Translate this page into:
Palmoplantar keratoderma unveiling renal cell carcinoma: A novel paraneoplastic presentation
Correspondence Address:
P Arunprasath
Department of Dermatology and STD, Vinayaka Mission's Medical College and Hospital, Karaikal - 609 609, Union Territory of Puducherry
India
| How to cite this article: Kamalakannan K K, Arunprasath P, Lanka P, Kothandapany S. Palmoplantar keratoderma unveiling renal cell carcinoma: A novel paraneoplastic presentation. Indian J Dermatol Venereol Leprol 2016;82:333-335 |
Sir,
A 70-year-old man presented with asymptomatic thickening of the palms and soles for 6 months. There was no history of anorexia, weight loss or any symptom pertaining to specific systemic involvement. The patient denied exposure to any chemicals which might have contributed to his illness. Dermatological examination revealed diffuse, hyperkeratotic plaques and fissures involving both palms and soles with more marked involvement of the latter [Figure - 1]a and [Figure - 1]b. There was no hyperhidrosis. Hair, nails and mucous membranes were normal. Abdominal examination revealed a bimanually palpable 10 cm × 7 cm mass in the left lumbar region. It was soft, non-tender and ballotable. There was no hepatosplenomegaly. Other systems were clinically normal.
 |
| Figure 1: Diffuse keratoderma involving (a) palms (b) soles |
Hematological and biochemical parameters including serum calcium level were within normal limits, except for anemia (hemoglobin 8 g%) and an elevated erythrocyte sedimentation rate (62 mm/1st hour). Stool examination for occult blood was negative. Chest X-ray and computerized tomography (CT) scan of chest did not reveal any abnormality. CT scan of the abdomen revealed a mass arising from the anterior aspect of the left kidney extending inferiorly up to the level of left iliac crest. It was heterodense with hypodense areas suggestive of renal cell carcinoma [Figure - 2].
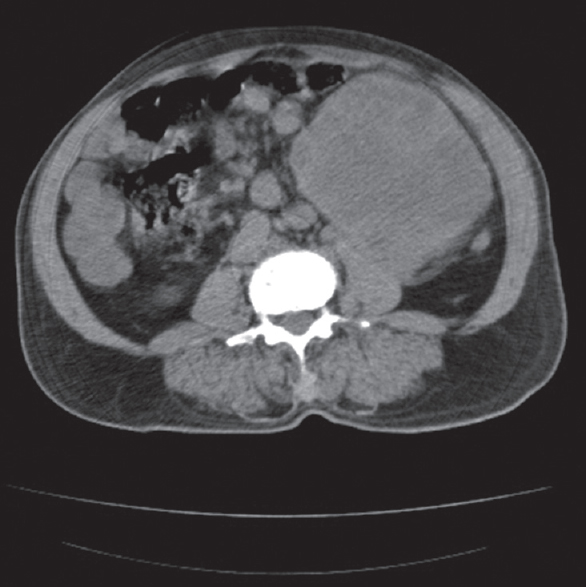 |
| Figure 2: Computerized tomography scan of the abdomen showing heterodense mass lesion arising from the left kidney |
Contrast CT scan of the abdomen and pelvis revealed renal cell carcinoma involving the lower pole of the left kidney. There was infiltration of perinephric fat and invasion of the lower pelvi-calyceal system causing hydronephrosis. Multiple small lymph nodes were detected in the left hilum and perinephric space. The tumor-node-metastasis (TNM) staging was T4N1M0. Histopathological examination of palmar skin showed features of keratoderma [Figure - 3].
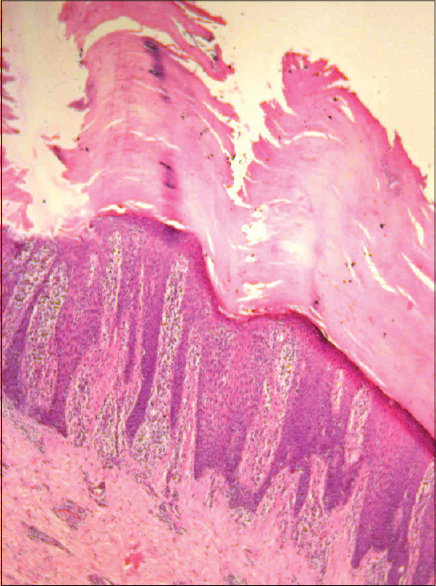 |
| Figure 3: Massive hyperkeratosis, acanthosis and lymphocytic infiltrate in the dermis (H and E, ×100) |
A diagnosis of paraneoplastic diffuse palmoplantar keratoderma associated with renal cell carcinoma was made. Topical keratolytics and emollients were advised for palms and soles. At the regional cancer institute, left radical nephrectomy with para-aortic nodal clearance was done and renal cell carcinoma was confirmed histopathologically [Figure - 4]. The patient succumbed to myocardial infarction during the early postoperative period.
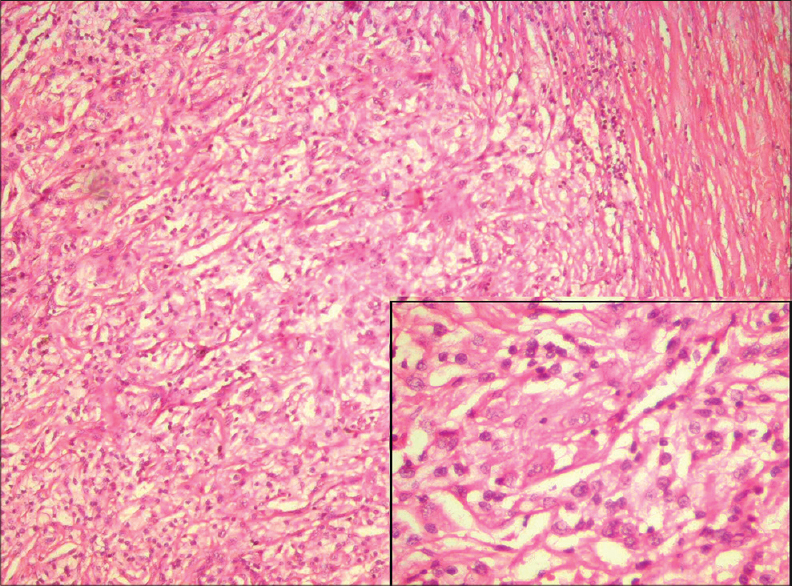 |
| Figure 4: Closely packed tubules and cystic structures (H and E, ×100). Inset showing tumor composed of large cells in sheets and tubule formation (H and E, ×400) |
Palmoplantar keratodermas are a heterogeneous group of disorders characterized by hyperkeratosis of the palms and soles and broadly classified into inherited and acquired types.[1] Acquired keratoderma may be paraneoplastic and morphologically, punctate, focal, or diffuse.[2],[3] Sudden onset of palmoplantar keratoderma in the absence of other findings should raise the suspicion of an underlying malignancy.[3]
Familial punctate and filiform keratoderma have been reported with a variety of malignancies.[2] Punctate palmoplantar keratoderma occurring in elderly individuals, Cowden's syndrome and arsenic toxicity may also be associated with internal malignancy.[4] Our patient had diffuse palmoplantar keratoderma without family history of similar disorder or possibility of arsenic exposure.
Esophageal carcinoma was ruled out in the patient by clinical and radiological screening thus Howel–Evans syndrome was excluded, Moreover, this entity presents with focal keratoderma unlike in the reported patient.
Acquired diffuse palmoplantar keratoderma has been described in patients with carcinoma of lung, breast, kidney and colon.[1] Our patient's paraneoplastic keratoderma was due to underlying renal cell carcinoma. This carcinoma is unique among the genitourinary malignancies as nearly one-third of affected patients present with a paraneoplastic syndrome during primary or metastatic disease.[5] Clinical features vary from constitutional symptoms to specific metabolic and biochemical abnormalities.[5] Palmoplantar keratoderma as a paraneoplastic manifestation of renal cell carcinoma is unusual.
Paraneoplastic cutaneous manifestations reflect interaction between tumor cells and the host. The pathogenesis of these syndromes are ascribed to excessive production or depletion of bioactive substances, growth factors, hormones, or other unidentified mediators produced by the tumor.[3] Renal cell carcinoma is known to produce interleukin-6, -10, vascular endothelial growth factor and transforming growth factor-beta 1.[6] Keratoderma in this case could possibly be attributed to any of these growth factors.
Definitive treatment for paraneoplastic syndromes associated with localized renal cell carcinoma is nephrectomy,[5] as was undertaken in our patient. Documentation of resolution of the keratoderma following removal of the original tumor was not possible in this case because of sudden demise of the patient. We were unable to find any previous reports of acquired palmoplantar keratoderma associated with renal cell carcinoma.
Paraneoplastic palmoplantar keratoderma has to be differentiated from various other causes of acquired keratoderma including hypothyroidism, malnutrition, drugs, infections and infestations, papulosquamous disorders, eczema and aquagenic keratoderma. Keratoderma climactericum (Haxthausen's disease) seen in post-menopausal women is also an important differential diagnosis.[7]
In conclusion, awareness and timely diagnosis of paraneoplastic dermatoses help in early detection and management of the underlying malignancy.
Acknowledgment
The authors thank Adyar Cancer Institute, Chennai, for providing histopathologcal details of the patient's renal cell carcinoma.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Krol AL, Siegel D. Keratodermas. In: Bolognia JL, Jorizzo JL, Schaffer JV, editors. Bolognia Textbook of Dermatology. 3rd ed. Please re-check: Elsevier; 2013. p. 871-85.
[Google Scholar]
|
| 2. |
Judge MR, Mclean WH, Munro CS. Disorders of keratinization. In: Burns T, Breathnach S, Cox NH, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. Oxford: Wiley Blackwell; 2010. p. 19.116.
[Google Scholar]
|
| 3. |
Yuste-Chaves M, Unamuno-Pérez P. Cutaneous alerts in systemic malignancy: Part I. Actas Dermosifiliogr 2013;104:285-98.
[Google Scholar]
|
| 4. |
Cox NH, Coulson IH. Systemic disease and the skin. In: Burns T, Breathnach S, Cox NH, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. Oxford: Wiley Blackwell; 2010. p. 62.33.
[Google Scholar]
|
| 5. |
Palapattu GS, Kristo B, Rajfer J. Paraneoplastic syndromes in urologic malignancy: The many faces of renal cell carcinoma. Rev Urol 2002;4:163-70.
[Google Scholar]
|
| 6. |
Cabillic F, Bouet-Toussaint F, Toutirais O, Rioux-Leclercq N, Fergelot P, de la Pintière CT, et al. Interleukin-6 and vascular endothelial growth factor release by renal cell carcinoma cells impedes lymphocyte-dendritic cell cross-talk. Clin Exp Immunol 2006;146:518-23.
[Google Scholar]
|
| 7. |
Patel S, Zirwas M, English JC 3rd. Acquired palmoplantar keratoderma. Am J Clin Dermatol 2007;8:1-11.
[Google Scholar]
|
Fulltext Views
4,289
PDF downloads
2,700





