Translate this page into:
Successful combined treatment of Buschke–Lowenstein tumor in anal canal with electroresection, photodynamic therapy and topical 5% imiquimod
Corresponding author: Dr. Chunguang Ma, Department of Dermatology, The First Affiliated Hospital, Sun Yat-Sen University, No. 58 Zhongshan Er Rd., Guangzhou 510080, China. machung@mail.sysu.edu.cn
-
Received: ,
Accepted: ,
How to cite this article: Huang X, Liu M, Han J, Ma C. Successful combined treatment of Buschke–Lowenstein tumor in anal canal with electroresection, photodynamic therapy and topical 5% imiquimod. Indian J Dermatol Venereol Leprol 2021;87:121-4.
Sir,
Buschke–Lowenstein tumor was first described as an invasive and exophytic lesion on the penis in 1925.1 During the past decades, Buschke-Lowenstein tumor on perineum, anus, and rectum have been reported. However, Buschke–Lowenstein tumor in anal canal has rarely been described. Herein we report a case of Buschke-Lowenstein tumor in anal canal treated with combination of electroresection, laser-mediated photodynamic therapy, and topical 5% imiquimod cream. The lesions had resolved within 4 months of treatment. During the next 8-year follow-up, the patient remained symptom-free without any other complications.
A 24-year-old female visited our out-patient clinic 8 years ago, with a complaint of newly emerging giant warts located in anal canal and recurrent perianal lesions for 6 months. She had a history of anal sex with a male who had multiple sex partners. She had undergone 4 sessions of laser resection previously for her recurrent anogenital warts. Anal speculum examination revealed a bulky cauliflower-like condylomatous mass blocking the anal canal. Complete blood counts, liver and renal function tests were normal. Cellular immunity, assessed by the percentages of CD4+ and CD8+ T cells, CD19+ B cells and natural killer cells in blood, was normal.
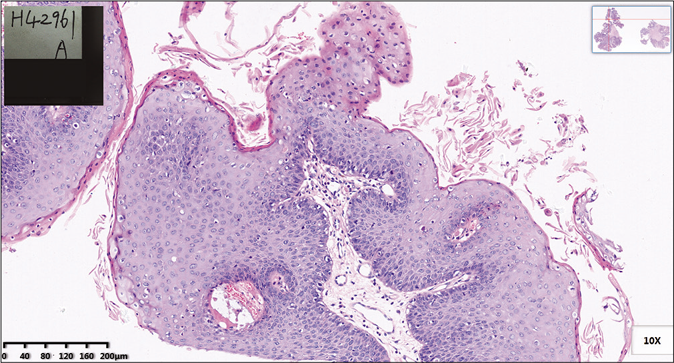
Based on the history and clinical features, patient was diagnosed to have Buschke-Lowenstein tumor in anal canal . We resected the giant cauliflower-like lesion by electroresection under epidural anesthesia. The lesion was about 5 cm in diameter and was resected with a 5 mm healthy margin. [Figure 1].

- Bulky condylomatous lesion about 5 cm in diameter
Histopathological examination of the mass in the anal canal showed papillary proliferation with extensive acanthosis, parakeratosis, and vacuolization [Figure 2a]. With the positive immunohistochemical staining by in situ hybridization of human papillomavirus antigen (HPV-Ag), the giant lesion was confirmed to be infected by HPV [Figure 2b]. The lesion had no apparent features of malignant tumor or transformation.
- Papillary proliferation with obvious vacuolization (H and E, ×100)
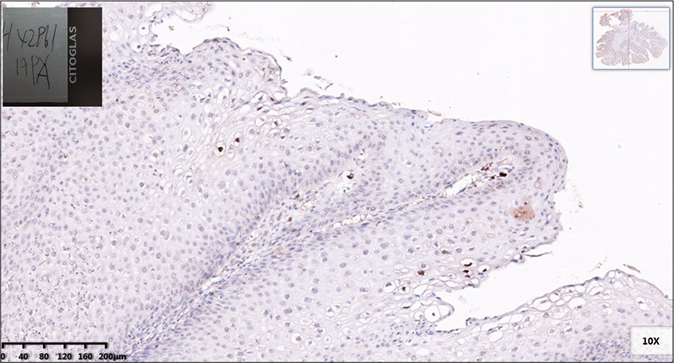
- Human papilloma virus antigen staining showing positive expression in koilocytes (H and E×100)
The wound healed 3 weeks postoperatively. However, during the following weekly visits, 4 times of recurrences were recorded on week 4.5, 5.5, 8.5, and 12.6 in the anal canal. We performed electroresection followed by laser-mediated photodynamic therapy once the recurrent lesion was identified. The process involved application of topical 16% 5-aminolevulinic acid gel and suppository in the anal canal by a sterile cotton piece left for 3 hours. Subsequently, the lesion was irradiated for 20 min via an anal speculum using a 635nm laser beam at 120 J/cm2 intensity (FD-400-B, linyun photoelectronic system co. Ltd, China).
From week 6.5, the patient received topical 5% imiquimod cream application into the anal canal every week for 9 weeks. On week 16, we confirmed that her previous lesions have resolved based on physical examination and a negative acetowhite test [Figure 3]. There were no recurrent lesions during the subsequent 8-year follow-up. The patient only reported intense burning sensation during laser application, and no other complications were observed. The course of the treatment is presented in Table 1.
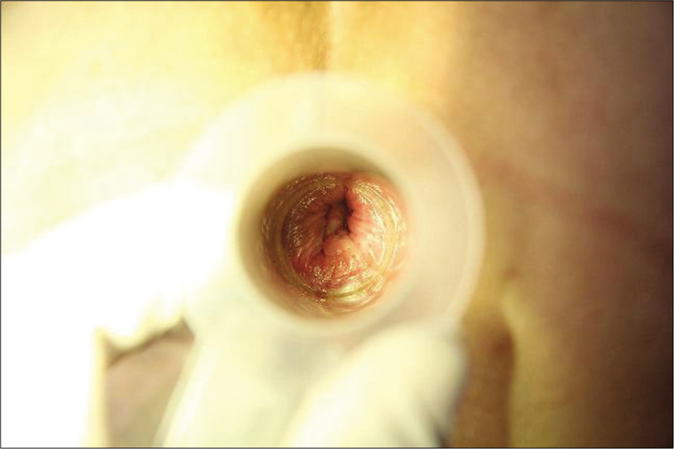
- No recurrent lesion in anal canal
| Time | Course of the disease | Physical examinations | Diagnosis | Treatment | |
|---|---|---|---|---|---|
| Perianal area | Anal canal | ||||
| 20110905 | 6 months ago | Papules and plaques | Unclear | Perianal CA | Four times laser resection |
| 20120307 | Day 1 | Papules and plaques | Giant tumor | Perianal CA and BLTAC | Electroresection of perianal lesions + PDT |
| 20120314 | Day 7 | Faded perianal lesions | Giant tumor | Perianal CA and BLTAC | Electroresection of perianal lesions + PDT |
| 20120320 | Day 14 | Perianal lesions | Giant tumor | BLTAC | Electroresection under epidural anesthesia |
| 20120411 | Week 4.5 | None | Two lesions about 8 and 10 mm in diameter under dentate line | Recurrence in anal canal | Electroresection + PDT |
| 20120418 | Week 5.5 | None | One papule about 3 mm in diameter on dentate line | Recurrence in anal canal | Electroresection + PDT |
| 20120425 | Week 6.5 | None | None | No recurrence | Topical 5% imiquimod cream |
| 20120503 | Week 7.5 | None | None | No recurrence | Topical 5% imiquimod cream |
| 20120511 | Week 8.5 | None | BLTAC | Recurrence in anal canal | Electroresection+PDT |
| 20120518 | Week 9.5 | None | None | No recurrence | Topical 5% imiquimod cream |
| 20120524 | Week 10.5 | None | None | No recurrence | Topical 5% imiquimod cream |
| 20120601 | Week 11.5 | None | None | No recurrence | Topical 5% imiquimod cream |
| 20120609 | Week 12.6 | None | One papule about 3 mm in diameter on dentate line | Recurrence in anal canal | Electroresection + PDT |
| 20120613 | Week 13.5 | None | None | No recurrence | Topical 5% imiquimod cream |
| 20120622 | Week 14 | None | None | No recurrence | Topical 5% imiquimod cream |
| 20120629 | Week 15 | None | None | No recurrence | Topical 5% imiquimod cream |
| 20120707 | Week 16 | None | None | No recurrence | Topical 5% imiquimod cream |
CA: Condyloma acuminatum, BLTAC: Buschke-Lowenstein tumor in anal canal, PDT: Photodynamic therapy
Buschke-Lowenstein tumor in anal canal is a rare disease, with a high recurrence rate.2 The surgical treatment represents the first-line therapy.3 However, complications such as anal reconstruction or stenosis are quite common postoperatively. There is limited literature on anal condyloma acuminatum cases being treated with photodynamic therapy 4 Recurrences in our case was probably caused by incomplete resection of the condyloma lesion inside the anal canal. Laser-mediated photodynamic therapy with 5-aminolevulinic acid is an emerging approach for treating genital HPV infection.5 Several studies have suggested the administration of topical aminolevulinic acid along with photodynamic therapy is an effective, safe, and well-tolerated treatment for condyloma acuminatum, and more importantly, associated with low recurrence rate.6 In our case, laser-mediated photodynamic therapy was beneficial in ablating the residual tiny and latent lesions. With our previous experiences in treating and preventing the recurrence of cervical condyloma accuminatum, we prescribed topical 5% imiquimod cream on both perianal skin and anal canal for the patient weekly for latent lesions.7 Since week 16, no recurrences have been observed involving both external and internal anal region.
In summary, we recommend electroresection to resect the entire visible lesion and preserve anal function. Subsequently, the combined application of laser-mediated photodynamic therapy and topical 5% imiquimod cream can remarkably reduce the recurrence rate for Buschke-Lowenstein tumor in anal canal . Moreover, the long-lasting efficacy of combined treatment reduces the physical inconvenience for the patients and saves the cost of treatment. We consider this effective and acceptable therapy was worthy of clinical application.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was supported by the Guangdong Natural Sciences Foundation of China (grant no. 2018A030310270) and the Guangzhou Science and Technology Planning Project of China (grant no. 201807010081).
Conflicts of interest
There are no conflicts of interest.
References
- Giant condylomata acuminata (carcinoma-like condylomata or Buschke-Loewenstein tumors) of the penis. J Urol. 1953;69:164-72.
- [CrossRef] [Google Scholar]
- Giant condyloma acuminatum (Buschke-Lowenstein tumor) of the anorectal and perianal regions.Analysis of 42 cases. Dis Colon Rectum. 1994;37:950-7.
- [CrossRef] [PubMed] [Google Scholar]
- Giant condyloma acuminatum-Buschke-Lowenstein disease-A literature review. Chirurgia (Bucur). 2014;109:445-50.
- [Google Scholar]
- Photodynamic therapy for the treatment of endoanal condylomata acuminata. Clin Infect Dis. 2010;51:1222-3.
- [CrossRef] [PubMed] [Google Scholar]
- Topical hexaminolevulinate photodynamic therapy for the treatment of persistent human papilloma virus infections and cervical intraepithelial neoplasia. Expert Opin Investig Drugs. 2015;24:273-81.
- [CrossRef] [PubMed] [Google Scholar]
- Therapeutic combination of radiofrequency surgical dissection and oral acitretin in the management of perianal Buschke-Lowenstein tumour: a case report. Int J STD AIDS. 2012;23:362-4.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of recurrent and refractory cervical condylomata acuminata with topical 5% imiquimod cream in five patients. Int J STD AIDS. 2010;21:528-9.
- [CrossRef] [PubMed] [Google Scholar]





