Translate this page into:
Recurrent ulcers in the flexures of a 48-year-old woman
2 Department of Pathology, Care Institute of Medical Sciences, Hyderabad, Telangana, India
Correspondence Address:
Laxmi Chandravathi Penmetcha
Department of Dermatology, Care Institute of Medical Sciences, Road No. 10, Banjara Hills, Hyderabad - 500 034, Telangana
India
| How to cite this article: Penmetcha LC, Awake P, Fonseca A. Recurrent ulcers in the flexures of a 48-year-old woman. Indian J Dermatol Venereol Leprol 2016;82:740-743 |
A 48-year-old woman presented with a 4-year history of recurrent painful erythematous ulcerated lesions in with purulent secretion along with fibrosis and adhesions in her right axilla [Figure - 1]a and multiple severe ulcers in both groins disabling the mobility of limbs [Figure - 1]b. The remainder of the mucocutaneous examination including hair, nails, teeth and mucosae was normal.
 |
| Figure 1: (a) Erythematous ulcers with adhesions in the right axilla. (b) Multiple severe ulcers in both groins |
There were no costitutional symptoms. The patient had diabetes mellitus and hypertension. Systemic examination was normal. Serum biochemistry, lung function tests and, urine osmolality were all within normal limits. Bone marrow biopsy report showed no abnormality. Imaging studies were normal. A skin biopsy specimen was obtained from the lesions.
Histopathological examination revealed a nodular infiltrated lesion in dermis. The overlying epidermis was ulcerated and the dermis showed a lesion composed of ovoid cells with moderate amounts of eosinophilic cytoplasm and an indented reniform nucleus with an admixed cellular inflammatory infiltrate of neutrophils, eosinophils and mast cells [Figure - 2]a and [Figure - 2]b. On immunohistochemical study, the tumoral cells showed strong cytoplasmic positivity for CD1a and were negative for CD 68 [Figure - 3].
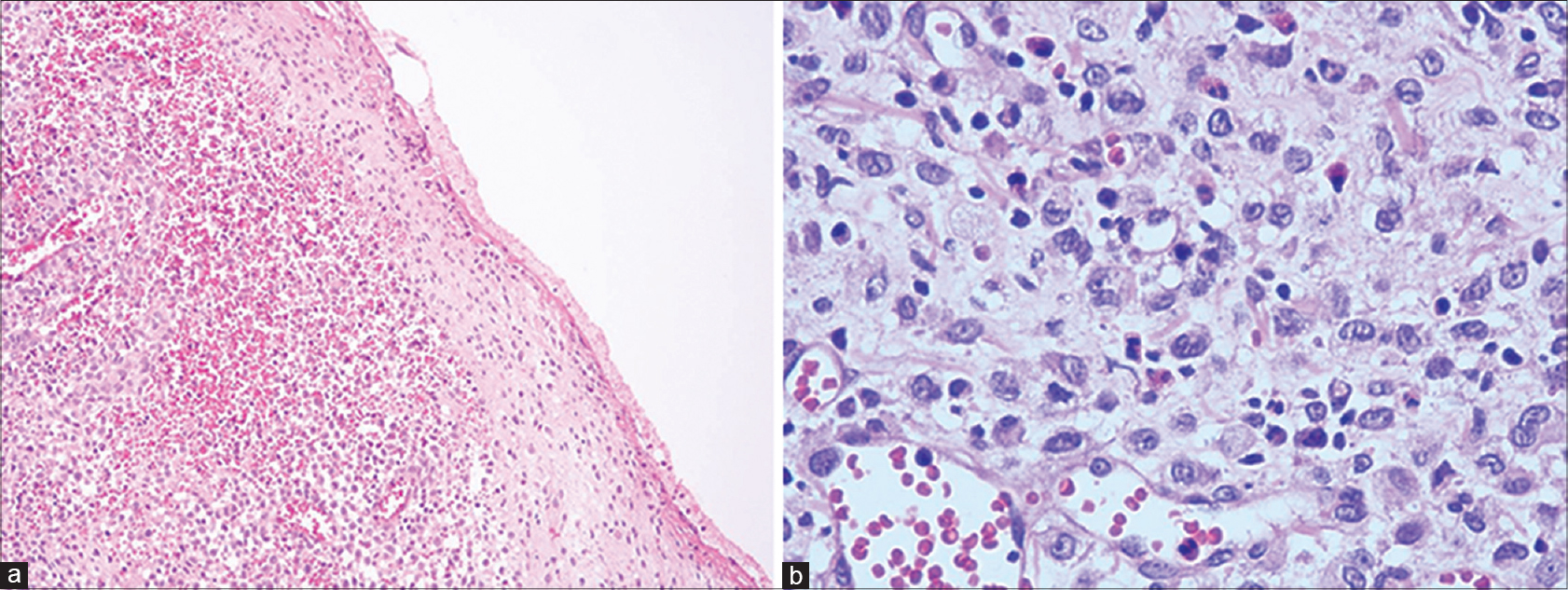 |
| Figure 2: (a) Nodular infiltrated lesion in dermis with ulcerated overlying epidermis (H and E, ×10). (b) Ovoid cells with moderate amounts of eosinophilic cytoplasm and an indented reniform nucleus with an admixed cellular inflammatory infiltrate of neutrophils, eosinophils and mast cells (H and E, ×400) |
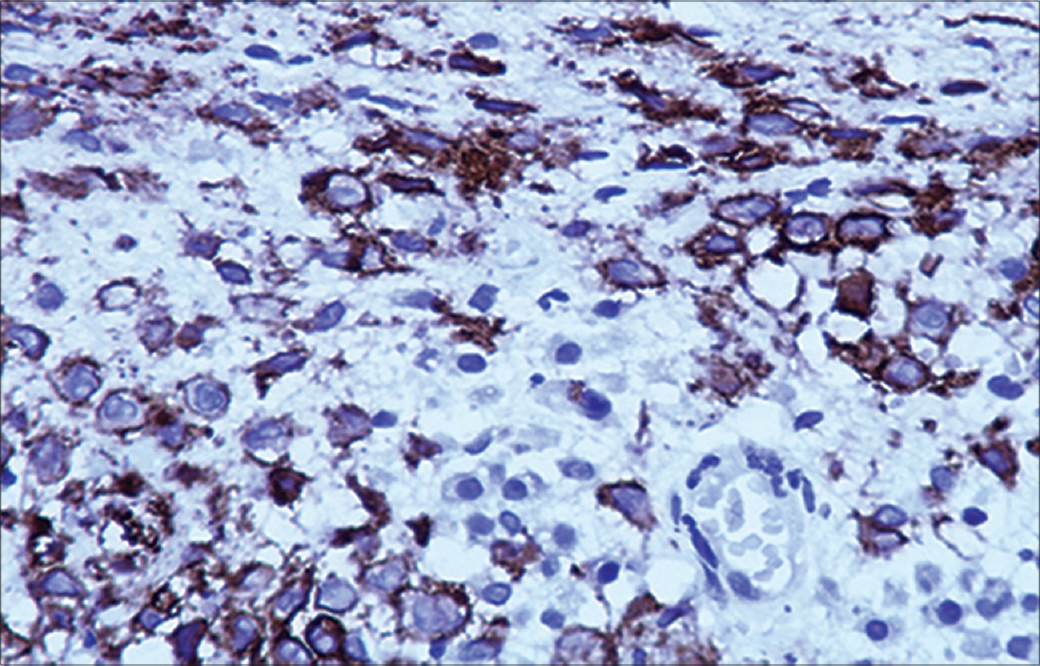 |
| Figure 3: Immunohistochemical staining is positive for CD1a (immunostain CD1a, ×100) |
What Is Your Diagnosis?
| 1. |
Pan Z, Sharma S, Sharma P. Primary Langerhans cell histiocytosis of the vulva: Report of a case and brief review of the literature. Indian J Pathol Microbiol 2009;52:65-8.
[Google Scholar]
|
| 2. |
Nezelof C, Basset F. An hypothesis Langerhans cell histiocytosis: The failure of the immune system to switch from an innate to an adaptive mode. Pediatr Blood Cancer 2004;42:398-400.
[Google Scholar]
|
| 3. |
Walia SS, Gayer K. An unusual presentation of refractory cutaneous Langerhans cell histiocytosis in an adult. J Drugs Dermatol 2006;5:174-7.
[Google Scholar]
|
| 4. |
Sander CS, Kaatz M, Elsner P. Successful treatment of cutaneous Langerhans cell histiocytosis with thalidomide. Dermatology 2004;208:149-52.
[Google Scholar]
|
| 5. |
Kolde G, Schulze P, Sterry W. Mixed response to thalidomide therapy in adults: Two cases of multisystem Langerhans' cell histiocytosis. Acta Derm Venereol 2002;82:384-6.
[Google Scholar]
|
Fulltext Views
2,272
PDF downloads
2,022







