Translate this page into:
Senile-onset ochronosis
2 Department of Orthopedia, Fatıh Sultan Mehmet Education and Training Hospital, Istanbul, Turkey
3 Department of Dermatology, Ankara Atatürk Education and Training Hospital, Ankara, Turkey
Correspondence Address:
Nebahat Demet Akpolat
Department of Dermatology, Beykoz State Hospital, Istanbul
Turkey
| How to cite this article: Akpolat ND, Akpola AO, Metin A. Senile-onset ochronosis. Indian J Dermatol Venereol Leprol 2016;82:744 |
Sir,
A 70-year-old woman was referred to the dermatology clinic for bluish-gray discoloration of her hands and face for 5 years. The pigmentation had gradually increased with time. She had undergone a surgery for scoliosis and gonarthrosis and had also been diagnosed with spondylitis 2 months ago for which she was taking colchicine and salazopyrin. Her other medications included valsartan, hydrochlorothiazide, propranolol and propylthiouracil for co-existing hypertension and toxic multinodular goiter. Dermatologic examination revealed a grayish- blue discoloration involving the malar areas, nasal bridge, helices of the ears, thenar regions of the hands and the lateral and medial surfaces of the thumbs and index fingers with hard papules and plaques [Figure - 1]a and [Figure - 1]b. In addition, there was brownish-black pigmentation involving both sclerae at 3'o clock and 9'o clock positions along with grayish-blue pigmentation of the nails of both hands [Figure - 1]c.
 |
| Figure 1: (a) Grayish-blue discoloration of the nasal bridge and malar region. (b) Grayish-blue macules on the lateral and medial surfaces of the thumbs and index fingers. (c) Brownish-black pigmentation on the sclera at the 3 o'clock and 9 o'clock positions. |
Results of routine laboratory investigations were within the normal range. Based on the available findings, pigmentation secondary to ochronosis was considered a probable diagnosis. No medication or other predisposing factors which could cause exogenous ochronosis could be identified from the history. The urine homogentisic acid level was detected to be 1.4 g/L (normally <0.1 g/L) and the urine turned black in color on adding sodium hydroxide. Biopsy from the left finger revealed a hyperplastic and hyperkeratotic epidermis, yellowish-brown ochronotic granules exhibiting dispersed localization in the papillary dermis and coarsening and fragmentation of the collagen bundles in patches [Figure - 2].
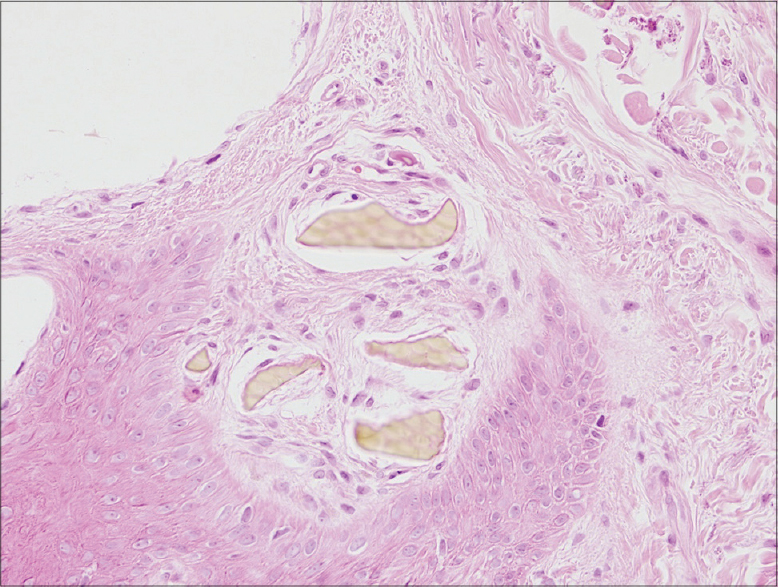 |
| Figure 2: Hyperkeratotic hyperplastic epidermis with yellow-brown ochronotic granules located in the papillary dermis (H and E, ×20) |
Based on the clinical and histopathological findings, a diagnosis of ochronosis was arrived at and the patient was asked to consult the departments of ophthalmology, cardiology and orthopedics to look for other organ involvement. Osler's sign was seen on ophthalmologic examination and cardiologic examination revealed senile degenerative changes. Musculo-skeletal system examination showed limited range of motion in the knee and hip joints. Flexion contractures of the knees were seen along with scoliosis and thoracic kyphosis. On imaging, the patient was found to have advanced degenerative changes, bridging osteophytes, calcification and reduced intervertebral disc distance and therefore, she was also diagnosed with arthropathy secondary to ochronosis [Figure - 3]. Treatment with
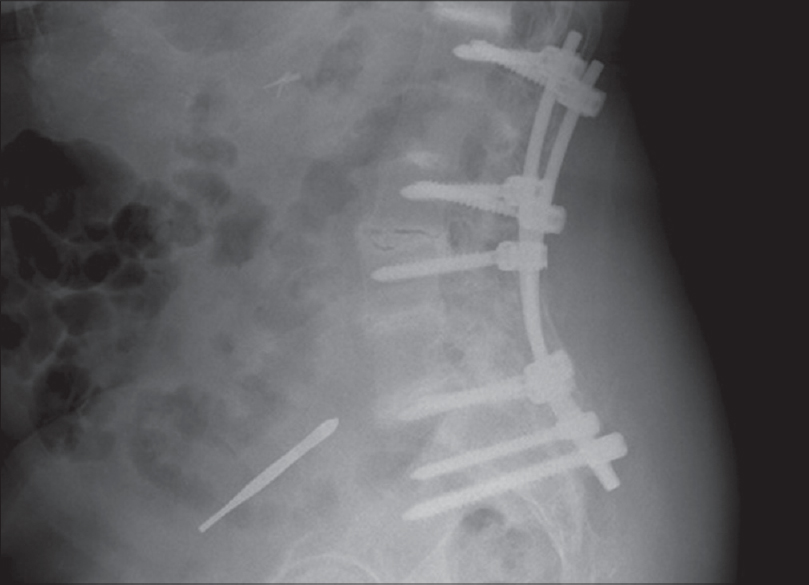 |
| Figure 3: Calcification in the intervertebral disc spaces |
1 g/day of vitamin C was initiated and the patient was on follow-up to monitor the articular and cardiologic changes.
Ochronosis is a rare hereditary disorder affecting tyrosine and phenylalanine metabolism occurring in association with homogentisic acid oxidase enzyme deficiency.[1] It may be endogenous (alkaptonuria) or exogenous (pigmentation secondary to the use of an oral anti-malarial drug or topical hydroquinone, resorcinol, picric acid, carbolic acid).[2],[3]
The major causes of morbidity in ochronosis are ochronotic arthropathy and cardiovascular involvement that occur in the fourth to fifth decades of life.[2] The deposits of homogentisic acid and its metabolites can affect both the axial and peripheral joints.[2],[4] Particularly during the fifth to sixth decades, stenosis and calcification of the aorta and mitral valves may occur secondary to the accumulation of ochronotic pigment.[2],[4]
Ochronotic pigment changes, which are the main clinical signs of the disease, occur particularly on sun-exposed areas such as the face and the dorsae of hands, cartilaginous regions such as the helices of the ears, areas that are rich in sweat glands such as the armpits and groin, and the nails. These changes are usually evident during the fourth decade of life.[2]
On skin biopsy, ochronotic pigment which is stained yellowish-brown with hematoxylin and eosin may be observed lying free in the tissue or in the form of granules in the vessel wall endothelium, basal membrane, eccrine sweat glands or inside the macrophages. Quantitative homogentisic acid levels may be estimated in the urine and blood by the gas-liquid chromatography method.[4]
The changes induced by alkaptonuria progress slowly but are irreversible and there is no effective treatment.[2],[4] High-dose vitamin C which affects homogenitisic acid metabolism and polymerizationin vitro and N-acetyl cysteine and vitamin E, which is also known to affect homogenitisic acid polymerization and accumulation, may be used for treatment.[2] In addition, a low-protein diet that is poor in tyrosine and phenylalanine may be beneficial, particularly in young patients.[2]
In conclusion, alkaptonuria is a rare disease with an autosomal recessive inheritance pattern. Skin lesions being the major clinical signs and showing the characteristic histopathologic changes are of importance in establishing an early diagnosis. Early diagnosis as well as detailed patient counseling and follow-up are important with respect to cardiovascular involvement and ochronotic arthropathy which occur particularly during the fourth and sixth decades and cause increased morbidity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Atalay A, Gocen U, Basturk Y, Kozanoğlu E, Yaliniz H. Ochronotic involment of the aortic and mitral valves in a 72-year-old man. Tex Heart Inst J 2015;42:84-6.
[Google Scholar]
|
| 2. |
Unlu I, Nacır B, Ulaslı AM, Erdem HR. Ochronotic spondylosis and arthropathy: Case report. Firat Med J 2008;13:220-3.
[Google Scholar]
|
| 3. |
Lapeere H, Boone B, De Schepper S, Verhaeghe E, Ongenae K, Geel NV, Hypomelanoses and hypermelanoses. Fitzpatrick' Dermatology in General Medicine. 7th ed. New York: The Mcgraw-Hill Companies; 2008. pp. 622-40.
[Google Scholar]
|
| 4. |
Yancovitz M, Anolik R, Pomeranz MK. Alkaptonuria. Dermatol Online J 2010;16:6.
[Google Scholar]
|
Fulltext Views
2,414
PDF downloads
2,613





