Translate this page into:
Photoprotection and vitamin D status: A study on awareness, knowledge and attitude towards sun protection in general population from Kuwait, and its relation with vitamin D levels
2 Department of Dermatology, Farwaniya Hospital, Kuwait
Correspondence Address:
Nawaf Al-Mutairi
Post box No. 280, Farwaniya 80000
Kuwait
| How to cite this article: Al-Mutairi N, Issa BI, Nair V. Photoprotection and vitamin D status: A study on awareness, knowledge and attitude towards sun protection in general population from Kuwait, and its relation with vitamin D levels. Indian J Dermatol Venereol Leprol 2012;78:342-349 |
Abstract
Background: The primary cause of skin cancers is exposure to ultraviolet (UV) radiation. And, for decades sun protection has been promoted in various public health education campaigns. Recently, however, vitamin D deficiency has been related to increased risk of skin cancers. And, skin being the primary site for the synthesis of active form of vitamin D, excessive sun protection could lead to vitamin D-deficient states. But, the results have so far been conflicting. Aims: To study the level of awareness, knowledge and attitude of representative groups from the general population from Kuwait towards sun protection. And, also study the correlation of the level of sun protective measures used and vitamin D levels in these groups. Methods: The study constituted of two main parts. First part comprised a questionnaire-based survey of representative group of people aged 18 and above to assess their knowledge, awareness and attitude towards sun protection. The second part consisted of measuring serum vitamin D levels in 150 volunteers amongst the responders of the questionnaire, who had been regularly using sunscreens for at least 2 years and compare to the levels seen in 150 age and sex-matched responders of similar skin phototypes, who had never used sunscreens. Results: Out of the total of 1044 responders, 80% of them had adequate knowledge of the beneficial and harmful effects of sun exposure, and had been using sunscreens regularly, and adopting other sun protective measures in their daily life. The levels of vitamin D were found to be deficient in both sunscreen users and those who had never used sunscreens. The difference between the two groups was statistically insignificant (60.67% vs 54.67%; P value>0.001). Conclusion: Population at large seems to be adequately informed about the beneficial and deleterious effects of sun exposure. Vitamin D levels are deficient in majority of our people, and there is a need to do larger surveys covering all parts of the country and give supplemental doses of vitamin D to those found deficient.Introduction
The role of ultraviolet (UV) radiation in causing sunburn, premature aging of the skin, development of skin cancers and cataracts, immune suppression and activation of latent viruses is very well known. [1] Some of the dermatoses that may be triggered or exacerbated by excessive exposure to ultraviolet radiation include actinic keratosis, basal cell skin cancer, squamous skin cancer, malignant melanoma, cutaneous lupus erythematosus, dermatomyositis, polymorphous light eruption and disseminated actinic porokeratosis. Chronic sun exposure leads to degenerative changes in the skin that are recognized as photoaging, immunosuppression and photocarcinogenesis. There is an increased risk of melanoma associated with sun exposure during the first 15 years of life and blistering and sunburns before age of 20 years.
On the contrary, sun exposure is also essential for the synthesis of vitamin D in humans [Figure - 1]. Ultraviolet-B irradiation on skin triggers photolysis of 7-dehydroxy cholesterol, which eventually is converted to biologically active 1, 25-dihyroxyvitamin D. This biologically active form of vitamin-D helps to regulate cell growth, prevent cancer progression by reducing angiogenesis, increasing cell differentiation and apoptosis of cancer cells and reducing cell proliferation and metastases.
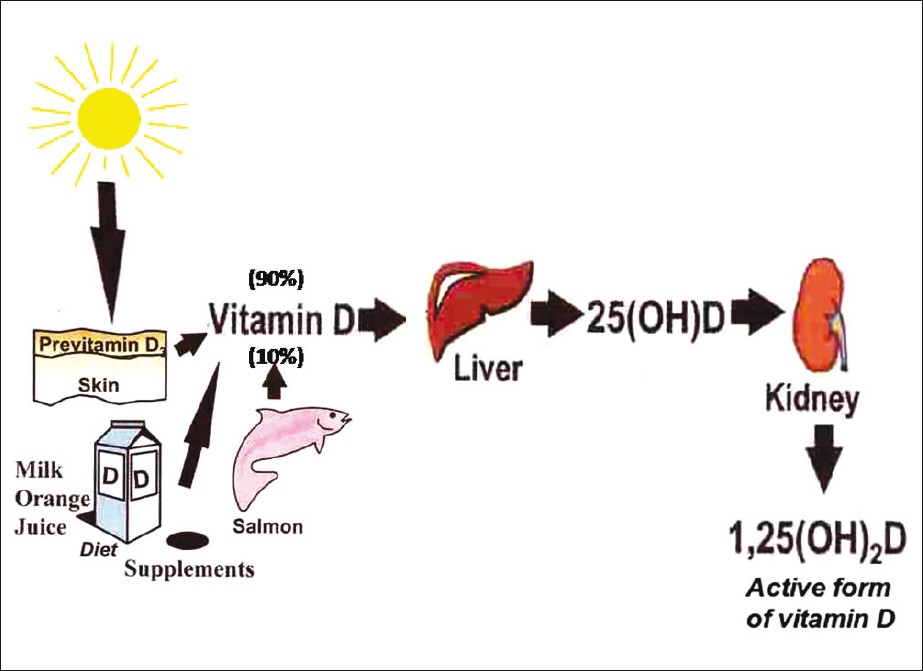 |
| Figure 1: Showing Vitamin D synthesis pathway in human body in skin and liver and its activation in kidney |
Many people are unaware of the association of sun exposure and vitamin D synthesis. Hence encouraging photoprotection and improving the awareness about the harmful effects of too much or very less sun exposure should be one of the leading Preventative Health Strategy.
Recently, there have been reports of vitamin D deficiency in epidemic proportions in this part of the world. [2],[3] It has been reported in all the age groups starting from healthy children, young adults, middle aged and elderly adults. [4],[5]
The use of sunscreen with a sun protection factor (SPF) of eight inhibits more than 95% of vitamin D production in the skin. [6],[7] And, with the rampant use of broad spectrum sunscreens in our population with mostly skin type III-V, who are already overprotected from sun, due to the clothing habits, we suspect vitamin D levels to be low in our population. In view of the fact, that there are no special programs or interventions available at the national level, to study sun protective awareness in our population, we undertook this study to investigate the knowledge of various representative groups of our people about the positive and negative effects of UV rays on the skin. And also, to estimate the vitamin D levels in the studied population to find out the association of vitamin D with the extent of sun exposure.
Methods
The study constituted of two main parts.
- First part comprised of a questionnaire-based survey of representative group of people aged 18 and above to assess their knowledge, awareness and attitude towards sun protection.
- The second part consisted of measuring serum vitamin D levels in 150 volunteers among the responders of the questionnaire, who had been regularly using sunscreens and compare it with the levels seen in 150 age and sex-matched responders of similar skin phototype having comparable daily outdoor activities, who had never used sunscreens.
In the first part a descriptive questionnaire [Table - 1] based survey was conducted amongst the people aged between 18 and 50 years, randomly selected from the Dermatology outpatient clinic of Farwaniya Hospital, between April 2011 and October 2011, belonging to representative groups of our population. The participation was on purely voluntary basis. And the study was approved by our hospital′s ethics committee. The questionnaire was made so as to elicit and assess the sun protection behavior as well as attitude towards the use of sun protective measures, knowledge of skin cancer and awareness of recommended solar protection behavior of each participant.
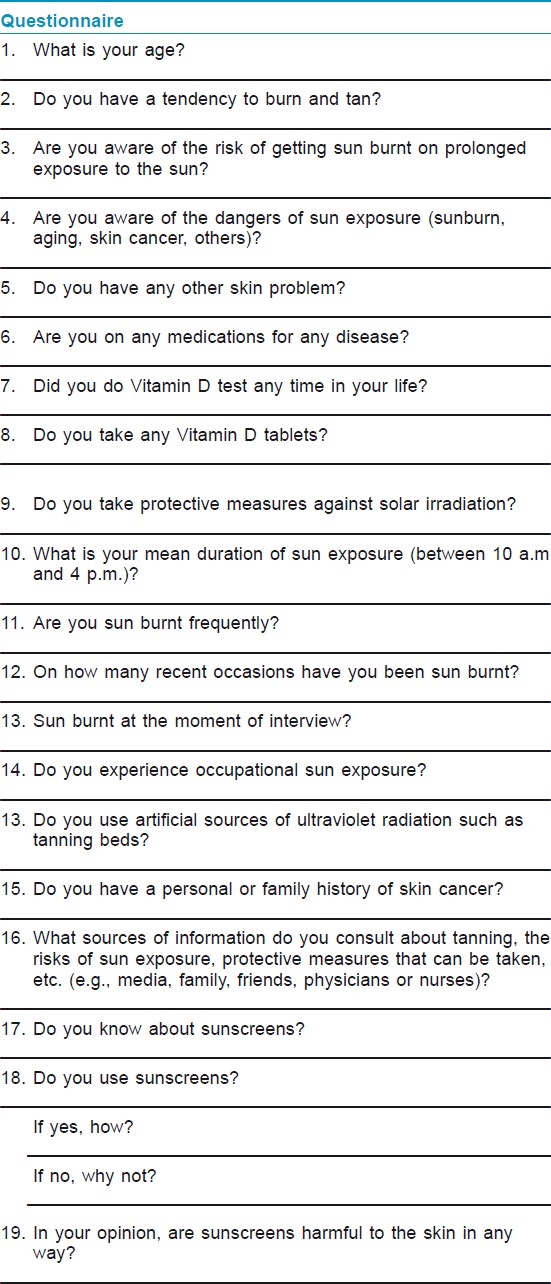
The questionnaire consisted chiefly of close-ended questions, and was used to collect information on the socio-demographic characteristics of the participants, such as age, sex, educational qualifications, profession, marital status and nationality [Table - 2]. The questionnaire then went on to assess their knowledge about sun sensitivity, their attitude toward sun protection and sun exposure hazards, the use of sunscreen and the pattern of its application (frequency of application and the surface of body covered), and its SPF. Participants were also asked about the source of information regarding the importance of sun protection.
An informed consent was signed by each subject included in this study. Every effort was made to ensure that the selected participants belonged to the population groups representing a cross-section of our society. And it included college students, house wives, teachers, businessmen (both with mainly indoor and mainly outdoor work), army personnel and sailors and people working at sea/sea front, in addition to doctors and nurses. All the participants were at least graduates, and belonged to different socioeconomic background. Apart from the demographic details Fitzpatrick skin photo type (SPT), eye color and hair color were also noted. Demographic data and related study variables were analyzed using descriptive statistics.
In the second phase of the study, blood samples were collected from 150 volunteers amongst the responders with daily outdoor activity who used daily sunscreen (SPF=15-50) continuously for at least the past 2 years and 150 others with matched age, sex, skin photo types and comparable daily outdoor activity but had never used sunscreens. These samples were then analyzed for 25 OH D levels to determine the impact of sun screen usage on vitamin D levels. Enzyme-linked immunosorbent assay (ELISA) was done for the quantitative determination of 25-hydroxyvitamin D, and other hydroxylated metabolites in serum or plasma. Selected monoclonal antibody recognizing 25, OH vitamin D was utilized in assay using competitive ELISA technique. And, for 1, 25 OH Vitamin D, competitive Enzyme-Immuno-Assay (EIA) technique with a selected monoclonal antibody was utilized. The samples which were assayed for 1, 25-dihydroxy vitamin D were incubated with the detection antibody after the extraction step. The preincubated solution was then transferred to the microplate coated with 1, 25-dihydroxy vitamin D. During this incubation step, 1,25-dihydroxy vitamin D in the sample and a fixed amount of 1,25-dihydroxy vitamin D bound to the microtiter competed for the binding to the detection antibodies. Peroxidase-conjugated anti-mouse antibody was then added into each microplate well, forming a complex of 1, 25-dihydroxy vitamin D - detection antibody - peroxidase conjugate. Tetramethylbenzidine (TMB) was used as a peroxidase substrate. Finally, to terminate the reaction an acidic stop solution was added. [8] The data obtained was analysed with "Chi square" test using SPSS 10.0 software.
Results
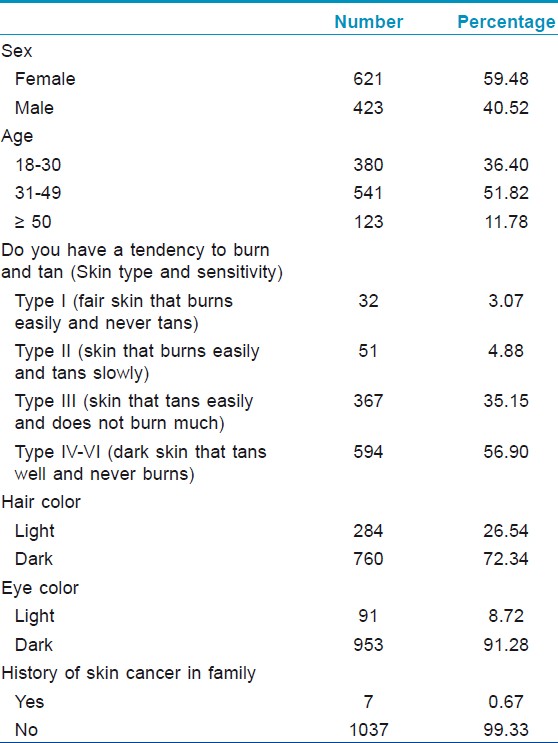
In total, 1044 Participants completed this survey, with notably more females (n=621; 59.48%) than males (n=423; 40.52%), with a mean age of 32.57 ± 12.25 years. The most common age groups being 31-49 years old group (354 females and 187 males, accounting for 57% and 44.21%).
Thirty eight participants (3.64%) had skin type I, 140 (13.41%) participants had skin type II, 411 (39.37%) participants had skin type III, and 455 (43.58%) participants had skin type between IV-VI [Table - 2]. Seven (0.9%) participants gave a history of skin cancer in their family.
Four hundred and six (38.89%) participants reported once weekly exposure to sun more than one hour between 10.00 am and 4.00 pm, 332 (31.80%) reported exposure on 2-3 days/week, and 183 (17.53%) reported exposure on more than 3 days/week. One hundred and twenty-three (11.78%) participants noted that they did not expose themselves to sunshine between 10 am and 4 pm, and all of them were females [Table - 3]. Sun exposure on more than 3 days/week was considerably more in male group in age group 18-30 years, than in females and more probably than the older age groups. The skin type and the level of education of the participants showed no relationship with the frequency of the time of sun exposure through peak hours of sunshine.
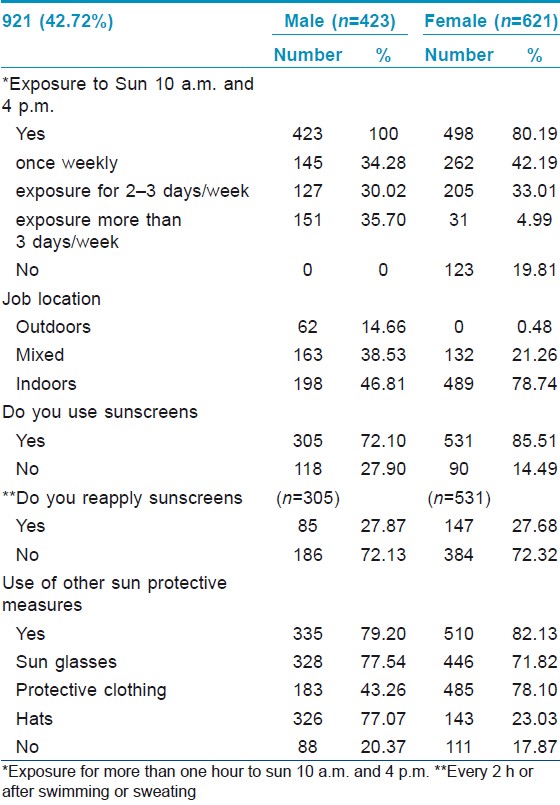
[Table - 3] also shows the various protective measures taken against sun exposure. Overall, 836 (80.08%) of the participants used a sunscreen. Sunscreen use was a popular protective measure in the female group: 531 of 621 (85.51%) used sunscreen. Only 232 of the 836 sunscreen users (27.75%) noted regular reapplication of sun screens (every 2 h or after swimming or sweating).
Sixty-two (5.94%) mentioned an occupational exposure (all were men and no women) due to the outdoor nature of their jobs. Twenty-four participants claimed working in the sun for 1-3 h/d, and 38 claimed working in the sun for more than 3 h/d. Sunscreen use was reported by only 14 of these 62 men. The rest of them depended on protective clothing as a protective measure against sun exposure. Spending more hours in the sun whilst at work was not connected with regular use of a sunscreen.
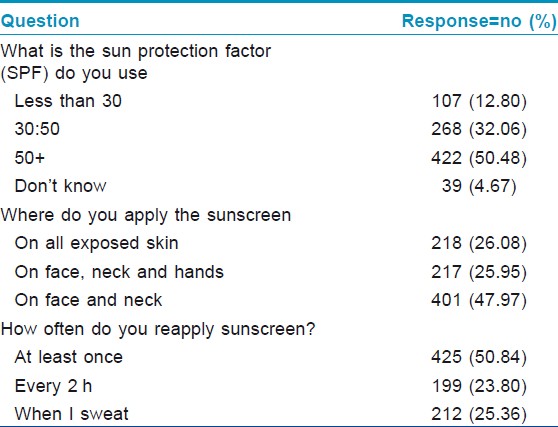
Among other protective measures, 774 (74.14%) of participants commonly wore sunglasses, 469 (44.92%) wore hats, while 668 (63.98%) of them used protective clothing. A sum of 199 (19.06%) of the 1044 participants did not use any protective measure at all. Hats were more accepted in males, 42.1% vs. 20%. One hundred and seven (12.80%) of the 836 sunscreen users, reported using SPF less than 30, 268 (32.06%) reported using an SPF of 30-50, and 422 (50.48%) reported using an SPF of more than 50, while 39 (4.67%) did not know the SPF they were using [Table - 4]. Use of an SPF greater than 50 was more common in females (1.7:1), with no association to the age, or skin sensitivity.
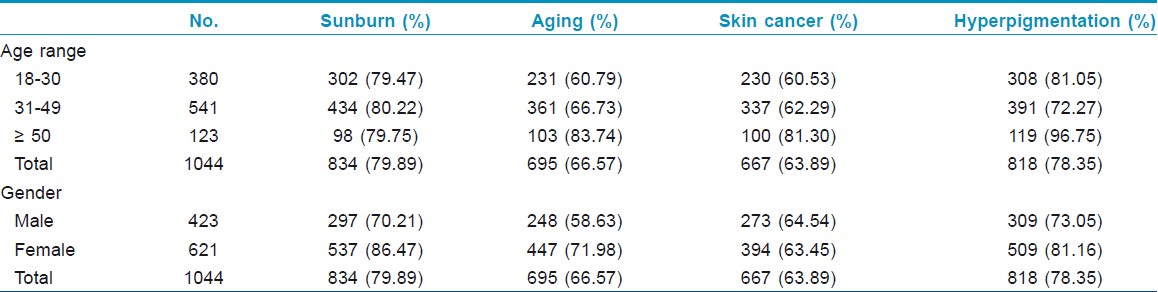
Nearly all of the participants (95.98%) knew that solar radiation is harmful; especially females. Eight hundred and thirty-four participants (79.89%) agreed that they are aware of the risk of getting sun burnt on prolonged exposure to the sun. [Table - 5] shows sun exposure risk awareness in relation to age and gender. Six hundred and ninety-five (66.57%) participants recognized the risk of sun exposure on skin aging, 667 (63.89%) of skin cancer and hyperpigmentation risk in 818 (78.35%) subjects. There were no major differences regarding the knowledge of sun exposure awareness risk factors between the different age groups
The awareness of sun risk percentages was higher in the female participants than in males, respectively, 86.47% and 68.75% for sunburn, 71.98% and 57.41% for skin aging and 81.16% and 71.53% for hyperpigmentation. Awareness for skin cancer risk was approximately equal.
The last part of the survey discussed the awareness about sun protection and vitamin D levels. About 80% (827; 79.21%) of participants agreed that sun exposure was required for maintaining vitamin D level. Six hundred and twenty-two (59.58%) participants indicated that more than 10 minutes in the sun was required to get enough vitamin D in summer. This idea was notably more common in males than in females. Seven hundred and ninety-nine (76.53%) of the participants agreed that sunscreen application lead to the danger of not getting enough vitamin D. Lastly, to the question regarding the source of information about the relation between sun protection and vitamin D production,716 (68.58%) of the participants replied that their source of information was the mass media (73.27% in female vs. 61.70% in male), 20.88% of the participants stated that their information was given by family or friends (22.06% in females vs. 19.15% in males), 19.54% got their information through a health professional (18.46% in female subjects vs. 21.04% in male subjects) and 9.00% said they have no distinct source (9.50% in female subjects vs. 8.27% in male subjects). Participants who assumed that sun protection might cause vitamin D deficiency reported a significantly lower incidence of sunscreen use.
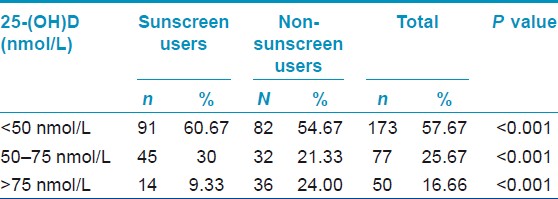
The second phase of our study which was to determine the association of vitamin D levels with the extent of sun exposure. Vitamin D-deficient concentrations were considered as those of <50 nmol/L); a level of 50-75 nmol/L) was considered to indicate vitamin D insufficiency, whereas a level of 75 nmol/L or greater was considered sufficient or optimum.
In our total sample of 184 of 300 subjects, (61.33% had 25-OHD insufficiency (96 of sunscreen users and 88 non-sunscreen users) and 71 (23.67%) had deficient concentrations (40 of sunscreen users and 21 non-sunscreen users) [Table - 6].
The age-wise comparison of mean serum concentration of vitamin D in both groups revealed that it was statistically significant among the younger age group (31-49 years; P=0.001).
Discussion
Kuwait is a small country situated in the north-east corner of the Arabian Peninsula. Located in the desert geographical region, Kuwait has a continental climate characterized by its dry hot long summer, and a short warm winter with occasional rainfall. The highest recorded temperature sometimes reaches 50°C under shadow in summer. Kuwait has one of the highest ultraviolet (UV) index scores in the world.
Protection against both UVA and UVB is very important, hence sun protection by clothes, avoiding sun exposure and proper use of sunscreens are important ways to diminish adverse solar radiation effects.
Sunscreens are proven to have encouraging effects on reducing the signs of aging and the frequency of skin cancers. Sunscreens can be classified according to their mechanism of action as physical sunscreens (inorganic agents) or chemical sunscreens (organic agents). Physical sunscreens reflect or scatter UVR. They contain inert minerals such as titanium dioxide or zinc oxide. Inorganic blockers are not well accepted as these agents are composed of opaque thick pastes that may lead to comedogenesis and could stain clothes. [9] Chemical sunscreens are generally aromatic compounds conjugated with a carbonyl group. Chemical sunscreens prevent the skin-damaging ultraviolet rays from reaching the skin. [10] Sunscreens alone may not provide satisfactory protection from UVR as they prevent sunburn from UV-B radiation and provide more limited protection from UV-A radiation. Experts advocate the use of sunscreen, as well as other sun-protective measures as wearing protective clothing, wearing wide-brimmed hats, and avoiding the sun, to protect persons from sun exposure. [11]
In our survey the vast majority of the participants knew that the sun can cause skin cancer and skin ageing, in agreement with other studies. [12],[13] In our study, men had a lesser knowledge level, for the importance of sun protection, and were less likely to use active sun-protective measures. Devos et al., [14] showed that these percentages were considerably higher in the female participant group than in the male group.
In our study, sunscreens were the most popular form of sun protection. Our study showed also that women reported higher sunscreen usage than men. Devos et al., [14] showed that sunscreen use was the most popular preventive behavior in Belgian beachgoers. Also a study by Halpern et al., [13] performed in Western Europe, Australia and the USA, 85% of the responders declared that they always took precautions against UV exposure and that sunscreens were the most popular form of sun protection. Persons who did not use sunscreen tended to be older and of male gender.
Mass media was the main source of information, as in other studies. [15] A low proportion of patients affirmed that they had been informed about sun protection by health professional. Former studies in the general population showed similar low percentages. [13],[14]
We also assessed knowledge and attitudes about vitamin D. About 80% of the participants agreed that sun exposure is required for maintaining vitamin D level. A study performed by Vu LH et al., [16] showed that high proportion of people were unaware that sun exposure leads to formation of vitamin D, and that only 11% of their sample believed that sun protection might lead to a lack of vitamin D. Over half of the participants (59.58%) indicated that more than 10 minutes in the sun was needed to attain enough vitamin D in summer.
Cholecalciferol (vitamin D3) is synthesized in the skin by exposure to UV light between 290 and 315 nm. [17] Melanin, which is the principal skin pigment, and is found abundantly in people with skin of color can reduce the synthesis of cholecalciferol. Vitamin D deficiency leads to skin cancer, increases blood pressure and increases the risk of autoimmune disease. [18] Some type of sun screens and/or very low level of sun exposure may lead to vitamin D deficiency. [18]
The second leg of our study was designed to assess whether people in Kuwait, who are exposed to high amounts of sun throughout the year have adequate levels of vitamin D. However, we documented vitamin D deficiency and insufficiency in both sunscreen and non sunscreen users. Our study revealed that vitamin D deficiency is common among both groups (60.67% of sunscreen users to 54.67% of non- sunscreen users). According to our results we assume that sunscreen use does not really influence vitamin D production in a population setting. Marks et al. [19] found no difference in 25OHD between sunscreen users and placebo in a randomized controlled trial of 7 months duration. In this follow-up study of long-term sunscreen users, it has been shown that sunscreen does not play a role in the development of vitamin D insufficiency or deficiency.
The reason for vitamin D deficiency seen in our study may be due to the high outside temperatures during most part of the year, which limits outdoor activity. In addition to this both genders traditionally wear a type of clothing which covers most of the body parts. Unexplained vitamin D deficiency has earlier been reported in women and children from Kuwait. [20],[21] In 1996 El-Sonbaty et al., [20] studied 50 veiled volunteer Kuwaiti women aged between 14 and 45 years old who had three children or less, and 22 unveiled volunteer Kuwaiti women with matched age and number of children as control. The results showed subclinical vitamin D deficiency among veiled women. Also, 2 cases of clinically overt osteomalacia were discovered among the veiled volunteers, suggesting a high prevalence of the disease among veiled Kuwaiti women.
In Lebanese women veil wearing and high parity were predictors of hypovitaminosis D. [22],[23] It is also well established in the general population from the gulf region. [24] ,[25] Women in Saudi Arabia and their children have high prevalence of osteomalacia and rickets, respectively, and vitamin D deficiency because of their practice of wearing clothing over the whole body and avoiding direct sunlight. [26],[27] A study from the United Arab Emirates in 2003 showed that hypovitaminosis D is common in summer in exclusively breast-feeding infants and their mothers. [28] Several studies from Qatar revealed that Qatari children are at high risk for vitamin D deficiency and are more common in Qatari girls. [29],[30],[31],[32] Lack of exposure to sunlight, outdoor activities under the sun, and physical activity and vitamin D intake are the main associated factors for vitamin D deficiency in the young population of Qatar.
In Iran 81.3% of the population within the age group 20 to 64 suffer vitamin D insufficiency. A cross-sectional study was done in Isfahan, Iran. Serum 25-hydroxy vitamin D (25-OHD), parathyroid hormone (PTH), calcium and phosphorus concentrations were measured in 1,111 healthy people-243 men and 868 women aged 41.4 (mean 14 and range 20-80) years. The prevalence of vitamin D deficiency was high in this sunny city (Isfahan) especially among women and younger population. [33] Studies from Morocco [34] and Tunisia [35] showed that vitamin D insufficiency is also very common in healthy adults in these Western Arab countries.
Conclusions
In our study, we found that the people in Kuwait have adequate knowledge, and are well aware about the useful as well as the harmful effects of sun exposure. They seem to have low levels of vitamin D in general but the levels are not influenced by regular usage of sunscreens, even of high SPF. It could be attributed to either insufficient dietary intake of vitamin D, decreased outdoor activities, higher delivery rate or protective clothing like veil. Considering the results, we recommend the encouragement of dietary enrichment or supplementation by vitamin D, and a more outdoor lifestyle with reasonable sun exposure (usually 5-10 min of exposure of the hands, arms, and face, two or three times per week) to reduce this deficiency in Kuwait.
Some of the food items rich in vitamin D include fatty fish species like cat fish, salmon, tuna; fish liver oils like cod liver oil; vitamin D fortified food products like packaged milk, juices, etc. The consumption of these items could be encouraged in the general population through media campaigns and other public awareness methods.
| 1. |
Ullrich SE. Sun exposure and the lupus patient. Lupus 2000;22:6-7.
[Google Scholar]
|
| 2. |
McKenna MJ. Differences in Vitamin D status between countries in young adults and elderly. Am J Med 1998;338:777-83.
[Google Scholar]
|
| 3. |
Matsuoka LY, Wortsman J, Haddad JG, Kolm P, Hollis BW. Racial pigmentation and the cutaneous synthesis of vitamin D. Arch Dermatol l991;127:536-8.
[Google Scholar]
|
| 4. |
McKenna MJ, Freany R. Secondary hyperparathyroidism in the elderly: Means to defining hypovitaminosis D. Osteoporos Int l998;8: S3-6.
[Google Scholar]
|
| 5. |
Krall EA, Sahyoun N, Tannenbaum S, Dallal GE, Dawsob-Hughes B. Effect of vitamin D intake on seasonal variations in parathyroid hormones secretion in postmenopausal women. N Engl J Med l989;321:1777-83.
[Google Scholar]
|
| 6. |
Kimlin MG, Schallhorn KA. Estimation of the human Vitamin D UV exposure in the USA. Photochem Photobiol Sci 2004;3:1067-70.
[Google Scholar]
|
| 7. |
Sayre RM, John CD. Darkness at noon: Sunscreens and Vitamin D3. Photochem Photobiol 2007;83:459.
[Google Scholar]
|
| 8. |
Hollis BW, Horst RL. The assessment of circulating 25(OH) D and l, 25 (OH) 2D: Where we are and where we are going? J Steroid Biochem Mol Biol 2007;103:473-6.
[Google Scholar]
|
| 9. |
Moloney FJ, Collins S, Gillian MM. Sunscreens: Safety, efficacy and appropriate use. Am J Clin Dermatol 2002;3:185-91.
[Google Scholar]
|
| 10. |
Lowe NJ. An overview of ultraviolet radiation, Sunscreens and photo-induced dermatoses. Dermatol Clin 2006;24:9-17.
[Google Scholar]
|
| 11. |
Hall HI, Jones SE, Saraiya M. Prevalence and correlates of sunscreen use among US high school students. J Sch Health 2001;71:453-7.
[Google Scholar]
|
| 12. |
Nikolaou V, Stratigos AJ, Antoniou C, Sypsa V, Avgerinou G, Danopoulou I, et al. Sun exposure behavior and protection practices in a Mediterranean population: A questionnaire-based study. Photodermatol Photoimmunol Photomed 2009;25:132-7.
[Google Scholar]
|
| 13. |
Halpern AC, Kopp LJ. Awareness, knowledge and attitudes to non-melanoma skin cancer and actinic keratosis among the general public. Int J Dermatol 2005;44:107-11.
[Google Scholar]
|
| 14. |
Devos SA, Baeyens K, Van Hecke L. Sunscreen use and skin protection behavior on the Belgian beach. Int J Dermatol 2003;42:352-6.
[Google Scholar]
|
| 15. |
Benvenuto-Andrade C, Zen B, Fonseca G, De Villa D, Cestari T. Sun exposure and sun protection habits among high-school adolescents in Porto Alegre, Brazil. Photochem Photobiol 2005;81:630-5.
[Google Scholar]
|
| 16. |
Vu LH, Van der Pols JC, Whiteman DC, Kimlin MG, Neale RE. Knowledge and attitudes about Vitamin D and impact on sun protection practices among urban office workers in Brisbane, Australia. Cancer Epidemiol Biomarkers Prev 2010;19:1784-9.
[Google Scholar]
|
| 17. |
Mac Laughlin JA, Anderson RR, Holick MF. Spectral character of sunlight modulates photosynthesis of previtamin D3 and its photoisomers in human skin. Science 1982;216:1001-3.
[Google Scholar]
|
| 18. |
Boland R. Role of vitamin D in skeletal muscle function. Endocr Rev 1986;7:434-48.
[Google Scholar]
|
| 19. |
Marks R, Foley PA, Jolley D, Knight KR, Harrison J, Thompson SC. The effect of regular sunscreen use on vitamin D levels in an Australian population. Arch Dermatol 1995;131:415-21.
[Google Scholar]
|
| 20. |
El-Sonbaty MR, Abdul-Ghaffar NU. Vitamin D deficiency in veiled Kuwaiti women. Eur J Clin Nutr 1996;50:315-8.
[Google Scholar]
|
| 21. |
Lubani MM, Al-Shab TS, Al-Saleh QA, Shanda DC, Quattawi SA, Ahmed SA, et al. Vitamin D deficiency rickets in Kuwait: The prevalence of a preventable disease. Ann Trop Paediatr 1989;9:134-9.
[Google Scholar]
|
| 22. |
Gannage-Yared MH, Chemali R, Halaby G. Hypovitaminosis D in a sunny country: Relation to lifestyle and bone markers. J Bone Miner Res 2000;15:1856-62.
[Google Scholar]
|
| 23. |
Gannage-Yared MH, Brax H, Asmar A, Tohme A. Vitamin D status in aged subjects. Study of a labanese population. Presse Med 1998;27:900-4.
[Google Scholar]
|
| 24. |
Elsammak MY, Al-Wosaibi AA, Al-Howeish A, Alsaeed J. Vitamin D deficiency in Saudi Arabs. Horm Metab Res 2010;42:364-8.
[Google Scholar]
|
| 25. |
Sadat-Ali M, Alelq A, Al-turki H, Al-mulhim F, Al-ali A. Vitamin D levels in healthy men in eastern Saudi Arabia. Ann Saudi Med 2009;29:378-82.
[Google Scholar]
|
| 26. |
Taha SA, Dost SM, Sedrani SH. 25-Hydroxyvitamin D and total calcium: Extraordinarily low plasma concentrations in Saudi mothers and their neonates. Pediatr Res 1984;18:739-41.
[Google Scholar]
|
| 27. |
Sedrani SH. Low 25-hydroxyvitamin D and normal serum calcium concentrations in Saudi Arabia: Riyadh region. Ann Nutr Metab 1984;28:181-5.
[Google Scholar]
|
| 28. |
Dawodu A, Agarwal M, Hossain M, Kochiyil J, Zayed R. Hypovitaminosis D and vitamin D deficiency in exclusively breast-feeding infants and their mothers in summer: A justification for vitamin D supplementation of breast-feeding infants. J Pediatr 2003;142:169-73.
[Google Scholar]
|
| 29. |
Bener A, Al-Ali M, Hoffmann GF. High prevalence of vitamin D deficiency in young children in a highly sunny humid country: A global health problem. Minerva Pediatr 2009;61:15-22.
[Google Scholar]
|
| 30. |
Bener A, Al-Ali M, Hoffmann GF. Vitamin D deficiency in healthy children in a sunny country: Associated factors. Int J Food Sci Nutr 2009;60 Suppl 5: S60-70.
[Google Scholar]
|
| 31. |
Bener A, Alsaied A, Al-Ali M, Al-Kubaisi A, Basha B, Abraham A, et al. High prevalence of vitamin D deficiency in type 1 diabetes mellitus and healthy children. Acta Diabetol 2009;46:183-9.
[Google Scholar]
|
| 32. |
Bener A, Alsaied A, Al-Ali M, Hassan AS, Basha B, Al-Kubaisi A, et al. Impact of lifestyle and dietary habits on hypovitaminosis D in type 1 diabetes mellitus and healthy children from Qatar, a sun-rich country. Ann Nutr Metab 2008;53:215-22.
[Google Scholar]
|
| 33. |
Hovsepian S, Amini M, Aminorroaya A, Amini P, Iraj B. Prevalence of vitamin D deficiency among adult population of Isfahan City, Iran. J Health Popul Nutr 2011;29:149-55.
[Google Scholar]
|
| 34. |
Allali F, El Aichaoui S, Khazani H, Benyahia B, Saoud B, El Kabbaj S, et al. High prevalence of hypovitaminosis D in Morocco: Relationship to lifestyle, physical performance, bone markers, and bone mineral density. Semin Arthritis Rheum 2009;38:444-51.
[Google Scholar]
|
| 35. |
Meddeb N, Sahli H, Chahed M, Abdelmoula J, Feki M, Salah H, et al. Vitamin D deficiency in Tunisia. Osteoporos Int 2005;16:180-3.
[Google Scholar]
|
Fulltext Views
6,640
PDF downloads
3,592





