Translate this page into:
Successful treatment of metastatic extramammary Paget's disease with pemetrexed monotherapy systemically and 5-fluorouracil topically
2 Department of Chemotherapy, Zhongshan People's Hospital, Zhongshan, Guangdong Province, People's Republic of China
3 Department of Oncology, Southern Medical University, Guangzhou, People's Republic of China
Correspondence Address:
Hanlin Liang
Department of Chemotherapy, Zhongshan People's Hospital, Zhongshan, Guangdong Province
People's Republic of China
| How to cite this article: Chen K, Liang H, Peng J, Zheng Y. Successful treatment of metastatic extramammary Paget's disease with pemetrexed monotherapy systemically and 5-fluorouracil topically. Indian J Dermatol Venereol Leprol 2019;85:56-59 |
Abstract
Advanced extramammary Paget's disease does not have a standardized treatment guideline as its incidence is low and has been rarely reported in literature. Here we describe a case of metastatic extramammary Paget's disease successfully treated with topical 5-fluorouracil (5-FU) and systemic pemetrexed. The therapy was safe without any appreciable adverse effects like diarrhea, rash, neutropenia or fatigue; maintaining remission for more than 6 months. Thus, we propose 5-FU and pemetrexed as the first-line therapy for advanced extramammary Paget's disease, especially for aged patients with unresectable skin lesions.
Introduction
Extramammary Paget's disease is a rare, slowly progressing malignancy, which may be cured with adequate treatment in the initial stages. However, in its advanced stages, treatment is mainly aimed at improving the quality of the patients' life and prolonging their survival. The treatment strategy for managing this condition should be highly effective, tolerable and less toxic. Here, we describe such a case involving the scrotum with distant metastases which responded favorably to 5-fluorouracil (5-FU) and pemetrexed therapy.
Case Report
A 76-year-old man was admitted in our hospital with complaints of recurrent itchy, erosive and oozing scrotal skin for the last 4 years. Initially, he developed an itchy, red lesion around the scrotum, which disappeared on using sulfur soap and emollient cream. Within three months, the scrotal skin became swollen, eroded and oozy. Subsequently he developed mild, asymptomatic edema involving both lower extremities. He had been admitted to our hospital for further evaluation and management.
Physical examination revealed multiple, enlarged lymph nodes in his right groin which were discreet, hard, elastic and mobile without any tenderness. An oozing, erythematous area, approximately 8 cm in diameter, was seen on the upper right region of the swollen scrotum [Figure - 1]a.
 |
| Figure 1 |
Abdominal computed tomography (CT) images revealed large (4-7 mm) nodules in the liver. In addition, multiple enlarged lymph nodes were detected around the abdominal aorta and bilateral inguinal regions; their diameters ranging from 15 – 35 mm. All these findings were considered to be signs of metastasis [Figure - 2]. Metastatic infiltration was also observed to involve the head of the pancreas, the bile duct, surrounding lymph nodes and bilateral crura of the diaphragm. Pelvic imaging also corroborated the CT findings. The patient underwent a punch biopsy and histolopathological examination. Microscopic examination of the biopsy sample showed presence of Paget cells in the dermis [Figure - 3]. Further immunohistological analysis revealed that the specimen was cytokeratin+, cytokeratin5/6+, cytokeratin7+, P63 (partly +), cytokeratin (high molecular weight)+, carcino-embryonic antigen+, S-100 (partly +), human epidermal growth factor receptor-2+, HMB45−, which was consistent with the diagnosis of Paget's disease.
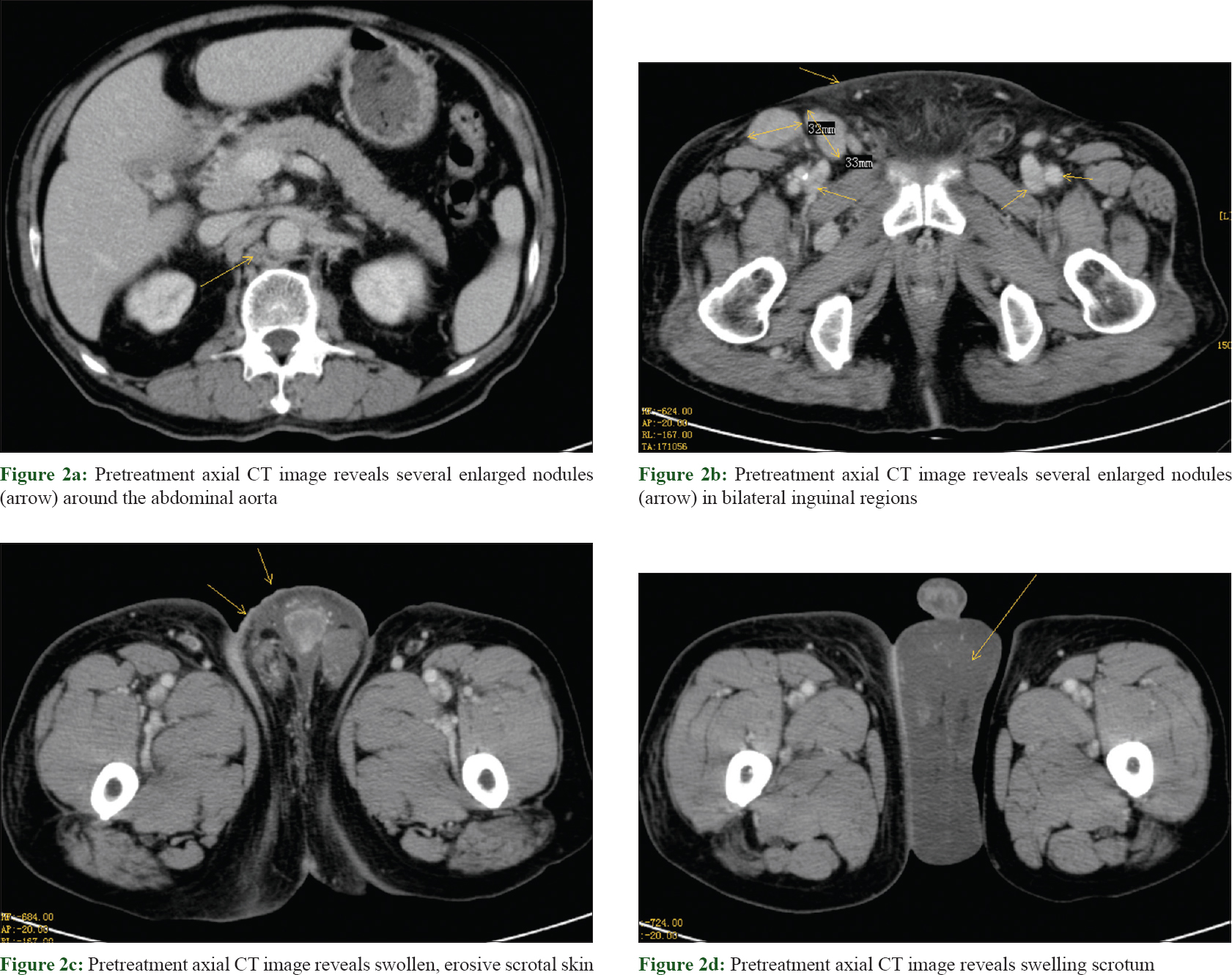 |
| Figure 2 |
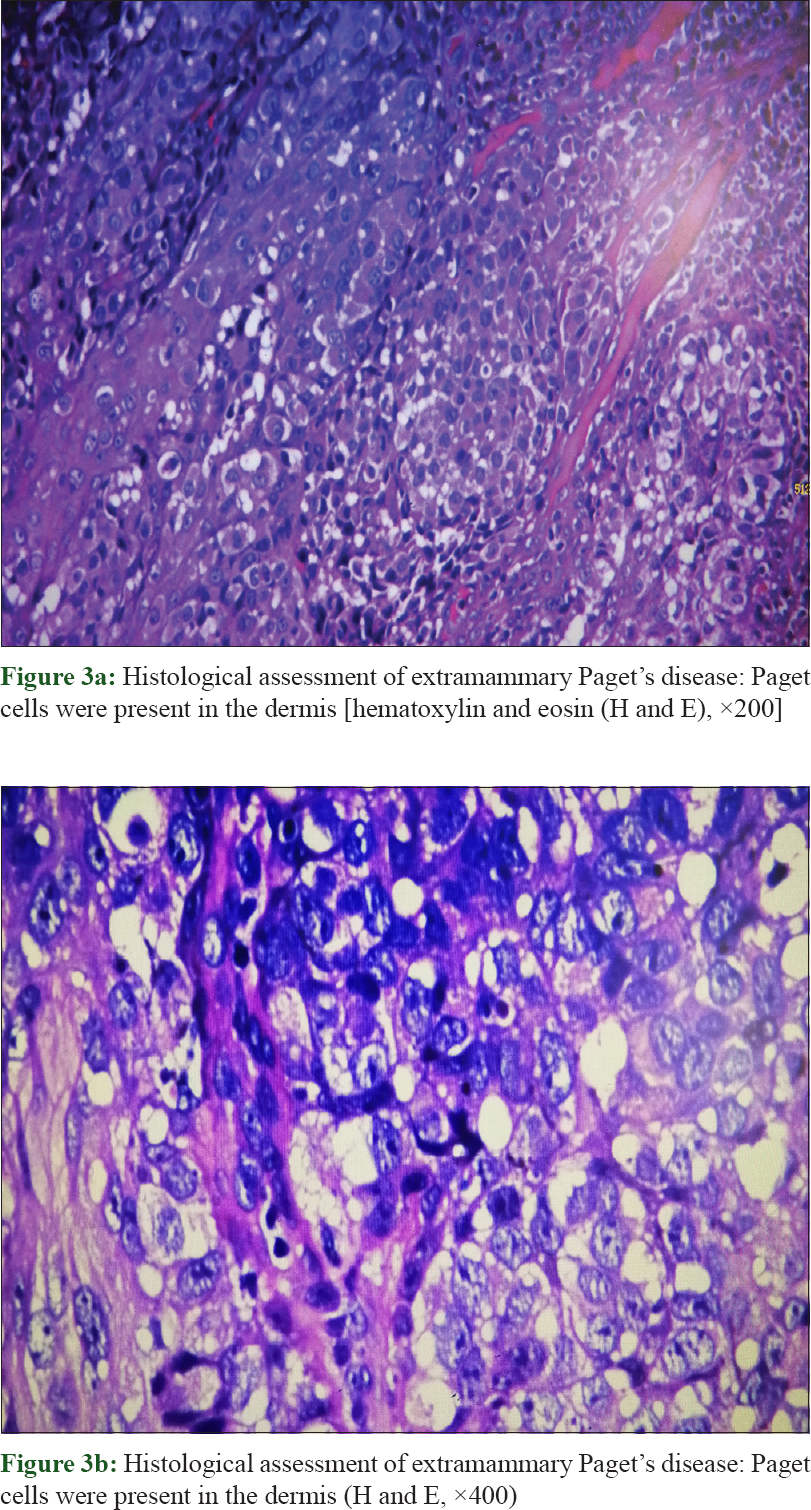 |
| Figure 3 |
During evaluation, the tumor was found to be unresectable. Chemotherapy was started after obtaining informed consent from the patient in the form of topical 5-fluorouracil (5-FU) [25 mg/ml] and systemic pemetrexed (0.5 g/m2 d1 q21d). The patient reported gradual remission of itchiness and swelling with regular use of topical 5-FU [Figure - 1]b. The first cycle of pemetrexed (0.5 g/m2 d1 q21d) was uneventful except for occurrence of mild fatigue. After two cycles of chemotherapy, the CT scan demonstrated significant reduction in the size of metastatic lymph nodes (inguinal and the para-vascular regions). The patient received six cycles of treatment, and the disease remained stable as evaluated by CT Scan [Figure - 4].
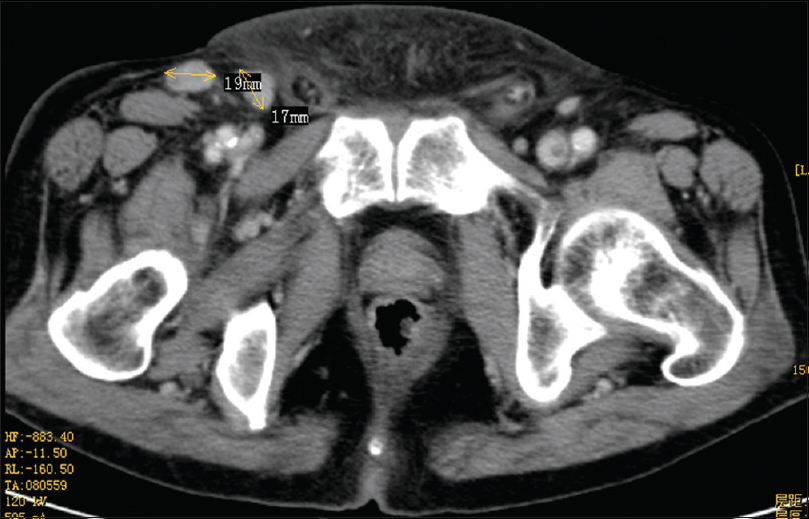 |
| Figure 4: Follow-up CT six cycles later demonstrated our regimen is significant, that the lymphatic metastasis decreased in size |
Discussion
Extramammary Paget's disease accounts for a small proportion of Paget's disease, which is only about 6.5%.[1] There are several theories explaining the pathogenesis of this rare condition. Mehta et al suspected it to be a metastatis derived from some kind of undetected, underlying malignant tumor,[2] and reported that up to 42% of the cases have associated underlying malignancy.[3] Hatta et al stated that the metastasis correlated with the differentiation of the exocrine or the apocrine system.[4] However, none of the above theories have been confirmed so far.
Most cases affect the 65–70 year age-group, with female predominance in Europe, in contrast to the Asian population where extramammary paget's disease develops most frequently in males.[5] The apocrine-rich glands in the penis, scrotum, vulva, axilla and the perineum are the usual affected areas, and the vulva, accounting for 65% of the extramammary paget's disease cases, ranks as the most common site.[6]
With the exception of few cases showing tumor invasion into the dermis or migration into other organs, most tumors are found in situ and are resectable on diagnosis. The site, size, location, staging and grading of the tumor are all important for risk stratification and treatment. Various options are available for its treatment including surgical excision, chemotherapy, radiotherapy, photodynamic therapy and ablation. Surgery is the primary, crucial and standard treatment for local disease, but recurrence rate after surgical therapy is reported to be as high as 30–60%, which might be attributed to the tumor's positive margins.[7] For advanced cases, no standard treatment guideline has been established yet, although few regimens have been reported to be effective. Yamazaki et al reported a combination chemotherapy regimen including mitomycin, epirubicin, vincristine and 5-FU,[8] while Kajihara et al. combined S-1 and docetaxel.[9] In addition, FOLFOX, trastuzumab, and paclitaxel combinations have been proven to be effective for tumor treatment as well.[7] Although combination chemotherapy can have positive outcomes, it is frequently associated with highly toxic adverse effects like anorexia, alopecia and leukopenia (neutropenia); therefore, its use requires further investigation and longer follow-up.
To treat local skin irritation, erythema and erosions, surgery is normally the first treatment choice, but for patients with widespread metastasis, alternative modalities need to be considered. Imiquimod 5% cream has been reported to be an effective therapeutic modality for unresectable primary or recurrent tumors.[10] However, imiquimod 5% cream is recommended to be applied topically three times per week for 16 weeks, and this long duration may be inconvenient for in-house patients. In this article, we report effective treatment of the skin lesion with 5-FU with symptomatic and clinical improvement reported after 10 days. Moreover, we decided to use monotherapy of low-dose pemetrexed as systemic chemotherapy. Pemetrexed is the antimetabolite of folate, which is widely used nowadays as chemotherapy agent for managing non-small cell lung cancer and pleural mesothelioma. This drug was well tolerated by the patient without any occurrence of adverse effects like neutropenia, thrombocytopenia, nausea or vomiting during the treatment. We recommend using pemetrexed in the systemic chemotherapy treatment of metastatic extramammary Paget's disease, especially for those cases who cannot physically tolerate combination chemotherapy. We also suggest additional topical administration of 5-FU, which is a noninvasive, convenient and effective treatment choice.
Due to low incidence of the disease, we cannot compare the efficacy and survival advantage among patients of different age, sex, race, nor demonstrate superiority of this regimen as first-line treatment in terms of progression-free survival.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Wu C, Tao HT, Li FF, Huang SW, Dong WW, Wang JL, et al. Pemetrexed induced a durable response in heavily pretreated metastatic extramammary Paget's disease. Int J Clin Exp Med 2015;8:9595-8.
[Google Scholar]
|
| 2. |
Mehta NJ, Torno R, Sorra T. Extramammary Paget's disease. South Med J 2000;93:713-5.
[Google Scholar]
|
| 3. |
Park S, Grossfeld GD, McAninch JW, Santucci R. Extramammary Paget's disease of the penis and scrotum: Excision, reconstruction and evaluation of occult malignancy. J Urol 2001;166:2112-6.
[Google Scholar]
|
| 4. |
Hatta N, Yamada M, Hirano T, Fujimoto A, Morita R. Extramammary Paget's disease: Treatment, prognostic factors and outcome in 76 patients. Br J Dermatol 2008;158:313-8.
[Google Scholar]
|
| 5. |
Cheng PS, Lu CL, Cheng CL and Lai FJ: Significant male predisposition in extramammary Paget disease: A nationwide population-based study in Taiwan. Br J Dermatol 2014; 171: 191-193.
[Google Scholar]
|
| 6. |
Kanitakis J. Mammary and extramammary Paget's disease. J Eur Acad Dermatol Venereol 2007;21:581-90.
[Google Scholar]
|
| 7. |
Al HM, Zouain N. Extramammary perianal Paget's disease. Case Rep Gastroenterol 2009;3:332-7.
[Google Scholar]
|
| 8. |
Yamazaki N, Yamamoto A, Wada T, Ishikawa M, Moriya Y, Nakanishi Y, et al. Acase of metastatic extramammary Paget's disease that responded to combination chemotherapy. J Dermatol 1999;26:311-6.
[Google Scholar]
|
| 9. |
Kajihara I, Kanemaru H, Miyake T, Aoi J, Masuguchi S, Fukushima S, et al. Combination chemotherapy with S-1 and docetaxel for cutaneous angiosarcoma resistant to paclitaxel. Drug Discov Ther 2015;9:75-7.
[Google Scholar]
|
| 10. |
Zampogna JC, Flowers FP, Roth WI, Hassenein AM. Treatment of primary limited cutaneous extramammary Paget's disease with topical imiquimod monotherapy: Two case reports. J Am Acad Dermatol 2002;47:S229-35.
[Google Scholar]
|
Fulltext Views
3,927
PDF downloads
3,168





