Translate this page into:
Ochronosis with subtle histological findings
2 Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Manoj Kumar Singh
Department of Pathology, All India Institute of Medical Sciences, New Delhi - 110 029
India
| How to cite this article: Vallonthaiel AG, Kakkar A, Singh MK, Ramam M. Ochronosis with subtle histological findings. Indian J Dermatol Venereol Leprol 2015;81:623-624 |
Sir,
Exogenous ochronosis is an increasingly recognized condition that typically presents with blue-black hyperpigmentation of skin;[1] this characteristic discoloration facilitates clinical diagnosis. However, it is sometimes difficult to differentiate ochronosis from melasma clinically, especially when there is no history of topical hydroquinone use. Skin biopsy is the gold standard for diagnosis in such situations with ochronosis displaying characteristic histological features. Findings on skin biopsy may occasionally be so subtle as to be missed if not looked for carefully.
A 45-year-old man presented to us with multiple well-defined brown-black macules over the cheeks, eyebrows and bridge of the nose with a few islands of sparing in between. There was no history of using hydroquinone-containing creams. There were also no clinical features to suggest alkaptonuria such as a history of blackish discoloration of urine or sclerae, arthritis, renal calculi or a family history of similar pigmentary alteration. Based on the clinical features, differential diagnoses of ochronosis and melasma were considered and a skin biopsy was performed.
On histological examination, the epidermis appeared normal and lower (x200) magnification did not show any pigment deposition. However, careful examination under high (x400) magnification revealed that there actually was a scant deposition of pale amber-colored pigment in a few collagen bundles. There was no increase in melanocytes or melanin. The abnormal collagen bundles stained blue-black with methylene blue and were smaller than those usually seen in exogenous ochronosis. Comparative photomicrographs of this case and a case of exogenous ochronosis with classical histomorphology at the same magnifications are shown in [Figure - 1].
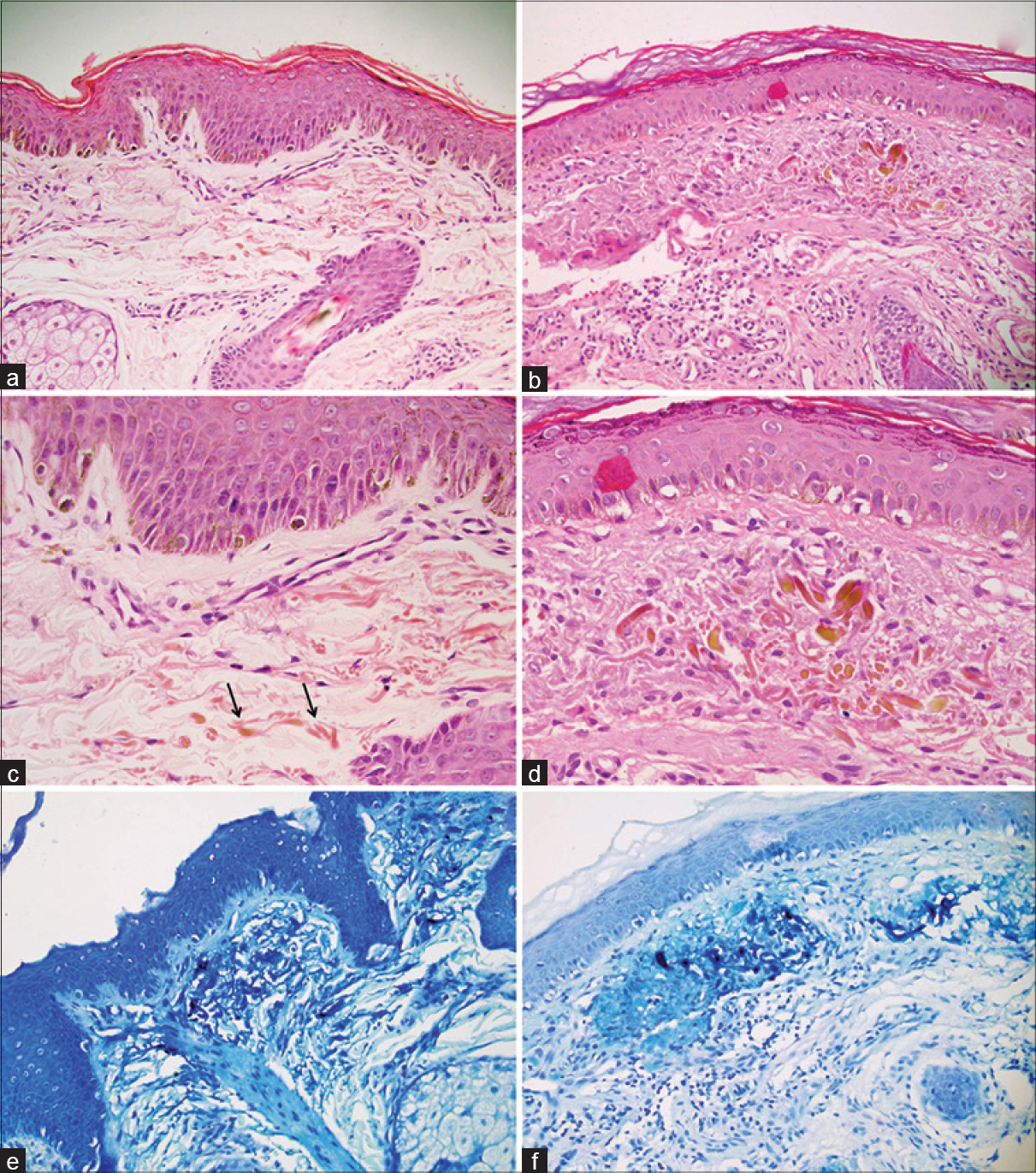 |
| Figure 1: Photomicrographs of our case (a, c and e) compared with a classical case of ochronosis (b, d and f). At lower magnification, there is no visible pigment deposition in (a) while the classical case shows easily identified pigment deposits (b) (H and E, ×200). On higher magnification, scant ochronotic pigment deposits are seen on small fractured collagen bundles in (c), while the typical case shows prominent pigment deposits on thick collagen bundles (d) (H and E, ×400). Methylene blue stain highlights these deposits in both cases (e, f) (×200) |
Endogenous ochronosis or alkaptonuria is an autosomal recessive disease caused by a deficiency of homogentisic acid oxidase resulting in the accumulation of homogentisic acid in tissues. Exogenous ochronosis, unlike endogenous ochronosis, does not involve cartilage, tendons, ligaments or sclerae and is not associated with dark urine.[1] Apart from hydroquinone, other agents including phenol, resorcinol, mercury, picric acid, benzene and systemic antimalarials like quinine have also been implicated in the causation of exogenous ochronosis.[2] These agents inhibit homogentisic acid oxidase in the skin, resulting in local accumulation of homogentisic acid, which then polymerises into the ochronotic pigment.[2] An idiopathic variant of ochronosis has also been described, wherein a detailed history does not reveal the use of any drug, features of alkaptonuria are absent and laboratory tests of blood and urine are negative.[3]
Endogenous and exogenous ochronosis are indistinguishable on histology and the clinical history should be taken into account.[1] Histopathological examination of a skin biopsy in classical ochronosis reveals the characteristic ochre or yellow-brown pigment from which the condition gets its name. The pigment is strikingly present within collagen bundles, which tend to fracture transversely resulting in pointed ends and have been described as banana or comma-shaped. Eventually there is collagen degeneration, and an occasional granuloma may be seen.[1] Fine granules of ochronotic pigment may also be seen intracellularly in the endothelium, macrophages and secretory cells of sweat glands, as well as extracellularly, particularly in basement membranes. Melasma, on the other hand, does not show this pigment; instead melanin is found to be significantly increased in all the epidermal layers.[4] Unlike melanin, ochronotic pigment does not stain with silver nitrate, and blackening on methylene blue or cresyl violet staining is a useful method to characterize it.
Early diagnosis is essential in managing exogenous ochronosis so that hydroquinone application is discontinued to prevent worsening. A skin biopsy is frequently required to establish the diagnosis. The pathologist should be aware that histological findings may be subtle, and in a setting of high clinical suspicion, a thorough examination under high magnification should be carried out to identify the scant pigment deposition, along with methylene blue staining to highlight these deposits.
| 1. |
Martins VM, Sousa AR, Portela Nde C, Tigre CA, Gonçalves LM, Castro Filho RJ. Exogenous ochronosis: Case report and literature review. An Bras Dermatol 2012;87:633-6.
[Google Scholar]
|
| 2. |
Levin CY, Maibach H. Exogenous ochronosis. An update on clinical features, causative agents and treatment options. Am J Clin Dermatol 2001;2:213-7.
[Google Scholar]
|
| 3. |
Prangova D, Hristozov E, Lazarov N, Lazarova R, Gantcheva T, Tzaneva M. Idiopathic variant of skin ochronosis. Trakia J Sci 2005;2:70-2.
[Google Scholar]
|
| 4. |
Ribas J, Schettini AP, Cavalcante Mde S. Exogenous ochronosis hydroquinone induced: A report of four cases. An Bras Dermatol 2010;85:699-703.
[Google Scholar]
|
Fulltext Views
5,313
PDF downloads
1,182





