Translate this page into:
Sepsis secondary to Rapunzel syndrome
Corresponding author: Dr. Ngo Binh Trinh, Nguyen Thong, District 3, Ho Chi Minh City, Vietnam. mdbinhtrinh@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Trinh NB, Nguyen MT, Hanh Nguyen TG. Sepsis secondary to Rapunzel syndrome. Indian J Dermatol Venereol Leprol doi: 10.25259/IJDVL_214_2022
Sir,
Rapunzel syndrome is an uncommon cause of trichobezoar, characterized by trichotillomania and trichophagia, subsequently resulting in gastrointestinal trichobezoar.1 Herein, we report a case of Rapunzel syndrome in a 4-year-old girl with concomitant intussusception and septic shock.
A 4-year-old girl was referred from a remote hospital to our center with history of sharp, crampy abdominal pain of 2-day duration associated with vomiting and non-bloody diarrhea. She was born at term following an uneventful pregnancy. Her parents denied any history of neuropsychomotor developmental delay. The patient was unconscious at presentation with manual ventilation (SpO2 = 98%), fever, tachycardia, abdominal tenderness and voluntary guarding. Dermatological examination revealed patchy hair loss on the scalp [Figure 1a]. We clinically diagnosed septic shock induced by intussusception. She was urgently admitted to the intensive care unit (ICU) and started on mechanical ventilation, intravenous fluids and intravenous empirical antibiotics. Hematological evaluation revealed total leukocyte count of 17,370/mm (polymorphs 78.3%, lymphocytes 12.6%, monocytes 9.0% and basophils 0.1%), aspartate aminotransferase (63 u/l), alanine aminotransferase (85 u/l), c-reactive protein (22 mg/l) and procalcitonin (2 ng/mL). Other tests including coagulation tests, serum lactate level, arterial blood gas analysis and peripheral blood culture were unremarkable. The abdominal radiograph revealed distended bowel loops with absence of colonic gas [Figure 1c], while ultrasonography showed a target sign corroborating the diagnosis of intussusception due to trichobezoar The hairy mass was removed by rectal catheter [Figure 1b] and patient was discharged after 15-days.
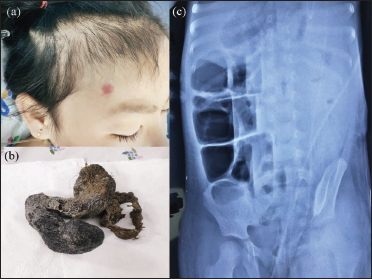
- (a) Patchy hair loss on the scalp. (b) The hairy mass was removed. (c) Distended loops of bowel with the absence of colonic gas on the abdominal plain film
She was referred for psychologist consultation, where a diagnosis of separation anxiety disorder was made, possibly aggravated by loneliness during the 4-month quarantine during COVID-19 pandemic. quarantine of the. A behavioural intervention was suggested to improve her the symptoms prior to medications.
Rapunzel syndrome is an unusual type of trichobezoar, first described by Vaughan et al. in 1968.2 The trichobezoars were formed by hair accumulation within the stomach and intestine, subsequent to trichotillomania and trichophagia disorder spectrum.3
The criteria to identify Rapunzel syndrome includes a trichobezoar with tail, which extends at least to the jejunum causing intestinal obstruction.1 The diagnosis of trichobezoars is quite challenging due to non-specific abdominal symptoms such as anorexia, weight loss, vomiting, abdominal pain and gastrointestinal bleeding.3,4 Plain film and ultrasound can detect 20–60% of bezoar cases, while abdominal computerised tomography scans are effective in 97% of cases. However, upper gastrointestinal endoscopy remains the gold standard for diagnosing trichobezoars.1
The complications related to gastrointestinal bezoars include ulceration, perforation, peritonitis, pancreatitis, obstructive jaundice, pneumatosis intestinalis and intussusception.1 Our patient presented with intussusception, which was confirmed by imaging.
Management of trichobezoars includes upper endoscopy, laparotomy, open surgical operation and psychiatric treatments.1,4 Diagnosing and managing trichotillomania is an integral part of its treatment. A multidisciplinary team including a dermatologist, pediatrician and/or psychiatrist along with patient education is necessary to prevent the aforementioned complications at the earliest stage.
The primary treatment includes psychologic therapy techniques such as cognitive behavioural therapy and habit reversal training, along with additional medications, when needed. Habit reversal therapy involves three factors: awareness, competing for the response and social support. Oral medications such as selective serotonin reuptake inhibitors, olanzapine, aripiprazole, quetiapine, clomipramine and n-acetylcysteine have shown positive results on treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflict of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Rapunzel syndrome: A rare case of small bowel intussusception in a child. Cureus. 2021;13:e17911.
- [CrossRef] [PubMed] [Google Scholar]
- The Rapunzel syndrome: An unusual trichobezoar presentation. Case Rep Med. 2010;2010:841028.
- [CrossRef] [PubMed] [Google Scholar]
- Giant gastroduodenal trichobezoar: A case report. World J Clin Cases. 2019;7:3649-54.
- [CrossRef] [PubMed] [Google Scholar]
- Gastric perforation secondary to Rapunzel syndrome. BMJ Case Rep. 2021;14:e240100.
- [CrossRef] [PubMed] [Google Scholar]





