Translate this page into:
Superficial white onychomycosis due to Trichophyton rubrum in a two-year-old child
Correspondence Address:
Wu Jianhua
Department of Dermatology, Changhai Hospital, Second Military Medical University, Shanghai-200433
China
| How to cite this article: Yu G, Jianhua W. Superficial white onychomycosis due to Trichophyton rubrum in a two-year-old child. Indian J Dermatol Venereol Leprol 2013;79:269 |
Sir,
Superficial white onychomycosis (SWO) due to Trichophyton rubrum is rare in children. We report a case of leukonychia of the 5 toes of one-month duration in a 2-year-old boy patient. On KOH examination, fungal hyphae were seen, and culture showed growth of Trichophyton rubrum. All toenails also showed almost complete clinical and mycological cure after 3 months of 1% Bifonazole cream topical therapy.
A 2-year-old boy was brought to our department with chief complaints of progressive whitish changes of his toenails of one-month duration. Physical examination found opaque, whitish patches on the surface of his first to third toenails on the left foot, and first to second toenails on the right foot [Figure - 1]. Fingernails were spared. Cutaneous examination revealed no other skin lesion of fungal infection, except there was erythema and mild exfoliation on the toes around nails. But, he didn′t feel pruritus. Systemic examination was within the normal limits, no other disease and no a history of application of immunosuppressant. But, there was a positive family history of tinea pedis in his father and grandmother. Direct microscopic examination of superficial nail scrapings with KOH showed numerous long hyaline septate-branched fungal hyphae along with conidia, confirming dermatophyte infection [Figure - 2]. Culture of the material yielded a colony, which is white, downy colony, and yellowish pigmentation from reverse [Figure - 2]. Microscopically, there were many chlamydoconidia and a few teardrop-shaped microconidia [Figure - 2]. So, a diagnosis of superficial white onychomycosis due to Trichophyton rubrum was made.
 |
| Figure 1: Before treatment: (a) First to third toenails on the left foot and first to second toenails on the right foot with many white patches on the surface of the toenails. Besides, erythema and mild exfoliation on the toes around nails. After 3 months of treatment: (b) All toenails were normal |
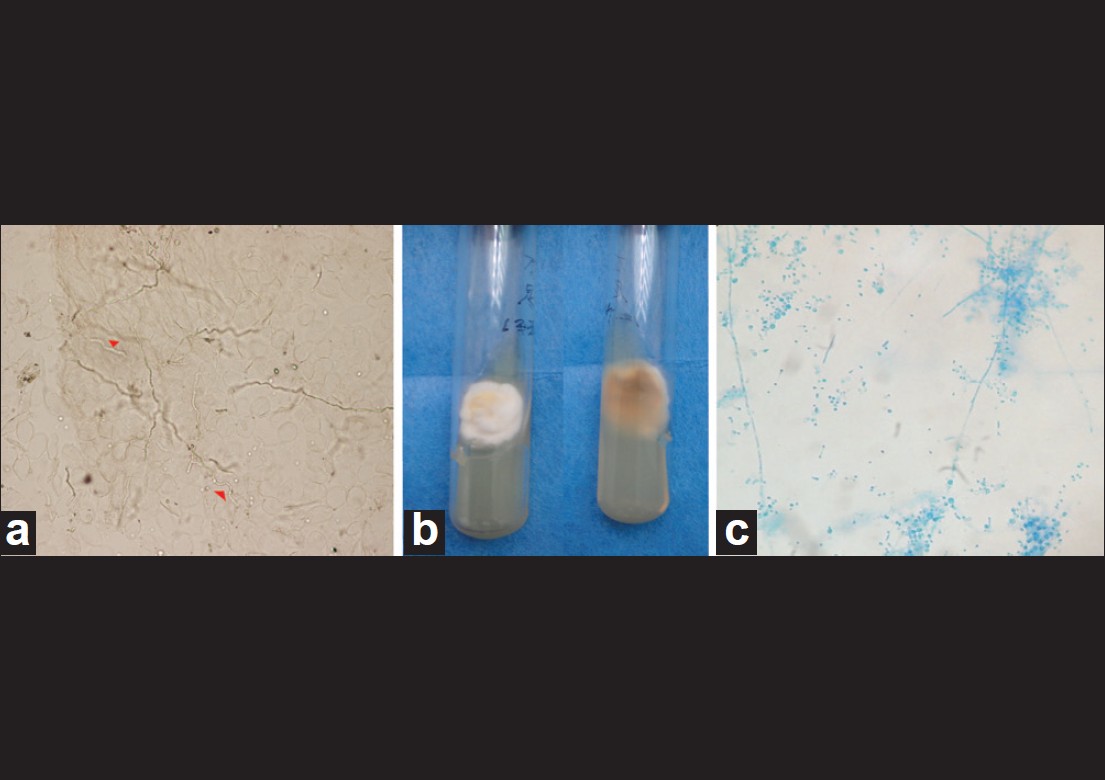 |
| Figure 2: (a) Direct microscopic examination of superficial nail scrapings showing hyaline-branched septate fungal hyphae and a few conidia (Potassium hydroxide, ×40). (b) The texture of Trichophyton rubrum colony. (c) Lactophenol cotton blue preparation of the culture showing typical chlamydoconidia and teardrop-shaped microconidia of Trichophyton rubrum micrograph (Potassium hydroxide, ×40) |
The patient was treated with 1% Bifonazole cream on each affected nail, 2 times a day, for 3 months. After 30 days of treatment, marked improvement was seen in all the 5 nails and the skin around the nails. No side-effects of the administered drug were seen. All toenails also showed almost complete clinical and mycological cure after 3 months of therapy [Figure - 1].
Onychomycosis is the general term for fungal infections of the nail caused by dermatophytes, non-dermatophytic moulds (NDM), or yeast. It includes 5 types: Distal lateral subungual onychomycosis (DLSO), superficial white onychomycosis (SWO), proximal subungual onychomycosis (PSO), total dystrophic onychomycosis (TDO), and endonyx onychomycosis (EO). Onychomycosis is considered an age-related infection with increasing prevalence in the older age groups. It is extremely rare in children although the prevalence tended to increase over the years. [1] This may be explained by children′s more rapid nail growth rate, smaller contact surface, lower incidence of tinea pedis, and infrequent exposure to fungi. [2] SWO is an uncommon form of fungal nail infection, with various series reporting an incidence of 1.5% - 7% of all cases of onychomycosis. [3] In addition, SWO has been reported to be caused mainly by Trichophyton mentagrophytes, Trichophyton interdigitale, and Candida species and rarely by Fusarium, Aspergillus and Cladosporium species, and dermatophytes including Trichophyton rubrum and Trichophyton verrucosum.[4] But, in our case, we found a 2-year-old child with SWO as a result of Trichophyton rubrum, which is rarely reported in literature. In children less than 2 years old having onychomycosis, Bonifaz found an association with Down′s syndrome, fungal infection on other body parts, premature birth, perinatal hypoxia, and infection in other family members. [5] It is said many SWO patients have a family history of tinea pedis or Trichophyton rubrum onychomycosis, which suggests a genetic susceptibility to dermatophyte infection contracted in the familial environment. [4] We also found the grandmother and father of the children has tinea pedis, but unfortunately, we couldn′t get any samples from them. So, we couldn′t know if it was caused by Trichophyton rubrum. But, we still think the SWO of the child in our case is the infection from his family.
Generally, systemic therapy is almost always more successful than topical treatment. But, for children, parents prefer to accept topical treatment than oral antifungal, because topical treatment has obvious advantages in avoiding systemic side-effects or drug interactions, especially for children. And, classical SWO is one of the indications for topical treatment of onychomycosis. [4] Probably because there is no nail bed or matrix involvement, and the nail plate is thinner in children, this may facilitate penetration of the drug. Moreover, children′s nails grow faster than adults. So, in our case, the patient was treated successfully twice-daily with 1% bifonazole cream therapy for 3 months.
Our case showed complete morphological and mycological cure in 3 months without any side-effects. Therefore, we think topical therapy is a good and safe method for the SWO of young children.
| 1. |
Rodríguez-Pazos L, Pereiro-Ferreirós MM, Pereiro M Jr, Toribio J. Onychomycosis observed in children over a 20-year period. Mycoses 2011;54:450-3.
[Google Scholar]
|
| 2. |
Baran R, Dawber RP, de Berker DA. The nail in childhood and old age. In: Baran R, Dawber RP, editors. Nails diseases and their management. 3 rd ed. Oxford: Blackwell Science; 2001. p. 104-28.
[Google Scholar]
|
| 3. |
Garg A, Venkatesh V, Singh M, Pathak KP, Kaushal GP, Agrawal SK. Onychomycosis in central India: A clinicoetiologic correlation. Int J Dermatol 2004;43:498-502.
[Google Scholar]
|
| 4. |
Piraccini BM, Tosti A. White superficial onychomycosis: Epidemiological, clinical, and pathological study of 79 patients. Arch Dermatol 2004;140:696-701.
[Google Scholar]
|
| 5. |
Bonifaz A, Saúl A, Mena C. Dermatophyte onychomycosis in children under 2 years of age: Experience of 16 cases. J Eur Acad Dermatol Venereol 2007;21:115-7.
[Google Scholar]
|
Fulltext Views
2,197
PDF downloads
2,251





