Translate this page into:
Rickets in congenital ichthyosis: A case report and brief review
Corresponding author: Dr. Shibhani Sudheer Hegde, Department of Dermatology, Venereology and Leprosy, Bharati Vidyapeeth Medical College, Pune, Maharashtra, India. shibhani.s.hegde@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tuli S, Hegde SS, Sardesai VR, Dilkush R. Rickets in congenital ichthyosis: A case report and brief review. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_695_2024
Dear Editor,
Vitamin D deficiency remains a global health concern, particularly among children. Emerging evidence reports children with congenital ichthyosis face a greater risk with more severe deficiency, clinical and/or radiological evidence of rickets being observed in 41% of children with congenital ichthyosis against 10.8% of apparently healthy children.1,2 The primary step of vitamin D production involves the skin; incidentally, the very organ affected in ichthyosis. Its connection to bone health might not be immediately evident, leading to undesirable consequences.
A four-year-old boy, second born from a third degree consanguineous marriage, was referred with generalised erythema and diffuse scaling since birth and bowing of legs since the last two years. The mother reported a term birth via caesarean section. At birth, a collodion membrane necessitated a ten-day neonatal intensive care admission, after which erythema and loose dry scales appeared all over his body. A history of increased redness on photo-exposure inducing an avoidance of sun and epiphora was reported. Developmental milestones were appropriate for age. There were no other mucocutaneous or systemic associations. Two years ago, the child developed pain and difficulty in walking, with subsequent bowing of lower limbs. The family had never consulted any doctors for this since infancy.
On examination, diffuse, superficial, white powdery scales and mild erythema was noted over his face with ectropion [Figure 1a]. Similar scaling without erythema was noted over the body and the extremities. Pectus carinatum [Figure 1b] and anterior bowing of bilateral lower limbs were noted. Laboratory evaluation revealed vitamin D levels <3 ng/mL, alkaline phosphatase (ALP) 1131 IU/L, parathyroid hormone (PTH) 173.9 pg/mL, and phosphate levels 3.8 mg/dL on admission. Radiological workup confirmed osteopenia, genu varum of distal femur and tibia, and severe metaphyseal changes, confirming the diagnosis of rickets [Figure 2a and 2b]. He was started on per-oral cholecalciferol 60,000 IU weekly for ten weeks and elemental calcium of 75 mg/kg/day for three months. Corrective surgery in the form of telescopic nailing with osteotomy was performed. The family was determined to continue their ayurvedic treatment and refused genetic testing, hence bland emollients were started. They were lost to follow-up post- discharge.

- Diffuse powdery scales overlying erythematous skin and bilateral ectropion.
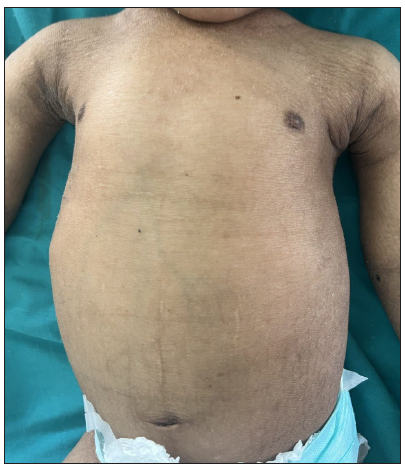
- Pectus carinatum with scaling without erythema over body and extremities.

- Preoperative X-ray image of the right leg in lateral view showing anterior bowing of femur and distal one-third of the leg, metaphyseal cupping, medullary widening and thinning of cortices.

- Preoperative X-ray image of left leg in anteroposterior view showing anterolateral bowing of distal femur, distal one-third of the leg, metaphyseal cupping, medullary widening and thinning of cortices.
Vitamin D has a very close association to skin. Figure 3a shows the production, metabolism, and functions of vitamin D.1,3,4
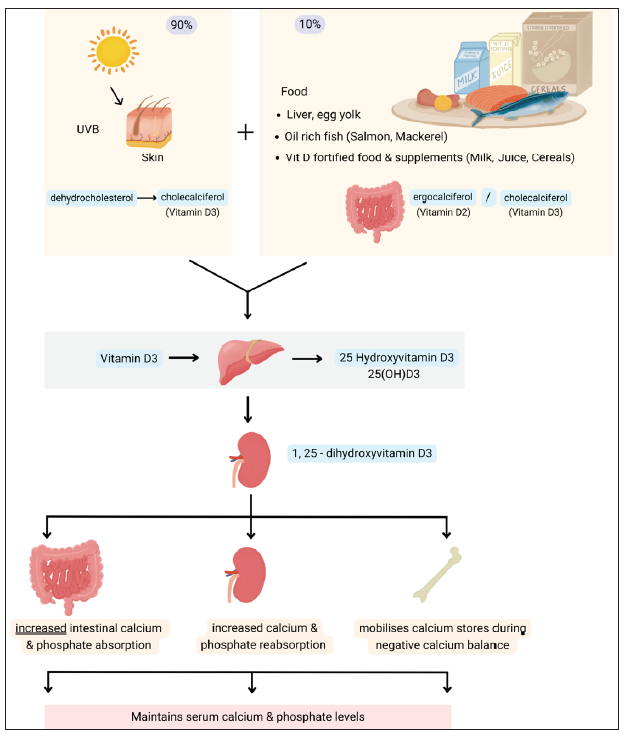
- Production, metabolism, and functions of Vitamin D.
Congenital ichthyoses are a heterogeneous group of disorders of cornification that are characterised by varying levels of scaling and/or erythema,5 and hence can affect vitamin D metabolism, making them susceptible to developing rickets and osteomalacia in children and adults, respectively.3 Vitamin D deficiency leading to hypocalcemia can present with varying amounts of extra osteal and osteal presentations. Subsequent effects on bone mineralisation are due to raised ALP and PTH levels [Figure 3b].3,6,7
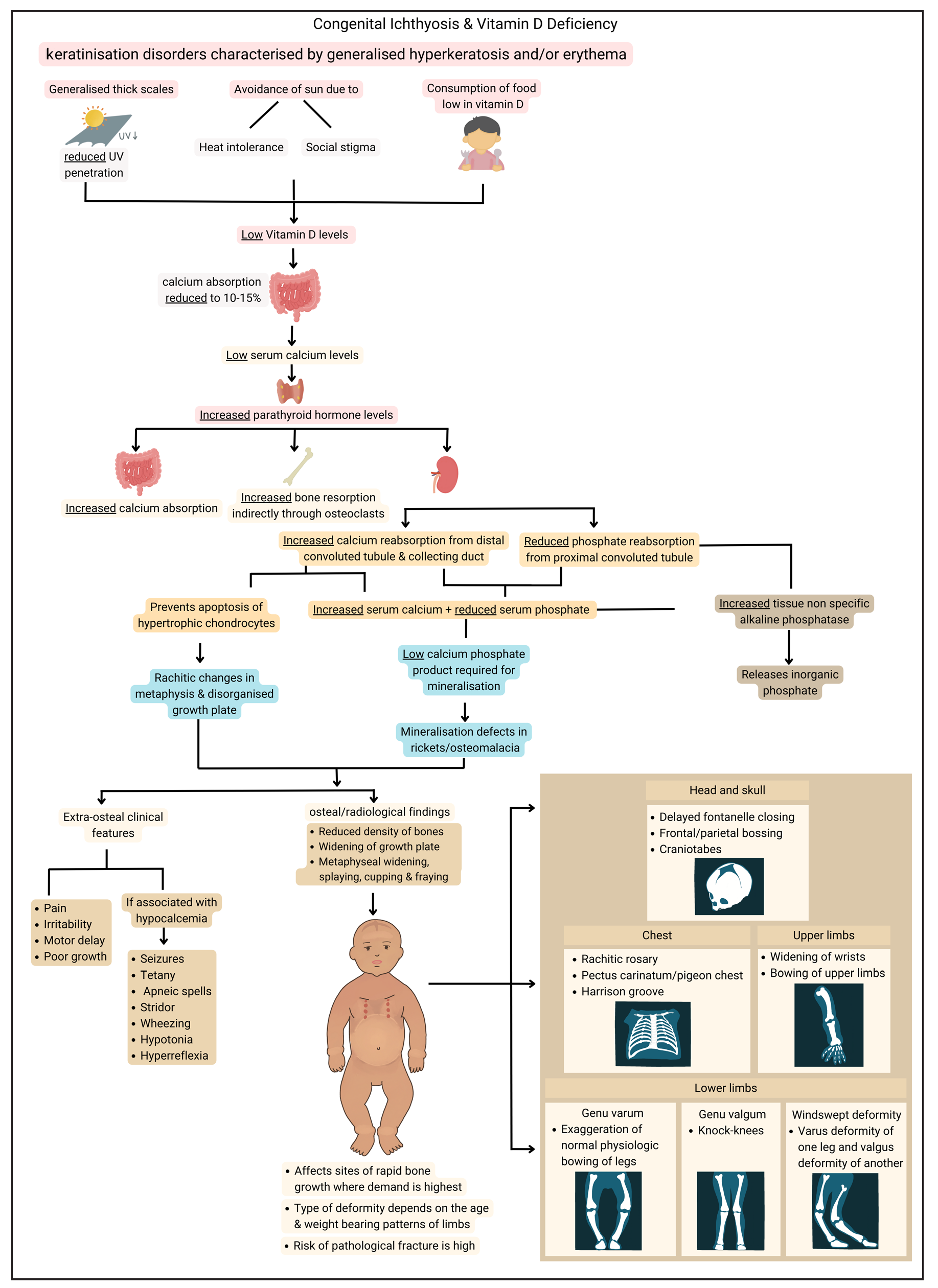
- Congenital ichthyosis and vitamin D deficiency with its rachitic outcome.
Non-syndromic and syndromic congenital Ichthyoses have been catalogued to be associated with vitamin D-deficient rickets. All the clinical, osseous, and biochemical findings of prior affected individuals have been summarised in Supplementary Table 1 from a comprehensive PubMed search of ‘congenital ichthyosis’ and ‘rickets’.1,4–6,8–23
Serum 25-hydroxyvitamin D (25[OH]D) is regarded as the most reliable indicator of a person’s vitamin D status. Many authorities classify deficiency as having a serum 25(OH)D concentration of <20 ng/mL. In a study done by Sethuraman et al., vitamin D deficiency in congenital ichthyosis was further classified as mild (10–20 ng/mL), moderate (5–10 ng/mL) and severe (<5 ng/mL). The majority of subjects tabulated in Supplementary Table 1 showed mean vitamin D levels of <5 ng/mL. A higher threshold of ‘normal’ vitamin D levels in such cases will ensure early detection and intervention, preventing flagrant deformities. Hence, maintaining a serum 25(OH)D >30 ng/mL is proposed as adequate.3 Moreover, serum 25(OH)D levels of ≤8 ng/mL and PTH ≥75 pg/mL have been shown to increase the risk of rickets in congenital ichthyosis, so a higher normal threshold for serum 25(OH)D levels of >30 ng/mL might have some credence.2
Diagnosis and management of vitamin D deficiency and calcipenic rickets thus includes various blood and osseous analysis.3 Treatment depends on low vitamin D levels with or without clinical rickets,2 and usually includes an intensive phase until signs of radiological healing are noted followed by a lifelong maintenance phase with annual evaluations [Supplementary Table 2].2,3,5,24,25
This report highlights the need to pre-emptively measure serum 25(OH)D levels in all patients of congenital ichthyosis so that an avoidable deformity and morbidity can be avoided. The triple jeopardy of congenital ichthyosis, social stigma, and rickets can further worsen the quality of life of such individuals. Vitamin D deficiency can be very easily corrected through per-oral supplementation, and procrastination in testing for this predictable deficiency can lead to detrimental effects on a child’s well-being.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Vitamin D deficiency and rickets in children and adolescents with ichthyosiform erythroderma in type IV and V skin. Br J Dermatol. 2012;166:608-15.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D, bone health and congenital ichthyosis. Indian J Dermatol Venereol Leprol. 2016;82:249-51.
- [CrossRef] [PubMed] [Google Scholar]
- Rickets-vitamin D deficiency and dependency. Indian J Endocrinol Metab. 2012;16:164-76.
- [CrossRef] [PubMed] [Google Scholar]
- Ichthyosiform erythroderma with rickets: Report of five cases. Br J Dermatol. 2008;158:603-06.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D: A new promising therapy for congenital ichthyosis. Pediatrics. 2016;137
- [CrossRef] [Google Scholar]
- Lamellar ichthyosis with genu valgum: Unfolding the link. BMJ Case Rep. 2012;2012:bcr1120115136.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Alkaline phosphatases: Biochemistry, functions, and measurement. Calcif Tissue Int. 2023;112:233-42.
- [CrossRef] [PubMed] [Google Scholar]





