Translate this page into:
Papules on the vulva and perianal area in a young woman
*Xiuyan Shi and Xiaohui Shi are equally contributing authors.
Corresponding author: Dr. Hong Luan, No. 67, Dongchang West Road, Dongchangfu District, Liaocheng 252000, Shandong Province, China. lcsrmyy@126.com
-
Received: ,
Accepted: ,
How to cite this article: Shi X, Shi X, Jia A, Meng X, Luan H. Papules on the vulva and perianal area in a young woman. Indian J Dermatol Venereol Leprol 2021;87:736-8.
A 23-year-old woman presented with a 6-month history of a raised pruritic eruption involving the vulva and perianal area. The physical examination revealed multiple white papules, 3–5 mm in size, localized to both sides of the labia majora [Figure 1] and perianal area.

- White papules 3–5 mm in size localized to both sides of the labia majora
The patient was treated with a 1-month course of topical desonide cream for presumed apocrine prurigo; however, there was no apparent improvement in symptoms. The patient underwent a gynecologic examination and no vaginal lesions were noted. No family history of skin disorders was reported. Eight months ago, the patient underwent a spontaneous delivery. A biopsy from a mid-section of the right labia majora revealed acantholytic dyskeratosis. The histopathologic findings showed acantholysis throughout the epidermis with dyskeratotic cells resembling corps ronds and grains. Hyperkeratosis and parakeratosis were also detected in the epidermis with chronic inflammation in the underlying dermis [Figures 2 and 3].
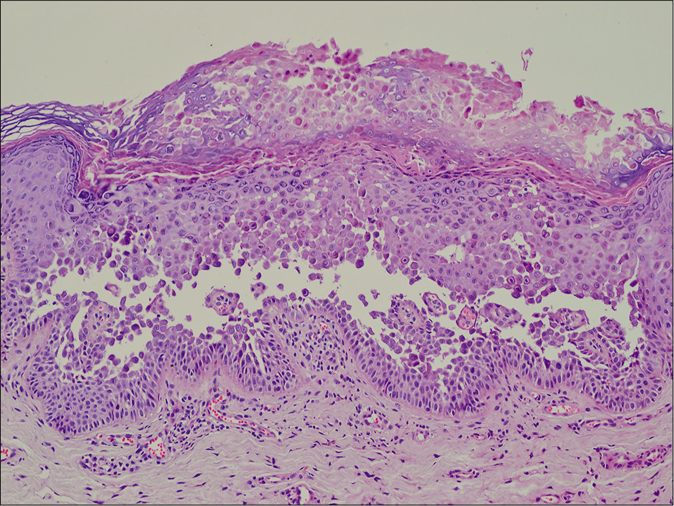
- Acantholysis throughout the epidermis, hyperkeratosis, and parakeratosis were found in the epidermis with chronic inflammation in the underlying dermis (H and E, ×100)
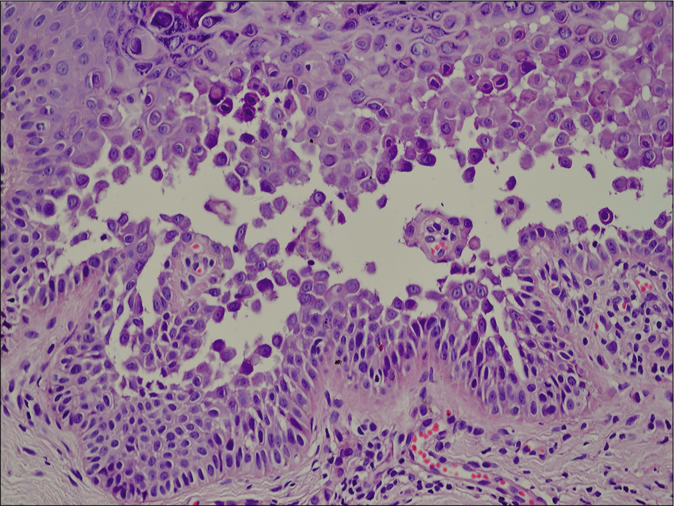
- Acantholysis and dyskeratosis with the presence of corps ronds and grains (H and E, ×400)
Question
What is your diagnosis?
Answer
Papular acantholytic dyskeratosis of the vulva and perianal area.
Discussion
Since the first reporting of papular acantholytic dyskeratosis of the vulva in 1984, there have been sporadic reports wherein the lesions were clinically and histologically similar to papular acantholytic dyskeratosis of the vulva, though not limited to vulva; other sites involved included anogenital and genitocrural areas.1 Papular acantholytic dyskeratosis presents as an eruption of multiple, asymptomatic, or pruritic skin-colored to white papules that may coalesce to form plaques in both genders with no reported family history of a similar condition.
According to a recent review, the anogenital area is the most commonly involved site for papular acantholytic dyskeratosis; the genitocrural area is the second most commonly involved site.2 Both acantholytic dermatoses of the genitocrural area and our case are classified as papular acantholytic dyskeratosis. The reported patient had bilateral involvement of the labia majora, labia minora, and perianal areas, but no involvement of the crural area.
The etiology of papular acantholytic dyskeratosis remains unclear. Indeed, a range of different etiologies have been postulated: hormonal, viral infections, Candida and physical factors, though they have not been proven scientifically. The lesions in this case first appeared 2 months after a spontaneous delivery, which likely indicates that hormonal alterations could be involved in the etiology. Recent evidence suggests that papular acantholytic dyskeratosis of the vulva may be caused by genetic mutations that are more closely related to Hailey–Hailey disease and that papular acantholytic dyskeratosis of the vulva is allelic to Hailey–Hailey disease.3 The diagnosis of papular acantholytic dyskeratosis could be challenging if one is not aware of this entity.
Alternative diagnoses include Darier disease, Grover’s disease, and warty dyskeratoma. The histologic features of papular acantholytic dyskeratosis are acantholysis which may involve the full thickness of the epidermis and dyskeratosis with corps ronds and grains. Hyperkeratosis and parakeratosis are also found. These features resemble Hailey–Hailey disease, Darier disease and Grover’s disease and thus, the clinical appearance is essential to distinguish papular acantholytic dyskeratosis from these diseases. Hailey–Hailey disease presents with painful superficial blisters and scaly erythematous plaques in the intertriginous areas. Darier disease is characterized by warty papules and plaques in seborrheic areas. In addition, Hailey–Hailey disease and Darier disease are skin diseases with a dominant inheritance and therefore the lack of a family history and skin lesions elsewhere on the body help distinguish papular acantholytic dyskeratosis from these conditions. Grover’s disease affects the trunk, neck, and proximal limbs, but there have been no reports of Grover’s disease affecting the genital area.2
Effective treatment of papular acantholytic dyskeratosis of the vulva and perianal area is a challenge. The lesions tend to persist for years. Successful treatment with topical and systemic steroids has been reported, but some reports also describe their failure in treating the condition.4 CO2 laser has been shown to be effective in a rare case involving the vulva.5 Our patient was treated with topical desonide and had alleviation of symptoms but the lesions persisted.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Is papular acantholytic dyskeratosis of the vulva a new entity? Am J Dermatopathol. 1984;6:557-60.
- [CrossRef] [Google Scholar]
- Papular acantholytic dyskeratosis of the anogenital and genitocrural area: Case series and review of the literature. J Cutan Pathol. 2016;43:749-58.
- [CrossRef] [Google Scholar]
- Genitoperineal papular acantholytic dyskeratosis is allelic to Hailey-Hailey disease. Br J Dermatol. 2012;167:210-2.
- [CrossRef] [Google Scholar]
- Papular acantholytic dyskeratosis of the vulva. Clin Exp Dermatol. 2001;26:386-8.
- [CrossRef] [Google Scholar]
- Successful laser therapy of a papular acantholytic dyskeratosis of the vulva: Case report and review of literature. Arch Gynecol Obstet. 2010;281:723-5.
- [CrossRef] [Google Scholar]





