Translate this page into:
Non-pigmenting fixed drug eruption due to fluoroquinolones
Correspondence Address:
Lalit Kumar Gupta
Department of Dermatology, Venereology and Leprology, Rabindranath Tagore Medical College, Udaipur - 313 001, Rajasthan
India
| How to cite this article: Gupta LK, Beniwal R, Khare AK, Mittal A, Mehta S, Balai M. Non-pigmenting fixed drug eruption due to fluoroquinolones. Indian J Dermatol Venereol Leprol 2017;83:108-112 |
Sir,
Non-pigmenting fixed drug eruption is an unusual entity, first defined by Abramowitz and Noun in 1937.[1] The lesions of non-pigmenting fixed drug eruptions heal without any residual pigmentation, unlike the more commonly encountered pigmenting fixed drug eruptions. Fluoroquinolones, a group of commonly prescribed antibiotics, have been incriminated in a significant number of cases of fixed drug eruptions but we were unable to find any previous reports of non-pigmenting fixed drug eruption due to fluoroquinolones.
Case 1
A 23-year-old man presented with a four day history of multiple, itchy, round to oval, well defined, erythematous macules and plaques over the trunk and limbs [Figure - 1]a,[Figure - 1]b,[Figure - 1]c,[Figure - 1]d,[Figure - 1]e,[Figure - 1]f, with onset 6 hours after taking ofloxacin tablet (200 mg), prescribed by the physician for loose stools. The lesions resolved without any residual pigmentation in 2 weeks. The patient denied taking any other medication during this episode and in the preceding 2–3 months. He had a history of developing similar lesions over the same sites on 3 earlier occasions, each time after taking levofloxacin. Each episode resolved in 7–10 days without leaving behind any residual pigmentation. General and systemic examination was unremarkable and routine investigations did not reveal any abnormality. Histopathological examination showed dyskeratotic keratinocytes and perivascular infiltrates of lymphocytes along with neutrophils and eosinophils scattered interstitially. Melanin incontinence was conspicuously absent [Figure - 2]. The patient did not give consent for oral rechallenge. Based on the temporal correlation of lesions appearing after drug intake, previous history of similar reactions after intake of the same drug, and the uneventful self-resolution of lesions without pigmentation, a diagnosis of non-pigmenting fixed drug eruption triggered by fluoroquinolones was made. The causality assessment as per the World Health Organization-Uppsala Monitoring Centre scale [2] was “certain.” He was advised to avoid fluoroquinolones and structurally related drugs and carry with him an adverse drug reaction card to be shown to the prescribing physician before taking any medication.
 |
| Figure 1a: Multiple well defined erythematous macules over chest |
 |
| Figure 1b: Chest lesions after resolution; note the absence of any residual pigmentation |
 |
| Figure 1c: Multiple well defined erythematous macules over back |
 |
| Figure 1d: Lesions over back after resolution |
 |
| Figure 1e: Multiple well defined erythematous macules over lower limbs |
 |
| Figure 1f: Lesions over lower limbs post resolution |
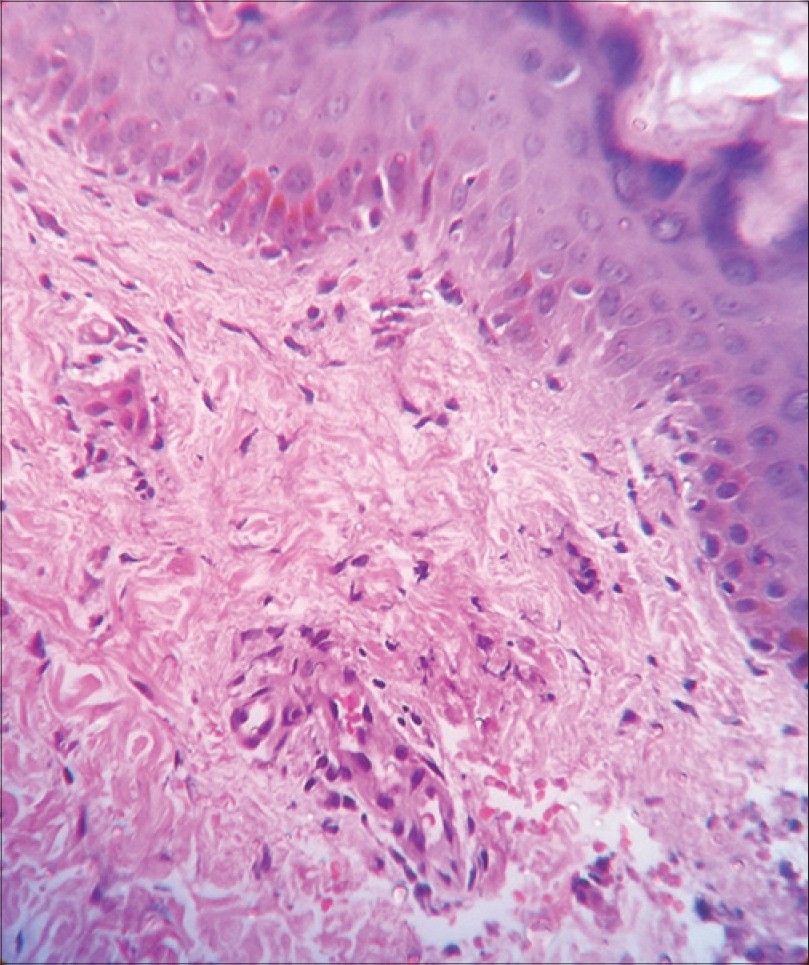 |
| Figure 2: Dyskeratotic keratinocytes and lack of pigmentary incontinence (Case 1) (H and E, ×400) |
Case 2
A 45-year-old laborer developed 2 itchy, round, well defined, erythematous to purpuric macules with vesicobullous change [Figure - 3]a and [Figure - 3]b asymmetrically over the wrists (on the dorsum of one wrist and on the volar aspect of the other wrist), 4 hours after taking a tablet containing norfloxacin (400 mg) and tinidazole (600 mg) for loose stools. There was a history of 7–8 similar episodes in the past. The lesions used to heal without any residual pigmentation in 2–3 weeks. The patient was asked to report for rechallenge after a month. About 2 months later, the patient reported back with similar lesions that developed 2 hours after taking ciprofloxacin (500 mg) from a chemist for a furuncle on the right leg. This time too, the lesions healed without any residual pigmentation in about 2 weeks. A month later, after obtaining informed consent, the patient was challenged with incremental doses of tinidazole without any reaction. Provocation with half the therapeutic dose of norfloxacin (200 mg) resulted in reappearance of lesions at the same sites. Based on the clinical history and positive rechallenge, the diagnosis of non-pigmenting fixed drug eruption to norfloxacin was established. The causality assessment in this case, as per the World Health Organization-Uppsala Monitoring Centre scale,[2] was “certain.”The patient was advised to avoid taking norfloxacin and other fluoroquinolones in future and he was issued an adverse drug reaction card.
 |
| Figure 3a: Active lesions of FDE on wrists |
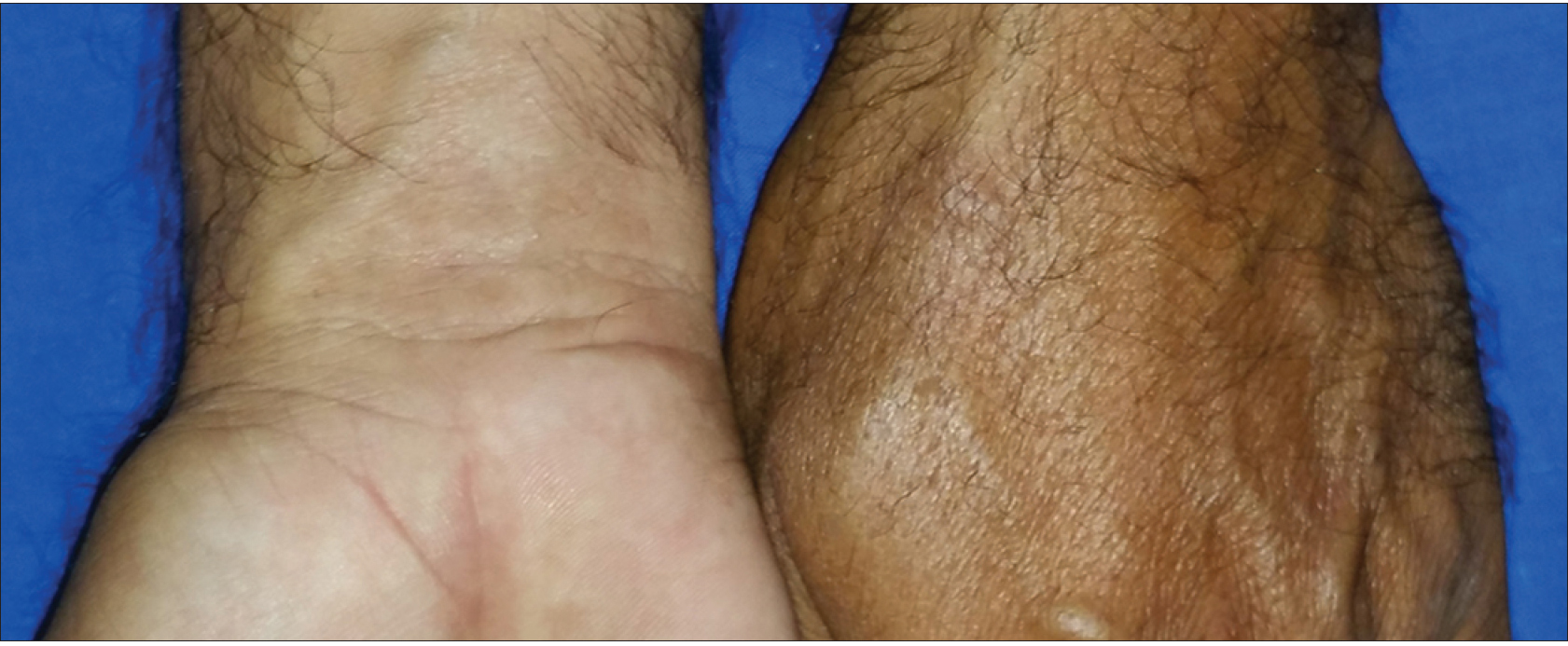 |
| Figure 3b: Healed lesions without any significant pigmentary residue |
Fixed drug eruption is one of the most common types of cutaneous adverse drug reaction and over 100 drugs are known to induce fixed drug eruption.[3] The exact etiology is unknown, but it is believed to be a delayed type hypersensitivity reaction mediated by CD8+ T cells. Epidermal CD8+ memory T cells, which are retained in the lesions, get reactivated on rechallenge. The lesions of typical fixed drug eruptions usually develop within 30 minutes to 8 hours after drug administration as sharply marginated, round or oval itchy plaques of erythema and edema which subsequently become dusky, violaceous or brown and sometimes, vesiculobullous.[4] After the initial acute phase that lasts for days to weeks, a characteristic residual grayish or slate-colored hyperpigmentation remains.[5] The reappearance of the lesions over previously affected sites on rechallenge with the offending drug is considered a diagnostic hallmark.
The concept of non-pigmenting fixed drug eruption, a relatively rare variant in which the lesions resolve without leaving any residual pigmentation, was popularized by Shelley and Shelley in 1987. They postulated that the likely site of the drug-induced hypersensitivity response was the dermis rather than the epidermis, in such cases. Hence, there was no pigment incontinence, and therefore, no pigmentary sequelae after the initial lesion subsided.[6]
Non-pigmenting fixed drug eruption is typically characterized by large, symmetrical, well circumscribed, tender erythematous plaques that fade without pigmentation over 2–3 weeks. This was seen in Case 1. Asymmetrical, localized, non-pigmenting fixed drug eruptions can also occur as seen in Case 2. Non-pigmenting fixed drug eruption has been reported in association with pseudoephedrine, tetrahydrozoline, diflunisal, thiopental, piroxicam, iothalamate, arsephenamine, paracetamol, intra-articular triamcinolone acetonide, eperisone hydrochloride, furazolidone and acetaminophen.[4] Recently, reports of non-pigmenting fixed drug eruption to eprazinone, sorafenib, tadalafil and esomeprazole have also been described.
Flouroquinolones, a widely used group of antibiotics, have been found responsible for a variety of cutaneous adverse drug reactions such as exanthems, urticaria, angioedema, exfoliative dermatitis, photosensitivity, acute generalized exanthematous pustulosis, vasculitis, anaphylaxis and Stevens–Johnson syndrome or toxic epidermal necrolysis, apart from being commonly implicated in fixed drug eruptions. However, an extensive literature search (GoPubMed.org, SearchMedica, Google, Google Scholar, MedlinePlus, Medscape, MedWatch, PubMed Central, Cochrane Summaries) did not reveal any case of non-pigmenting fixed drug eruption caused by this subset of antibiotics. With fluoroquinolones being incriminated as culprits in a considerable number of fixed drug eruptions, we wish to highlight the possibility that this class of drugs can trigger non-pigmenting fixed drug eruptions as well.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Abramowitz EW, Noun MH. Fixed drug eruptions. Arch Dermatol Syph 1937;35:875-92.
[Google Scholar]
|
| 2. |
The use of the WHO-UMC system for standardized case causality assessment. World Health Organization (WHO) — Uppsala Monitoring Centre. Available from: http://www.who-umc.org/Graphics/24734.pdf. [Last accessed on 2013 Apr 10].
[Google Scholar]
|
| 3. |
Guptha SD, Prabhakar SM, Sacchidanand S. Fixed drug eruption due to levocetirizine. Indian J Dermatol Venereol Leprol 2005;71:361-2.
[Google Scholar]
|
| 4. |
Breathnach SM. Drug reactions. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. UK: Wiley-Blackwell; 2010. p. 75. 1-177.
[Google Scholar]
|
| 5. |
Sehgal VN, Srivastava G. Fixed drug eruption (FDE): Changing scenario of incriminating drugs. Int J Dermatol 2006;45:897-908.
[Google Scholar]
|
| 6. |
Shelley WB, Shelley ED. Nonpigmenting fixed drug eruption as a distinctive reaction pattern: Examples caused by sensitivity to pseudoephedrine hydrochloride and tetrahydrozoline. J Am Acad Dermatol 1987;17:403-7.
[Google Scholar]
|
Fulltext Views
6,229
PDF downloads
3,001





