Translate this page into:
Porokeratosis confined to the genital area: A report of three cases
Correspondence Address:
Sujata Sengupta
UV 24/3C, Udayan, 1050/1, Survey Park, Kolkata - 700 075, West Bengal
India
| How to cite this article: Sengupta S, Das JK, Gangopadhyay A. Porokeratosis confined to the genital area: A report of three cases. Indian J Dermatol Venereol Leprol 2008;74:80 |
Abstract
Genital involvement in porokeratosis (PK) is a rare occurrence even in disseminated forms. We encountered three patients who had porokeratosis affecting only the genital area. Two of them were male with involvement of the penis and scrotum and only the scrotum respectively. The lady with vulvar involvement is a hitherto unreported instance of porokeratosis confined to female genitalia. None of the cases were very easy to diagnose clinically but biopsies proved confirmatory. The male patients were advised light electrocautery under local anesthesia while the female patient underwent surgical excision. No malignant change has been reported in them till date. |
| Figure 5: Keratotic depigmented plaque on scrotum |
 |
| Figure 5: Keratotic depigmented plaque on scrotum |
 |
| Figure 4: Porokeratosis on scrotum |
 |
| Figure 4: Porokeratosis on scrotum |
 |
| Figure 3: Annular plaques of porokeratosis on penis and scrotum |
 |
| Figure 3: Annular plaques of porokeratosis on penis and scrotum |
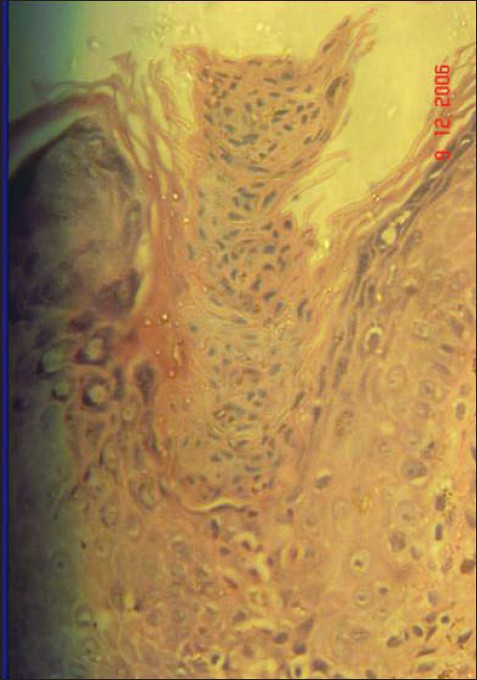 |
| Figure 2: Cornoid lamella with underlying hypogranulosis (H and E stain, X400) |
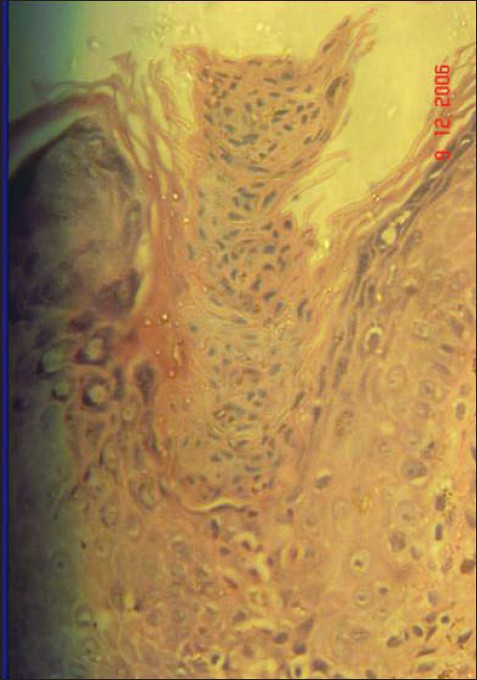 |
| Figure 2: Cornoid lamella with underlying hypogranulosis (H and E stain, X400) |
 |
| Figure 1: Vulvar porokeratosis |
 |
| Figure 1: Vulvar porokeratosis |
Porokeratosis (PK) is a clonal disorder of keratinization showing one or multiple atrophic patches surrounded by a distinct ridge-like border. The common clinical variants include classical plaque-type porokeratosis of Mibelli (PM), disseminated superficial porokeratosis, linear porokeratosis, porokeratosis palmaris et plantaris disseminate and punctate porokeratosis. [1] Genital porokeratosis (GP), though uncommon, can occur as a part of a more generalized involvement. [2] But PK localized to the genital area is a rare entity. We report such an occurrence in one female patient and two male patients.
Case Reports
Case 1
A 36-year-old housewife from a rural socioeconomic background presented with a dry, itchy vulvar lesion for the last 8 months. There was no history of sexual promiscuity or local irradiation and her family history was not significant. Topical steroids, antifungal and antibiotic creams had yielded no results. A hyperkeratotic verrucous plaque, 2 x 1.5 cm, was seen involving the vestibule, fourchette and adjacent perineal skin [Figure - 1]. No similar skin lesion was present anywhere else in her body and systemic examination was normal. Histology from the edge of the skin lesion showed a parakeratotic column (cornoid lamella) in the epidermal invagination and underlying hypogranulosis [Figure - 2]. A mild perivascular infiltrate was seen in the dermis. She was diagnosed to have vulvar PK. She was advised surgical excision.
Case 2
A 35-year-old businessman presented with slowly spreading multiple asymptomatic brownish lesions on the scrotum and penis for the last 8 months. There was no history of extramarital sexual exposure, drug intake; and his family history was noncontributory. Topical and systemic steroids had produced no results. Several well-defined hyperpigmented annular plaques of varying sizes were seen on the penile shaft and scrotum [Figure - 3]; each one had a mildly scaly atrophic center and a raised border [Figure - 4]. The rest of the skin and systemic examination was normal. We initially considered the genital lesions to be annular lichen planus (LP), but a biopsy was advised. Histopathology was typical of PK with the cornoid lamella and epidermal invagination.
Case 3
A 34-year-old man reported with an asymptomatic plaque on the scrotal skin for the last 3 months. It had started as a small papule, which expanded slowly to its present size. His family and sexual history was not significant. He had a 1.5 x 1 cm depigmented annular keratotic plaque on the scrotal skin that was surrounded by a raised border [Figure - 5]. On close inspection, the border was found to be traversed by a groove. Skin biopsy was consistent with PK. The lesion healed, with a thin scar, after electrodesiccation under local anesthesia.
None of the three patients had inguinal adenopathy or any evidence of sexually transmitted disease (STD). Routine hematological and biochemical tests were normal and VDRL and ELISA for HIV were negative. Till date, malignant change has not been seen.
Discussion
PK confined to the genital area is rarely seen. We came across about 20 such cases in English literature. [3] Surprisingly, all the cases were males. PK is two to three times more common in males than in females, but GP in females seems even rarer. Robinson et al, [4] gave the first report of vulvar PK in a 39-year-old lady who had disfiguring lesions in the perineal area, medial thigh and sole. But our report of the female patient is probably the first report of PK confined to female genitalia.
PK localized to the male genitalia has been reported most commonly in the scrotum, followed by penis, buttock, natal cleft, groins and adjacent thighs. [3] Porter et al, [5] came across a case involving the external urethral meatus that was treated with topical 5-fluorouracil. In our cases PK was localized to the penis and/or scrotum and involvement of skin adjacent to genitalia was not seen. Though the inheritance of PK is known to be autosomal dominant, none of our cases had a positive family history. Similarly, family history was noncontributory in all the 10 cases studied by Chen and his colleagues. [3] In contrast to their study, none of our patients had diabetes or sexually transmitted diseases (STDs). Malignant transformation into squamous or basal cell carcinoma has been seen in almost all forms of PK. [6] We have earlier reported multicentric squamous cell carcinoma (SCC) of the inguinal lesions of disseminated PK. [7] But that patient did not have genital lesions. In fact, malignant change has not been found in GP till date. [8]
Clinically, none of the cases were very easy to diagnose. We thought of condyloma acuminata in Case 1; but there was no sexual promiscuity and the response to imiquimod was unsatisfactory. This uncommon verrucous form of PK has been reported to occur over scrotum and buttocks. [3],[9] In Case 2, the annular plaques had raised borders but no typical ridge was seen. We considered lichen planus but extragenital or oral lesions were not seen. Annular syphilide was another possibility but VDRL was negative. A distinct keratotic ridge helped to diagnose Case 3 even though the center was depigmented.
The treatment options of GP are cryotherapy (liquid N 2 ), surgery, CO 2 laser, topical 5% 5-fluorouracil and imiquimod cream. [2],[5],[10] We found that all our patients had been previously treated for GP with either antifungals or topical and systemic steroids. This highlights the possibility that PK confined to the genital area is an under-diagnosed entity and can be easily confused with STDs and other nonvenereal diseases affecting genitalia. A thorough clinical evaluation is mandatory and skin biopsy may be diagnostic in such cases. In addition, keeping in mind the potential for malignancy, all diagnosed cases should receive regular follow-up.
| 1. |
Spencer LV. Porokeratosis. Available from: http://www.emedicine.com/derm/topic 343htm. [Last accessed on 2006 Oct 9].
[Google Scholar]
|
| 2. |
Levell NJ, Bewly AP, Levene GM. Porokeratosis of Mibelli on the penis, scrotum and natal cleft. Clin Exp Dermatol 1994;19:77-8.
[Google Scholar]
|
| 3. |
Chen TJ, Chow YC, Chen CH, Kuo TT, Hong HS. Genital porokeratosis: A series of 10 patients and review of the literature. Br J Dermatol 2006;155:325-9.
[Google Scholar]
|
| 4. |
Robinson JB, Im DD, Jockle G, Roshenshein NB. Vulvar porokeratosis: Case report and review of literature. Int J Gynecol Pathol 1999;18:169-73.
[Google Scholar]
|
| 5. |
Porter WM, Du P Menagι H, Philip G, Bunker CB. Porokeratosis of the penis. Br J Dermatol 2001;144:643-4.
[Google Scholar]
|
| 6. |
Judge MR, McLean WH, Munro CS. Disorders of keratinization. In : Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook Of Dermatology. 7 th ed. Blackwell Science: Oxford; 2004. p. 34.1-34.111.
th ed. Blackwell Science: Oxford; 2004. p. 34.1-34.111.'>[Google Scholar]
|
| 7. |
Sengupta S, Das JK, Gangopadhyay A. Multicentric squamous cell carcinoma over lesions of porokeratosis palmaris et plantaris disseminata and giant porokeratosis. Indian J Dermatol Venereol Leprol 2005;71:414-6.
[Google Scholar]
|
| 8. |
Neri I, Marzaduri S, Passarini B, Patrizi A. Genital porokeratosis of Mibelli. Genitourin Med 1995;71:410-1.
[Google Scholar]
|
| 9. |
Wallner JS, Fitzpatrick JE, Brice SL. Verrucous porokeratosis of Mibelli on the buttocks mimicking psoriasis. Cutis 2003;72:391-3.
[Google Scholar]
|
| 10. |
Agarwal S, Berth Jones J. Porokeratosis of Mibelli. Br J Dermatol 2002;146:338-9.
[Google Scholar]
|
Fulltext Views
3,278
PDF downloads
2,459





