Translate this page into:
Ten clinical clues for the diagnosis of frontal fibrosing alopecia
2 Departament of Dermatology, General Hospital of Santa Casa de Misericórdia do Rio de Janeiro, Rio de Janeiro, Brazil
3 Departament of Dermatology, Army Central Hospital, Rio de Janeiro, Brazil
4 Departament of Dermatology, Marcílio Dias Naval Hospital, Rio de Janeiro, Brazil
Correspondence Address:
Elaine de Souza Albernaz
Ituverava Street, 1138, Freguesia, Jacarepaguá, Rio De Janeiro
Brazil
| How to cite this article: Melo DF, de Mattos Barreto T, de Souza Albernaz E, Haddad NC, Tortelly VD. Ten clinical clues for the diagnosis of frontal fibrosing alopecia. Indian J Dermatol Venereol Leprol 2019;85:559-564 |
Frontal fibrosing alopecia was described by Kossard as a progressive scarring alopecia along the frontotemporal hairline.[1] It was initially thought to occur with postmenopausal women,[1],[2],[3] however, the description of its occurrence in premenopausal women has been on the rise.[4] Its incidence in male patients has rarely been described.[5],[6],[7],[8] Although it is considered a variant of lichen planopilaris due to the similarity of the prominent histopathological findings, the pathogenesis of frontal fibrosing alopecia is not completely elucidated yet.[1],[5],[6],[7],[9],[10],[11] It is believed that an autoimmune reaction against the pilosebaceous unit, as well as hormonal factors, may be involved in the etiopathogenesis of the disease.[12] However, reports of familial cases suggest a genetic susceptibility with probable environmental triggers.[5],[6],[13],[14]
The association of frontal fibrosing alopecia with androgenetic alopecia and autoimmune diseases such as hypothyroidism, vitiligo, Sjögren's syndrome and chronic cutaneous lupus erythematosus has been reported in global literature.[3],[5],[15],[16] A relationship between frontal fibrosing alopecia and the use of facial cosmetics was recently postulated.[17] Facelifts and hair transplantion also, reportedly, trigger the disease.[18],[19]
Clinically, frontal fibrosing alopecia affects the frontotemporal hairline, making its differentiation from male androgenetic alopecia and marginal alopecia areata in that location, difficult. Frontal fibrosing alopecia can also generate areas of alopecia in the auricular margins and, less frequently, may affect the occipital region.[2],[3],[5],[7],[10]
Patients may present loss of eyebrows in 50–80% of cases, involvement of eyelashes in 15% and can present with progressive and generalized disappearance of body hair.[2],[3],[5],[11],[20],[21] Typically, loss of eyebrows and body hairs does not exhibit the classical inflammatory signs of erythema and perifollicular scaling.
Most patients are asymptomatic, although pruritus, pain and burning can be observed at affected sites.[5] As a primary cicatricial alopecia with a potential for irreversible damage to affected scalp areas, biopsy and histopathological confirmation is essential. Trichoscopy (dermoscopy of the scalp) and its findings increase diagnostic accuracy, and are useful in determining the best site for scalp biopsy, proving to be a valuable tool to assess disease activity, on follow-up consultations. The characteristic findings in trichoscopy of frontal fibrosing alopecia are erythema with perifollicular scaling in the peripheral part of the alopecic area, absence of vellus hairs and reduction of the number of follicular ostia. In addition, the presence of branched capillaries, honeycomb pattern of pigmentation and white dots have been described.[6],[7],[22],[23]
Due to its insidious course, in some cases the late recognition of the disease and consequent delay in the institution of treatment could affect the evolution and prognosis of cases.[24]
The purpose of this study is to describe and illustrate 10 clinical clues that can facilitate the identification of frontal fibrosing alopecia, aiming that residents having their first contacts with hair diseases would be able to formulate the diagnostic hypothesis of frontal fibrosing alopecia only from their clinical examination, even without complementary tools such as trichoscopy. Frontal fibrosing alopecia has been described only two decades ago, having increasing incidence in recent years. Proper clinical evaluation, leading to early and correct diagnosis, is fundamental to establish adequate treatment that can minimize symptoms, disease progression, scars and the impact on quality of life.[25]
- High hairline is a critical finding for frontal fibrosing alopecia diagnosis. Fronto-parieto-temporal hairline recession [1],[5],[6],[7],[10],[22],[24] usually develops bilaterally and symmetrically,[5],[10] and it can extend through to the retroauricular region and occipital margin [Figure - 1]. Additionally, frontal fibrosing alopecia may cause pain, itching or burning sensations in the band across the frontal hairline.[5],[7],[10]
- Skin color difference: The area affected by frontal fibrosing alopecia presents as pale skin with no follicular ostia, in contrast to normal facial skin which shows more signs of photodamage.[1] Hypopigmentation can be better visualized with the aid of a Wood's lamp [Figure - 2].[26]
- Contraction of the frontal muscle represents a simple and useful semiological maneuver that can be helpful in determining the extension of hairline recession, by precising the limits between facial and scalp areas. Contraction can be promoted by requesting the patient to raise the eyebrows. This measure allows the differentiation between frontal wrinkles and the marginal region of the scalp, thus enabling quantification of the hairline retraction area [Figure - 3].[27]
- Bilateral eyebrow loss is another clinical warning sign for frontal fibrosing alopecia, and may represent one of the earliest manifestations which could precede alopecia by several months to years.[5],[28] The distal third is commonly affected [6],[7] and, unlike the scalp, it is unusual to find evident erythema or scaling on the eyebrow area.[11] Eyelash loss may also occur, albeit less frequently,[5],[7],[10] and appears to be related to more severe forms of frontal fibrosing alopecia.[5] This finding could, therefore, be effective as a prognostic marker and it may be considered, by some, as indicative for initiation of systemic treatment [Figure - 4].[6]
- More evident frontal veins can be detected by palpation as a localized depression, near the original hairline. Cutaneous atrophy is thought to be responsible, in addition, by the use of topical steroids [Figure - 5].[26],[29]
- The disappearance of the vellus (fine, thin and light-colored hairs) at the scalp hairline is a relevant clinical and trichoscopic finding which corroborates the peculiar histopathological finding of early involvement and destruction of these follicles by a lymphocytic infiltrate [Figure - 6] and [Figure - 7].[11],[23]
- Lonely hairs: After progressive disappearance of vellus hairs on the frontal region, persistence of some isolated terminal hairs in the original hairline become evident, measuring 3–7 cm and may present perifollicular erythema and scaling [Figure - 8].[21],[25]
- Pseudofringe sign is a retention of hairs along the frontotemporal hairline with a clinical aspect similar to the fringe sign, present in traction alopecia.[30] This sign, although infrequent, is apparently related to a good prognosis with less severe scalp involvement, greater sparing of eyebrows and less frequent facial papules [Figure - 9].[31]
- Facial papules in frontal fibrosing alopecia were described as follicular, normochromic and monomorphic papules,[32] representing the involvement of facial vellus hair, and are present in 6–37% of the cases.[5],[33],[34] They are randomly distributed on facial skin and are not easily noticed, being better visualized over the temples.[35] Involvement of the inframandibular and retroauricular areas can also occur, helping in differentiation from photodamaged skin.[33] These papules are associated with more severe forms of frontal fibrosing alopecia [Figure - 10].[5],[6]
- Association with lichen planus pigmentosus: It is characterized by hyperpigmented macules with colors ranging from brown to blue-grayish and a reticulated or diffuse appearance, predominating over photoexposed areas. It occurs frequently in patients with higher skin phototypes and may precede the manifestations of the disease in the scalp. In the presence of facial hyperpigmentation in these patients, the possibility of lichen planus pigmentosus must be considered [Figure - 11].[35],[36],[37]
 |
| Figure 1: Patient with a high hair implantation line |
 |
| Figure 2: Patient with an evident difference in the appearance of marginal region skin |
 |
| Figure 3: Patient contracting the frontal muscle, allowing the differentiation between frontal wrinkles and the marginal region of the scalp |
 |
| Figure 4: Patient with both eyebrow and eyelash loss. She resorted to micropigmentation of the eyebrows in order to cover up the hair loss in the region |
 |
| Figure 5: Patient with evident frontal veins. It is important to emphasize that this patient started the frontal fibrosing alopecia signs after having undergone a facelift procedure |
 |
| Figure 6: Patient without vellus hair at the capillary implantation border |
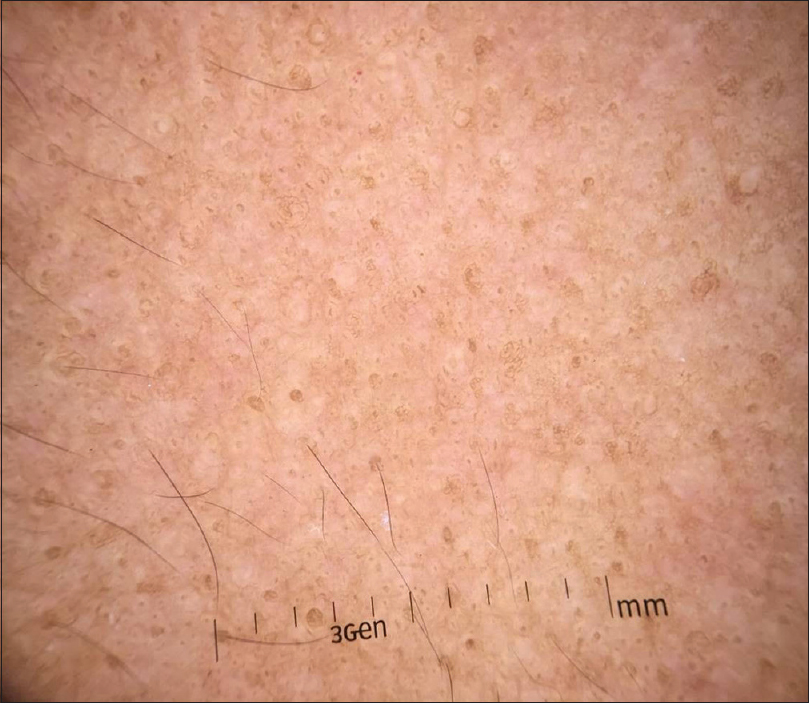 |
| Figure 7: Trichoscopy evidencing the absence of vellus hairs in the capillary implantation line |
 |
| Figure 8: Patient with isolated terminal hairs (lonely hairs) over the original hairline |
 |
| Figure 9: Patient with terminal hairs grouped over the original hairline (pseudo fringe sign) |
 |
| Figure 10: Patient with facial normochromic and monomorphic papules |
 |
| Figure 11: Patient with blue-grayish macules on the face, whose histopathological examination was compatible with lichen planus pigmentosus |
Conclusion
Frontal fibrosing alopecia is a recently described disease and subsequent studies are still needed to better understand its causes and triggering factors. Its predominance in women is a well-defined aspect, and its cicatricial and irreversible character enhances the importance of early recognition.
Because there are no established diagnostic criteria for frontal fibrosing alopecia, the purpose of this study is to summarize the most relevant clinical findings of this disease by highlighting 10 clinical clues, contributing to a better recognition of the disease, and leading to diagnostic suspicion in initial cases, thus, minimizing scars and the psychosocial impact. However, it should be emphasized that studies are still needed to determine the sensitivity and specificity of these clinical findings for the diagnosis of the disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kossard S. Postmenopausal frontal fibrosing alopecia. Scarring alopecia in a pattern distribution. Arch Dermatol 1994;130:770-4.
[Google Scholar]
|
| 2. |
Kossard S, Lee MS, Wilkinson B. Postmenopausal frontal fibrosing alopecia: A frontal variant of lichen planopilaris. J Am Acad Dermatol 1997;36:59-66.
[Google Scholar]
|
| 3. |
MacDonald A, Clark C, Holmes S. Frontal fibrosing alopecia: A review of 60 cases. J Am Acad Dermatol 2012;67:955-61.
[Google Scholar]
|
| 4. |
Elloudi S, Gallouj S, Meziane M, Mernissi FZ, Rimani M. Frontal fibrosing alopecia: A prospective study of 20 cases. Ann Dermatol Venereol 2017;144:409-14.
[Google Scholar]
|
| 5. |
Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, Arias-Santiago S, Rodrigues-Barata AR, Garnacho-Saucedo G, et al. Frontal fibrosing alopecia: A multicenter review of 355 patients. J Am Acad Dermatol 2014;70:670-8.
[Google Scholar]
|
| 6. |
Esteban-Lucía L, Molina-Ruiz AM, Requena L. Update on frontal fibrosing alopecia. Actas Dermosifiliogr 2017;108:293-304.
[Google Scholar]
|
| 7. |
Moreno-Ramírez D, Ferrándiz L, Camacho FM. Diagnostic and therapeutic assessment of frontal fibrosing alopecia. Actas Dermosifiliogr 2007;98:594-602.
[Google Scholar]
|
| 8. |
Callender VD, Reid SD, Obayan O, Mcclellan L, Sperling L. Diagnostic clues to frontal fibrosing alopecia in patients of African descent. J Clin Aesthet Dermatol 2016;9:45-51.
[Google Scholar]
|
| 9. |
Olsen EA, Bergfeld WF, Cotsarelis G, Price VH, Shapiro J, Sinclair R, et al. Summary of North American Hair Research Society (NAHRS)-sponsored workshop on cicatricial alopecia, Duke University Medical Center, February 10 and 11, 2001. J Am Acad Dermatol 2003;48:103-10.
[Google Scholar]
|
| 10. |
Tziotzios C, Stefanato CM, Fenton DA, Simpson MA, McGrath JA. Frontal fibrosing alopecia: Reflections and hypotheses on aetiology and pathogenesis. Exp Dermatol 2016;25:847-52.
[Google Scholar]
|
| 11. |
Chew AL, Bashir SJ, Wain EM, Fenton DA, Stefanato CM. Expanding the spectrum of frontal fibrosing alopecia: A unifying concept. J Am Acad Dermatol 2010;63:653-60.
[Google Scholar]
|
| 12. |
Jimenez F, Harries M, Poblet E. Frontal fibrosing alopecia: A disease fascinating for the researcher, disappointing for the clinician and distressing for the patient. Exp Dermatol 2016;25:853-4.
[Google Scholar]
|
| 13. |
Navarro-Belmonte MR, Navarro-López V, Ramírez-Boscà A, Martínez-Andrés MA, Molina-Gil C, González-Nebreda M, et al. Case series of familial frontal fibrosing alopecia and a review of the literature. J Cosmet Dermatol 2015;14:64-9.
[Google Scholar]
|
| 14. |
Dlova N, Goh CL, Tosti A. Familial frontal fibrosing alopecia. Br J Dermatol 2013;168:220-2.
[Google Scholar]
|
| 15. |
Gaffney DC, Sinclair RD, Yong-Gee S. Discoid lupus alopecia complicated by frontal fibrosing alopecia on a background of androgenetic alopecia. Br J Dermatol 2013;169:217-8.
[Google Scholar]
|
| 16. |
del Rei M, Pirmez R, Sodré CT, Tosti A. Coexistence of frontal fibrosing alopecia and discoid lupus erythematosus of the scalp in 7 patients: Just a coincidence? J Eur Acad Dermatol Venereol 2016;30:151-3.
[Google Scholar]
|
| 17. |
Aldoori N, Dobson K, Holden CR, McDonagh AJ, Harries M, Messenger AG, et al. Frontal fibrosing alopecia: Possible association with leave-on facial skin care products and sunscreens; a questionnaire study. Br J Dermatol 2016;175:762-7.
[Google Scholar]
|
| 18. |
Kossard S, Shiell RC. Frontal fibrosing alopecia developing after hair transplantation for androgenetic alopecia. Int J Dermatol 2005;44:321-3.
[Google Scholar]
|
| 19. |
Chiang YZ, Tosti A, Chaudhry IH, Lyne L, Farjo B, Farjo N, et al. Lichen planopilaris following hair transplantation and face-lift surgery. Br J Dermatol 2012;166:666-370.
[Google Scholar]
|
| 20. |
Armenores P, Shirato K, Reid C, Sidhu S. Frontal fibrosing alopecia associated with generalized hair loss. Australas J Dermatol 2010;51:183-5.
[Google Scholar]
|
| 21. |
Tosti A, Miteva M, Torres F. Lonely hair: A clue to the diagnosis of frontal fibrosing alopecia. Arch Dermatol 2011;147:1240.
[Google Scholar]
|
| 22. |
Salido-Vallejo R, Garnacho-Saucedo G, Moreno-Gimenez JC, Camacho-Martinez FM. Beard involvement in a man with frontal fibrosing alopecia. Indian J Dermatol Venereol Leprol 2014;80:542-4.
[Google Scholar]
|
| 23. |
Lacarrubba F, Micali G, Tosti A. Absence of vellus hair in the hairline: A videodermatoscopic feature of frontal fibrosing alopecia. Br J Dermatol 2013;169:473-4.
[Google Scholar]
|
| 24. |
Fertig R, Tosti A. Frontal fibrosing alopecia treatment options. Intractable Rare Dis Res 2016;5:314-5.
[Google Scholar]
|
| 25. |
Chiang YZ, Bundy C, Griffiths CE, Paus R, Harries MJ. The role of beliefs: Lessons from a pilot study on illness perception, psychological distress and quality of life in patients with primary cicatricial alopecia. Br J Dermatol 2015;172:130-7.
[Google Scholar]
|
| 26. |
Lin J, Valdebran M, Bergfeld W, Conic RZ, Piliang M, Atanaskova Mesinkovska N, et al. Hypopigmentation in frontal fibrosing alopecia. J Am Acad Dermatol 2017;76:1184-6.
[Google Scholar]
|
| 27. |
Mirmirani P, Zimmerman B. Cocking the eyebrows to find the missing hairline in frontal fibrosing alopecia: A useful clinical maneuver. J Am Acad Dermatol 2016;75:e63-4.
[Google Scholar]
|
| 28. |
Anzai A, Donati A, Valente NY, Romiti R, Tosti A. Isolated eyebrow loss in frontal fibrosing alopecia: Relevance of early diagnosis and treatment. Br J Dermatol 2016;175:1099-101.
[Google Scholar]
|
| 29. |
Vañó-Galván S, Rodrigues-Barata AR, Urech M, Jiménez-Gómez N, Saceda-Corralo D, Paoli J, et al. Depression of the frontal veins: A new clinical sign of frontal fibrosing alopecia. J Am Acad Dermatol 2015;72:1087-8.
[Google Scholar]
|
| 30. |
Pirmez R, Duque-Estrada B, Abraham LS, Pinto GM, de Farias DC, Kelly Y, et al. It's not all traction: The pseudo 'fringe sign' in frontal fibrosing alopecia. Br J Dermatol 2015;173:1336-8.
[Google Scholar]
|
| 31. |
Moreno-Arrones OM, Saceda-Corralo D, Fonda-Pascual P, Rodrigues-Barata AR, Buendía-Castaño D, Alegre-Sánchez A, et al. Frontal fibrosing alopecia: Clinical and prognostic classification. J Eur Acad Dermatol Venereol 2017;31:1739-45.
[Google Scholar]
|
| 32. |
Tan KT, Messenger AG. Frontal fibrosing alopecia: Clinical presentations and prognosis. Br J Dermatol 2009;160:75-9.
[Google Scholar]
|
| 33. |
Donati A, Molina L, Doche I, Valente NS, Romiti R. Facial papules in frontal fibrosing alopecia: Evidence of vellus follicle involvement. Arch Dermatol 2011;147:1424-7.
[Google Scholar]
|
| 34. |
López-Pestaña A, Tuneu A, Lobo C, Ormaechea N, Zubizarreta J, Vildosola S, et al. Facial lesions in frontal fibrosing alopecia (FFA): Clinicopathological features in a series of 12 cases. J Am Acad Dermatol 2015;73:987.e1-6.
[Google Scholar]
|
| 35. |
Pirmez R, Duque-Estrada B, Donati A, Campos-do-Carmo G, Valente NS, Romiti R, et al. Clinical and dermoscopic features of lichen planus pigmentosus in 37 patients with frontal fibrosing alopecia. Br J Dermatol 2016;175:1387-90.
[Google Scholar]
|
| 36. |
Dlova NC. Frontal fibrosing alopecia and lichen planus pigmentosus: Is there a link? Br J Dermatol 2013;168:439-42.
[Google Scholar]
|
| 37. |
Berliner JG, McCalmont TH, Price VH, Berger TG. Frontal fibrosing alopecia and lichen planus pigmentosus. J Am Acad Dermatol 2014;71:e26-7.
[Google Scholar]
|
Fulltext Views
17,308
PDF downloads
6,672





