Translate this page into:
Nodular secondary syphilis mimicking cutaneous lymphoreticular process
Correspondence Address:
B K Brar
C/o Brar Eye Hospital, Lajpat Nagar, Kotkapura - 151 204, Punjab
India
| How to cite this article: Brar B K, Mehta V, Raj RT. Nodular secondary syphilis mimicking cutaneous lymphoreticular process. Indian J Dermatol Venereol Leprol 2007;73:437-438 |
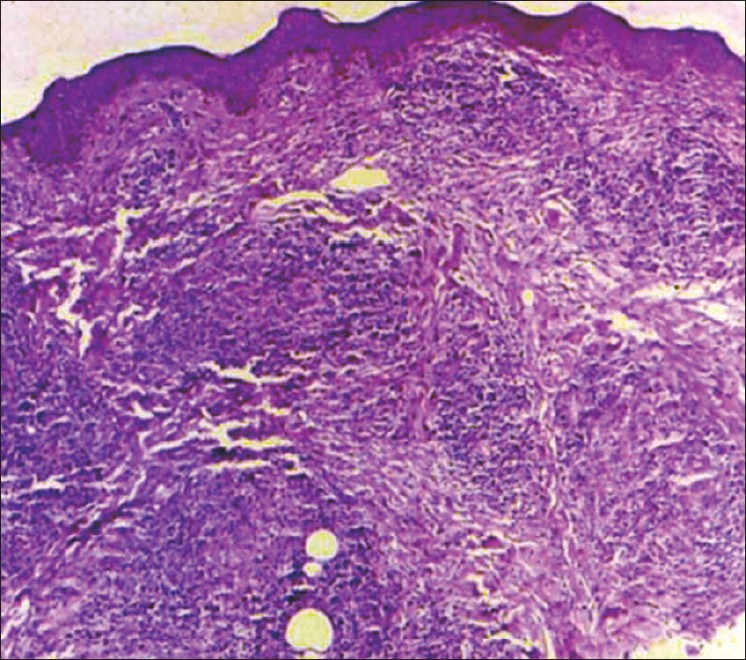 |
| Figure 2: Dense granulomatous infi ltrate in upper reticular dermis (H and E, X40) |
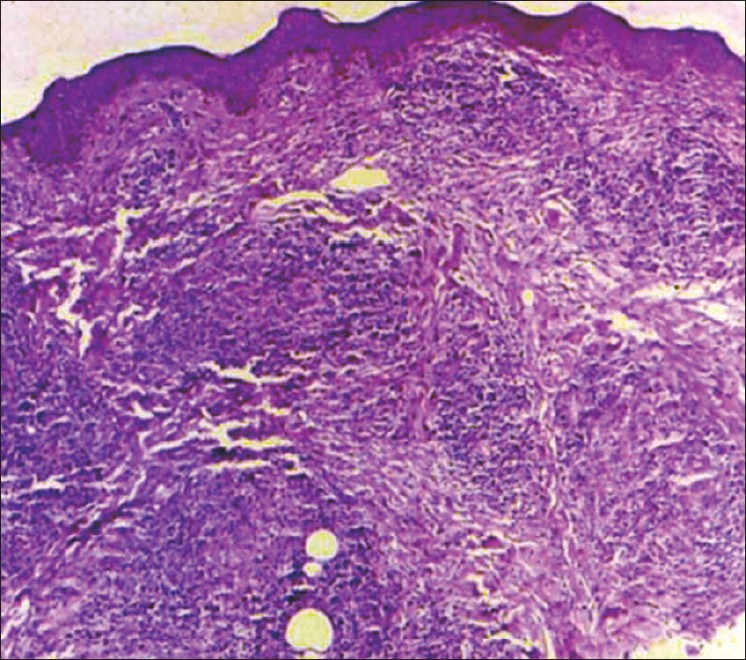 |
| Figure 2: Dense granulomatous infi ltrate in upper reticular dermis (H and E, X40) |
 |
| Figure 1: Large smooth, fi rm, dusky red nodules measuring in size from 1�1 cm to 3�2 cm on forehead and malar regions. Alopecia over nodular lesions was present on eyebrows and eyelid margins |
 |
| Figure 1: Large smooth, fi rm, dusky red nodules measuring in size from 1�1 cm to 3�2 cm on forehead and malar regions. Alopecia over nodular lesions was present on eyebrows and eyelid margins |
Sir,
Secondary syphilis has got different presentations. It should be considered in differential diagnosis of nodular lesions resembling cutaneous lymphoreticular processes. We report here a case of a 28 year-old man, which on the basis of clinical findings, was provisionally diagnosed as cutaneous lymphoreticular process. Diagnosis was eventually made after results of serological tests of syphilis were found to be positive with high titers in the venereal disease research laboratory (VDRL) test, histopathological findings and rapid response after first injection of benzathine penicillin.
A 28 year-old Indian man presented for evaluation of numerous non-itchy erythematous plaques and nodules on the face, chest, back and upper extremities along with intense pain in the legs of 25 days′ duration. One and a half months earlier, he had been treated for high-grade fever with body ache with antibiotics and antipyretics. He remained well for 20 days except for generalized body aches. Physical examination revealed an afebrile patient with bilateral enlarged, firm, mobile, nontender cervical, axillary, inguinal and epitrochlear lymph nodes. Dermatological examination revealed numerous erythematous plaques and papulonodular lesions on the face, upper chest, back and upper extremities. Large nodular lesions measuring in size from 1 x 1 cm to 3 x 2 cm were present on the face especially on the forehead and malar regions which were smooth, firm and dusky red [Figure - 1]. Alopecia over the nodular lesions was present on the eyebrows and eyelid margins. Palms, soles and mucous membranes were spared. There was no history of any loss of weight. Initial presenting clinical diagnosis was malignant lymphoreticular disease. Laboratory tests demonstrated a moderate rise in erythrocyte sedimentation rate (ESR) (32 mm at the end of the 1st hour) and the total leukocyte count (TLC) of 9,300/cu. mm with normal differential counts. VDRL test was then reported to show positive results with a titer of 1:512. Consequently, the Treponema pallidum hemagglutination (TPHA) test was also found to be positive. Anti-human immunodeficiency virus (HIV) antibodies were found to be negative. Skin biopsy was performed, which showed dense granulomatous infiltrate present in upper reticular dermis made up of mainly plasma cells, epitheloid cells and lymphocytes. Granulomas were not of the sarcoidal type [Figure - 2]. Diagnosis of secondary syphilis was confirmed on the basis of positive serological tests, clinical and histopathological findings. On enquiry, the patient admitted having extramarital sexual contact with a commercial sex worker several months back. The patient was then pretreated with analgesics and oral steroids to avoid the Jarisch Herxheimer reaction. The patient was given intramuscular benzathine penicillin 2.4 M units weekly for three weeks. There was a marked clinical response after the first injection and a gradual resolution of nodular eruption and regression of lymph nodes within six weeks together with normalization of ESR. Lesions healed with mild erythema, which was aggravated after exposure to the sun. Symptomatic treatment was given for photosensitivity. VDRL titers after three and six months were 1:64 and 1:32 respectively.
Secondary syphilis should be considered as a good imitator in view of its protean clinical and laboratory presentations, which not uncommonly mimic other diseases. The appellation of syphilis as "the great imitator" has been attributed to Sir William Osler, but in reality was coined by Sir Jonathan Hutchinson almost 20 years earlier. [1] The eruption of secondary syphilis has certain characteristics that help to identify and distinguish it from other dermatoses. The cutaneous manifestations characterizing secondary syphilis are usually superficial, classically comprising four major types of rash: macular, papular, papulosquamous or pustular. [2] Nodular lesions in syphilis are typical of the late benign stage of the disease. The eruption is generalized, involving both skin and mucous membranes, is bilateral, symmetrical and more prominent on the upper extremities than on the abdomen and the lower extremities. It has a special predilection for the palms and the soles although these may be clear only in the early stages. The lesions are discrete rather than confluent, have a coppery hue and are sharply demarcated. Scales when present, tend to be located peripherally rather than centrally.
Generalized lymphadenopathy and numerous large nodular lesions on the face are likely to be misdiagnosed as lymphoma not only clinically, [3] but also both clinically and histopathologically. [4],[5] Such cases are a reminder that syphilis should be considered as a differential diagnosis of generalized lymphadenopathy. Other differential diagnosis of secondary syphilis such as sarcoidosis, leishmaniasis, leprosy, atypical mycobacterial infections and deep fungal infections were retained in our patient. The histopathological report suggested a dense granulomatous infiltrate in the upper reticular dermis, which led us to consider the diagnosis of lymphoma. It was only after the positive serological tests for syphilis that a diagnosis of nodular secondary syphilis was considered.
| 1. |
Jackson R. Jonathan Hutchinson on syphilis. Sex Transm Dis 1980;7:90-6.
[Google Scholar]
|
| 2. |
Chapel TA. Primary and secondary syphilis. Cutis 1984;33:47-53.
[Google Scholar]
|
| 3. |
Nayeem SA, Berhradt B. Syphiltic lymphadenopathy. JAMA 1978;239:495.
[Google Scholar]
|
| 4. |
Goffinet DR, Hoyt C, Eltringham JR. Secondary syphilis misdiagnosed as lymphoma. West J Med 1970;112:22-3.
[Google Scholar]
|
| 5. |
Drusin LM, Singer C, Valenti AJ, Armstrong D. Infectious syphilis mimicking neoplastic disease. Arch Intern Med 1977;137:156-60.
[Google Scholar]
|
Fulltext Views
5,480
PDF downloads
1,866





