formaldehyde resin allergy: A consideration in the atopic toddler. Contact Dermatitis 2008;58:312-3.
[Google Scholar]
|
| 14. |
Yokota M, Thong HY, Hoffman CA, Maibach HI. Allergic contact dermatitis caused by tosylamide formaldehyde resin in nail varnish: An old allergen that has not disappeared. Contact Dermatitis 2007;57:277.
[Google Scholar]
|
| 15. |
Stechschulte SA, Avashia N, Jacob SE. Tosylamide formaldehyde resin. Dermatitis 2008;19: E18-9.
[Google Scholar]
|
| 16. |
Gach JE, Stone NM, Finch TM. A series of four cases of allergic contact dermatitis to phthalic anhydride/trimellitic anhydride/glycols copolymer in nail varnish. Contact Dermatitis 2005;53:63-4.
[Google Scholar]
|
| 17. |
Pant N, Pant A, Shukla M, Mathur N, Gupta Y, Saxena D. Environmental and experimental exposure of phthalate esters: The toxicological consequence on human sperm. Hum Exp Toxicol 2011;30:507-14
[Google Scholar]
|
| 18. |
Habert R, Muczynski V, Lehraiki A, Lambrot R, Lécureuil C, Levacher C, et al. Adverse effects of endocrine disruptors on the foetal testis development: Focus on the phthalates. Folia Histochem Cytobiol 2009;47: S67-74.
[Google Scholar]
|
| 19. |
de Groot AC, van der Meeren HL, Weyland JW. Cosmetic allergy from stearic acid and glyceryl stearate. Contact Dermatitis 1988;19:77-8.
[Google Scholar]
|
| 20. |
Sasseville D, Joncas V. Allergic contact cheilitis from D and C Yellow 11. Contact Dermatitis 2009;60:294-5.
[Google Scholar]
|
| 21. |
Bhattacharya IS, Watson F, Bruce M. A case of γ-butyrolactone associated with severe withdrawal delirium and acute renal failure. Eur Addict Res 2011;17:169-71
[Google Scholar]
|
| 22. |
Savage T, Khan A, Loftus BG. Acetone-free nail polish remover pads: Toxicity in a 9-month old. Arch Dis Child 2007;92:371.
[Google Scholar]
|
| 23. |
Brown JJ, Nanayakkara CS. Acetone-free nail polish removers: Are they safe? Clin Toxicol (Phila) 2005;43:297-9.
[Google Scholar]
|
| 24. |
Rambourg-Schepens MO, Buffet M, Durak C, Mathieu-Nolf M. Gamma butyrolactone poisoning and its similarities to gamma hydroxybutyric acid: Two case report. Vet Hum Toxicol 1997;39:234-5.
[Google Scholar]
|
| 25. |
Lenz D, Rothschild MA, Kröner L. Intoxications due to ingestion of gamma-butyrolactone: Organ distribution of gamma-hydroxybutyric acid and gamma-butyrolactone. Ther Drug Monit 2008;30:755-61.
[Google Scholar]
|
| 26. |
Kanerva L, Lauerma A, Jolanki R, Estlander T. Methyl acrylate: A new sensitizer in nail lacquer. Contact Dermatitis 1995;33:203-4.
[Google Scholar]
|
| 27. |
Borak J, Fields C, Andrews LS, Pemberton MA. Methyl methacrylate and respiratory sensitization: A critical review. Crit Rev Toxicol 2011;41:230-68.
[Google Scholar]
|
| 28. |
Isaksson M, Siemund I, Bruze M. Allergic contact dermatitis from ethylcyanoacrylate in an office worker with artificial nails led to months of sick leave. Contact Dermatitis 2007;57:346-7.
[Google Scholar]
|
| 29. |
Jurado-Palomo J, Caballero T, Fernández-Nieto M, Quirce S. Occupational asthma caused by artificial cyanoacrylate fingernails. Ann Allergy Asthma Immunol 2009;102:440-1
[Google Scholar]
|
| 30. |
Freeman S, Lee MS, Gudmundsen K. Adverse contact reactions to sculptured acrylic nails: 4 case reports and a literature review. Contact Dermatitis 1995;33:381-5.
[Google Scholar]
|
| 31. |
Guin JD. Eyelid dermatitis from methacrylates used for nail enhancement. Contact Dermatitis 1998;39:312-3.
[Google Scholar]
|
| 32. |
Baran R. Nail cosmetics: Allergies and irritations. Am J Clin Dermatol 2002;3:547-55.
[Google Scholar]
|
| 33. |
Sauni R, Kauppi P, Alanko K, Henriks-Eckerman ML, Tuppurainen M, Hannu T. Occupational asthma caused by sculptured nails containing methacrylates. Am J Ind Med 2008;51:968-74.
[Google Scholar]
|
| 34. |
Andersen SL, Rastogi SC, Andersen KE. Occupational allergic contact dermatitis to hydroxyethyl methacrylate (2-HEMA) in a manicurist. Contact Dermatitis 2009;61:48-50.
[Google Scholar]
|
| 35. |
Dejobert Y, Martin P, Piette F, Thomas P, Bergoend H. Contact dermatitis caused by benzoyl peroxide in podiatrists. Contact Dermatitis 1999;40:163.
[Google Scholar]
|
| 36. |
MacFarlane DF, Alonso CA. Occurrence of nonmelanoma skin cancers on the hands after UV nail light exposure. Arch Dermatol 2009;145:447-9.
[Google Scholar]
|
| 37. |
Cravo M, Cardoso JC, Gonçalo M, Figueiredo A. Allergic contact dermatitis from photobonded acrylic gel nails: A review of four cases. Contact Dermatitis 2008;59:250-1.
[Google Scholar]
|
| 38. |
Winthrop KL, Albridge K, South D, Albrecht P, Abrams M, Samuel MC, et al. The clinical management and outcome of nail salon acquired Mycobacterium fortuitum skin infections. Clin Infect Dis 2004;38:38-44.
[Google Scholar]
|
| 39. |
Dombrowski NC, Lloyd JR. Nail changes induced by application of a callus eliminator during a manicure. J Am Acad Dermatol 2005;52: E4.
[Google Scholar]
|
| 40. |
Lazzarini R, Duarte I, de Farias DC, Santos CA, Tsai AI. Frequency and main sites of allergic contact dermatitis caused by nail varnish. Dermatitis 2008;19:319-22.
[Google Scholar]
|
| 41. |
Brauer E, Baran R. Cosmetics: The care and adornment of nail. In: Baran R, Dawber RPR, de Berker D, et al., editors. Diseases of the nail and their management. 3 rd ed. Oxford (UK): Blackwell; 2001. p. 358-69.
[Google Scholar]
|
| 42. |
Draelos ZD. Nail cosmetic issues. In: Hordinsky M, Sawaya ME, Scher RK, editors. Atlas of Hair and Nails. 1 st ed. New York: Churchill Livingstone; 1999. p. 184.
[Google Scholar]
|
| 43. |
Wynd CA, Samstag DE, Lapp AM. Bacterial carriage on the fingernails of OR nurses. AORN J 1994;60:796
[Google Scholar]
|
| 44. |
Chan MM, Chan MM, Chan ED. What is the effect of finger nail polish on pulse oximetry? Chest 2003;123:2163-4.
[Google Scholar]
|
| 45. |
Iorizzo M, Piraccini BM, Tosti A. Nail cosmetics in nail disorders. J Cosmet Dermatol 2007;6:53-8.
[Google Scholar]
|
| 46. |
Baran R. Nail cosmetology. In: Baran R, De Berker D, Dawber RP, editors. Manual of nail Disease and Surgery. 2 nd ed. London: Blackwell Science Ltd; 1997 p. 50.
[Google Scholar]
|
| 47. |
Ozkaya E, Mirzoyeva L. Tosylamide/formaldehyde resin allergy in a young boy: Exposure from bitter nail varnish used against nail biting. Contact Dermatitis 2009; 60:171-2.
[Google Scholar]
|
| 48. |
McNary JE, Jackson EM. Inhalation exposure to formaldehyde and toluene in the same occupational and consumer setting. Inhal Toxicol 2007;19:573-6.
[Google Scholar]
|
| 49. |
Turgut F, Kanbay M, Uz B, Carlioglu A, Selcoki Y, Karanfil A, et al. A forgotten but important risk factor for infective endocarditis in patients with prosthetic valve: Pedicure. Scand J Infect Dis 2007;39:274-6.
[Google Scholar]
|
| 50. |
Parry MF, Grant B, Yukna M, Adler-Klein D, McLeod GX, Taddonio R, et al. Candida osteomyelitis and diskitis after spinal surgery: An outbreak that implicates artificial nail use. Clin Infect Dis 2001;32:352-7
[Google Scholar]
|
| 51. |
Baran R, Dawber RP. The nail and cosmetics. In: Samman PD, Dav F, editors. The Nails in Disease. 4 th ed. Chicago: Year-book Publishers; 1986. p. 129.
[Google Scholar]
|
| 52. |
Kurtzweil P. Fingernails: Looking good while playing safe. FDA Consum 1995;29:20-4.
[Google Scholar]
|
Fulltext Views
22,584
PDF downloads
7,202





