Translate this page into:
Solitary nodular lesion on forehead in a 56-year-old woman
Correspondence Address:
Mukta Pujani
Department of Pathology, ESIC Medical College, Faridabad, Haryana
India
| How to cite this article: Agarwal C, Singh K, Pujani M, Verma P, Chauhan V. Solitary nodular lesion on forehead in a 56-year-old woman. Indian J Dermatol Venereol Leprol 2019;85:555-558 |
A 56-year-old woman came to the surgical out-patient department of ESIC Medical College and Hospital, Faridabad, Haryana, with a swelling above the left eyebrow which she noticed since 5 years. There was no history of trauma. There was no significant past history or other relevant complaints. Systemic examination was within normal limits. On local examination, a well-circumscribed reddish nodular lesion of size 2 × 2 cm was seen just above the left eyebrow [Figure - 1]. It was non-tender and soft to firm in consistency.
 |
| Figure 1: Clinical presentation of the patient with a well-circumscribed nodular reddish lesion above left eyebrow |
Fine-needle aspiration was done; smears were moderately cellular, comprising of tight clusters of small basaloid cells with scant cytoplasm, round to oval bland nuclei and inconspicuous nucleoli. Basement membrane material was seen lying in between the tumor cells with cells embedded in it. A few histiocytes along with multinucleated giant cells were seen in the background.
An excision biopsy was advised. A grey-white soft tissue mass measuring 2 × 1 cm was excised, from which multiple sections were taken. There was a well-circumscribed lesion in the dermis comprising lobules of basaloid tumor cells, separated by fibrous septa [Figure - 2]. On further sections, a few of the lobules showed presence of retraction artifacts [Figure - 3], mitotic figures (3-4/10 high power field) [Figure - 4] and a few horn cysts. No amyloid or melanin was seen in the sections examined. An immunohistochemistry panel comprising of CD10 [Figure - 5], CD34, bcl-2 [Figure - 6], epithelial membrane antigen and cytokeratin 20 was advised.
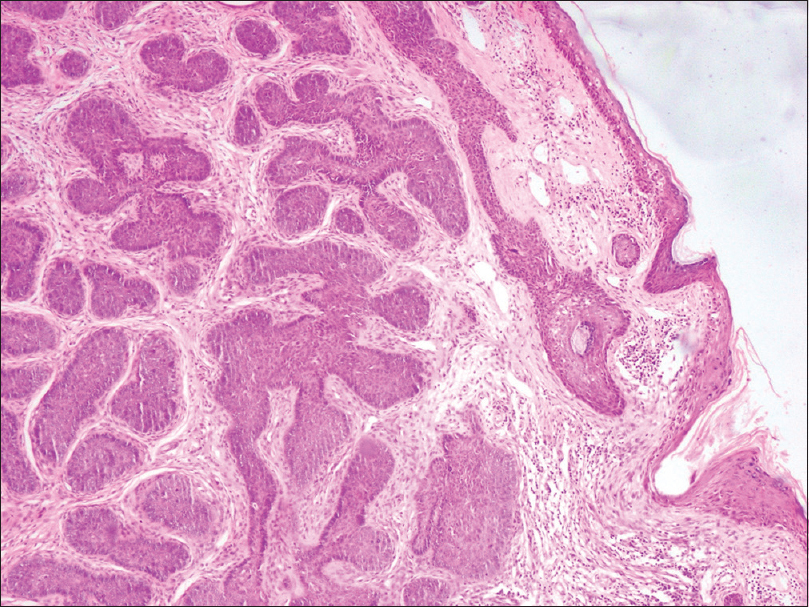 |
| Figure 2: Histopathology smear showing skin covered tissue. Sub-epidermis shows a well-circumscribed lesion comprising lobules of basaloid tumor cells, separated by fibrous septa (hematoxylin and eosin, ×100) |
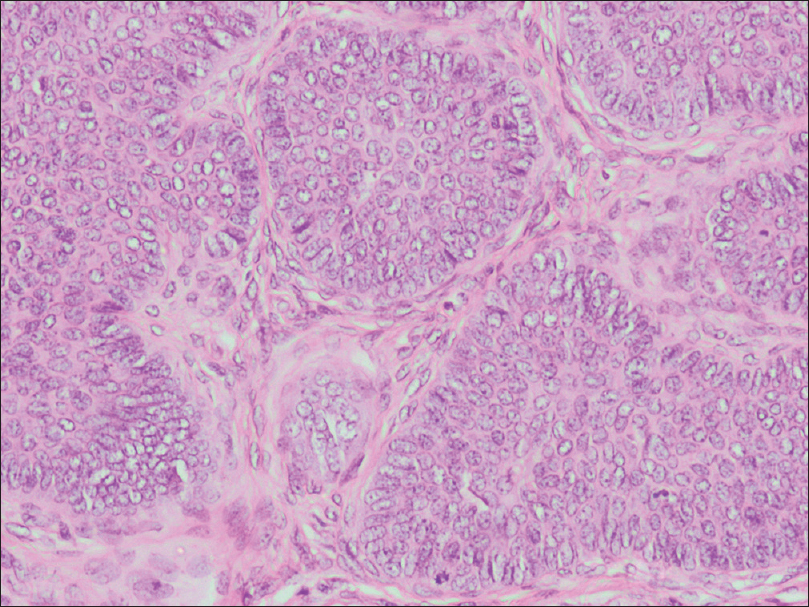 |
| Figure 3: Histopathology smear with some of the lobules showing presence of retraction artifact (hematoxylin and eosin, ×400) |
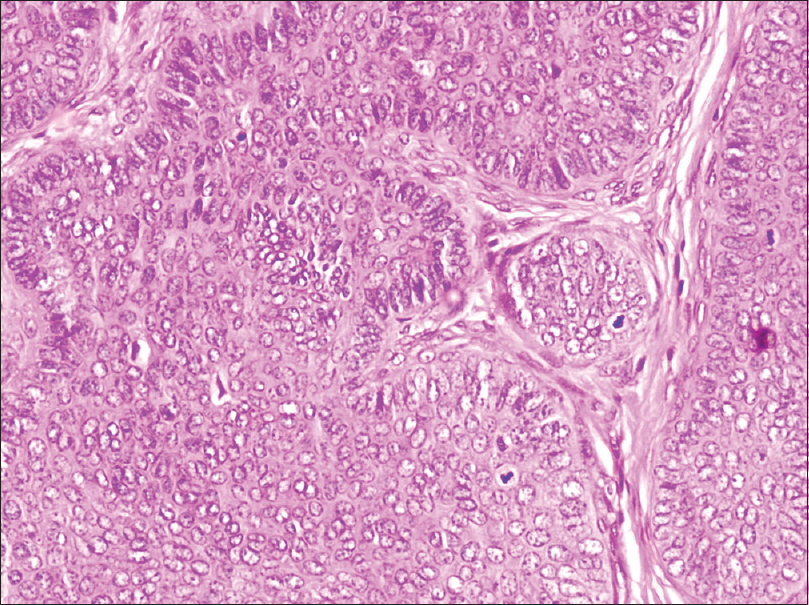 |
| Figure 4: Histopathology smears with presence of mitotic figures (hematoxylin and eosin, ×400) |
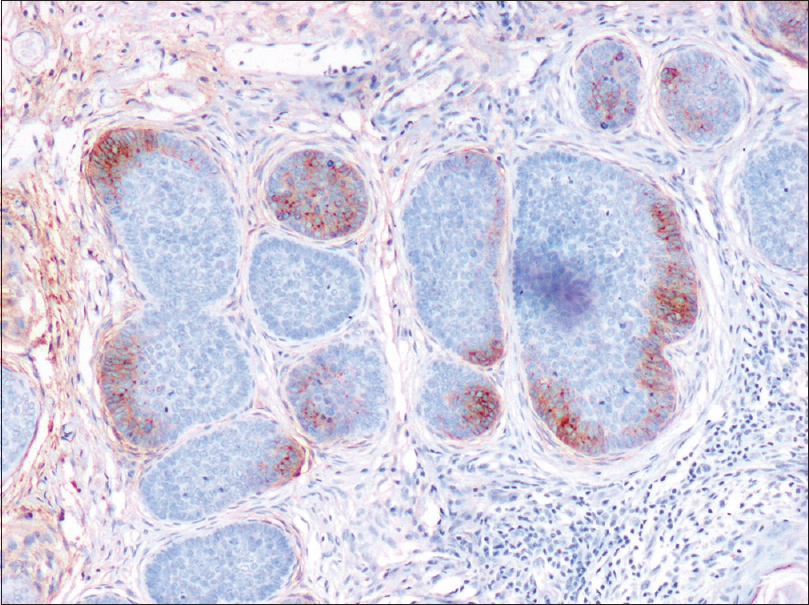 |
| Figure 5: Immunohistochemistry: CD10 showed focal cytoplasmic membranous positivity in tumor cells and stromal negativity (×400) |
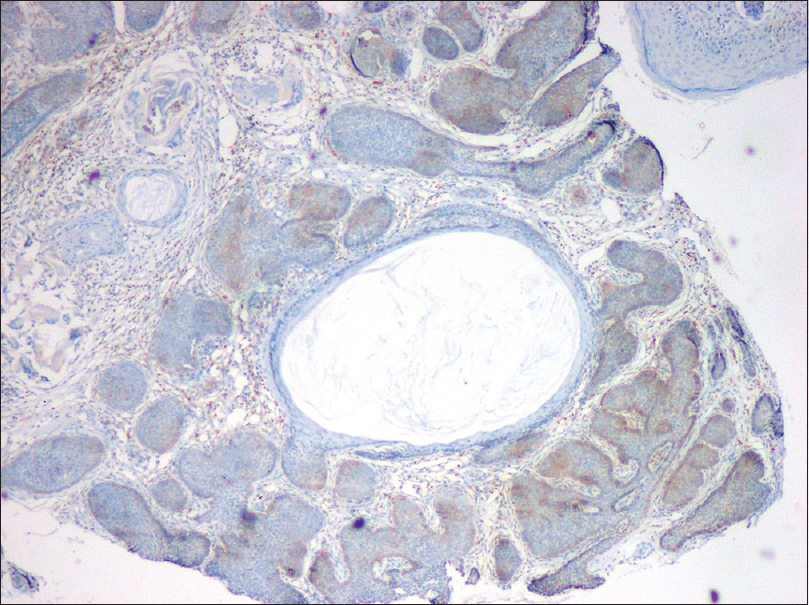 |
| Figure 6: Immunohistochemistry: Bcl-2 showed diffuse cytoplasmic positivity in tumor cells (×100) |
What is Your Diagnosis?
Answer
Basal cell carcinoma.
On immunohistochemistry, CD10 showed focal cytoplasmic membranous positivity in tumor cells and stromal negativity. Bcl-2 was diffusely positive in the cytoplasm of tumor cells, although weak; while CD34, epithelial membrane antigen and cytokeratin 20 came out to be negative. So a final diagnosis of basal cell carcinoma was arrived at. The margins of the lesion were free of the tumor. On follow-up, it was found that the patient was doing well.
It is very difficult to differentiate between trichoepithelioma and basal cell carcinoma, which poses a great difficulty for both the clinicians as well as the pathologists.[1] Trichoepithelioma is a benign neoplasm derived from basal cells in the hair follicle. It may occur sporadically or is inherited in an autosomal dominant pattern. The principal feature of a common genetic disorder called multiple familial trichoepithelioma is the presence of many small tumors, predominantly on face.[2] Both basal cell carcinoma and trichoepithelioma can present as solitary, slow-growing, flesh-colored papules or nodules with a pearly appearance, commonly located on the face.[1] Similarly in the present case, the patient presented with a flesh-colored nodule on the face.
Microscopically, both basal cell carcinoma and trichoepithelioma are composed of nests of basaloid cells within the dermis. Histopathological features of basal cell carcinoma include connection to the epidermis, apoptosis, mitosis and loose fibromyxoid stroma with peritumoral retraction.[1] Horn cysts are the most characteristic histologic feature of trichoepithelioma. Tumor cells in trichoepithelioma have similar appearance to the cells in basal cell carcinoma but lack high-grade atypia and mitosis. In trichoepithelioma, the fibroblasts encircle the basaloid islands and are tightly associated with them, lacking the retraction artifact, typical of basal cell carcinoma. A connection between tumor cell formations and the surface epidermis has been shown to exist in approximately 90% of basal cell carcinomas.[3] In the present case, a focal connection with epidermis, retraction artifact, mitosis and few horn cysts was found after extensive search, thereby creating a dilemma.
There is a variant of basal cell carcinoma that histologically resembles a benign follicular neoplasm and is designated as trichoepithelioma-like basal cell carcinoma. These are often small, circumscribed, symmetrical basaloid tumors. These tumors often have a relatively low number of mitotic figures and the stroma often lacks significant retraction artifact.[4] Another rare subtype of basal cell carcinoma is infundibulocystic basal cell carcinoma. Histopathologically, it is also a well-circumscribed, superficially located, basaloid cell tumor with hyperchromatic, pleomorphic nuclei and rare mitoses. However, it is formed by anastomosing cords of basaloid keratinocytes with several tiny cornifying cysts.[5] We observed some of the overlapping features of the above-mentioned rare variants of basal cell carcinoma in our case.
Basal cell carcinomas are seen almost exclusively on hair-bearing skin, especially on face. It usually occurs as a single lesion. It has five clinical types: (a) superficial, (b) nodular, (c) micronodular, (d) infiltrating and (e) fibroepithelioma. Nodular basal cell carcinoma begins as a small, waxy nodule that often shows a few small telangiectatic vessels on its surface.[3]
There are few immunohistochemical markers which are able to differentiate between trichoepithelioma and basal cell carcinoma. CD10 expression has been shown in tumors of follicular differentiation, including trichoepithelioma, pilomatricoma, basaloid follicular hamartoma and basal cell carcinoma. There is a difference in staining patterns of CD10 in these tumors: basaloid cells in basal cell carcinoma and stroma in trichoepithelioma.[2] The present case shows focal membranous staining in the basaloid cells, suggesting basal cell carcinoma.
Diffuse bcl-2 expression by basaliomatous cells was observed in basal cell carcinoma, while expression of this marker only in the outermost layers of basaloid nests was observed in trichoepitheliomatous tumors.[6] In our case also, although bcl-2 expression was diffuse it was only weakly positive.
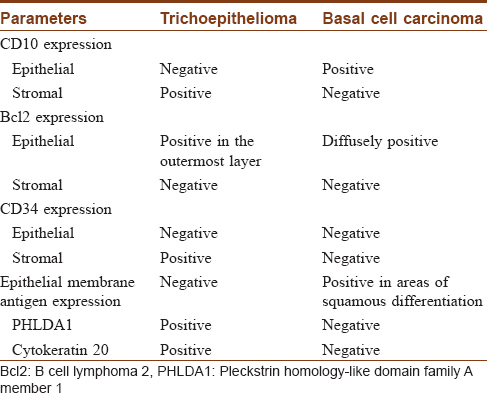
Follicular stem cell marker, pleckstrin homology-like domain, family A, member 1 (also known as T-cell death-associated gene 51), and cytokeratin 20 are positive in trichoepithelioma and negative in basal cell carcinoma. [Table - 1] depicts immunohistochemical markers that help to differentiate between trichoepithelioma and basal cell carcinoma.[7] However, in spite of availability of immune marker panel, histopathological criteria along with clinical data remain the best tool to differentiate between trichoepithelioma and basal cell carcinoma.[6]
In the present case, a diagnosis of basal cell carcinoma was favored over trichoepithelioma due to some supporting histomorphological features like focal connection with the epidermis, retraction artifact and mitosis along with focal membranous staining of CD10 in the basaloid cells and weak diffuse positivity of bcl-2 on immunohistochemistry.
Both the tumors share similar clinical as well as histological features. It is very important to distinguish these neoplasms because they have variable clinical behavior and require different therapeutic planning. Basal cell carcinoma is a locally aggressive neoplasm and must be totally excised with safe margins. However, trichoepithelioma is a benign neoplasm, which may be partially excised by shaving.[6]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for the images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Pham TT, Selim MA, Burchette JL Jr., Madden J, Turner J, Herman C, et al. CD10 expression in trichoepithelioma and basal cell carcinoma. J Cutan Pathol 2006;33:123-8.
[Google Scholar]
|
| 2. |
Heidarpour M, Rajabi P, Sajadi F. CD10 expression helps to differentiate basal cell carcinoma from trichoepithelioma. J Res Med Sci 2011;16:938-44.
[Google Scholar]
|
| 3. |
Klein W, Chan E, Seykora JT. Tumours of epidermal appendages. In: Elder DE, editor. Lever's Histopathology of the Skin. 10th ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 867-926.
[Google Scholar]
|
| 4. |
Carr RA, Taibjee SM, Sanders DS. Basaloid skin tumours: Basal cell carcinoma. Diagn Histopathol 2007;13:252-72.
[Google Scholar]
|
| 5. |
Roldán-Marín R, Leal-Osuna S, Lammoglia-Ordiales L, Toussaint-Caire S. Infundibulocystic basal cell carcinoma: Dermoscopic findings and histologic correlation. Dermatol Pract Concept 2014;4:51-4.
[Google Scholar]
|
| 6. |
Tebcherani AJ, de Andrade HF Jr. Sotto MN. Diagnostic utility of immunohistochemistry in distinguishing trichoepithelioma and basal cell carcinoma: Evaluation using tissue microarray samples. Mod Pathol 2012;25:1345-53.
[Google Scholar]
|
| 7. |
Agarwal P, Agarwal C, Bhardwaj M, Ahuja A, Rani S. Trichoepithelioma and basal cell carcinoma with squamous differentiation: Is it causal or coincidental? Indian J Dermatol 2015;60:394-6.
[Google Scholar]
|
Fulltext Views
5,005
PDF downloads
1,879





