Translate this page into:
Toxic epidermal necrolysis predominantly involving irradiated site in a carcinoma breast patient – An example of immunocompromised cutaneous district
Corresponding author: Dr. Preema Sinha, Department of Dermatology, Base Hospital, Lucknow, India. sinhapreema@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sinha P, Sharma J, GB Prashantha, Toor SS, Kamboj P. Toxic epidermal necrolysis predominantly involving irradiated site in a carcinoma breast patient – An example of immunocompromised cutaneous district. Indian J Dermatol Venereol Leprol. 2025;91:234-6. doi: 10.25259/IJDVL_310_2023
Dear Editor
Toxic epidermal necrolysis is a potentially life-threatening condition which requires prompt evaluation and appropriate management. A recent study of erythema multiforme, Stevens–Johnson syndrome and toxic epidermal necrolysis in patients undergoing radiotherapy showed anticonvulsants being the most common drug associated with radiotherapy and these reactions.1 We present a case of toxic epidermal necrolysis in a known case of breast carcinoma receiving radiotherapy with carbamazepine and predominant initial localisation of skin lesions to the site of irradiation.
A 58-year-old female, a known case of hypertension and carcinoma breast, received chemotherapy for 6 months. Later, she was treated with palliative radiation therapy to her left breast for 25 days. She also received tab carbamazepine 500 mg daily for right hemifacial pain. Ten days later, she developed multiple fluid filled lesions over the well demarcated area of irradiation on the left side of the chest, along with painful raw areas involving the lips, buccal mucosa, hard palate and nasal mucosa. Nikolsky’s sign was positive. Palms and soles showed mild erythema. Eye examination revealed conjunctival suffusion in both eyes. The lesions were initially confined only to areas of skin corresponding to the radiation field [Figure 1a]. Within the next 48 hours, skin lesions progressed with similar blisters occurring on her trunk, extremities and face associated with intense pain [Figure 1b]. Multiple atypical targetoid lesions were seen on the extremities and trunk.
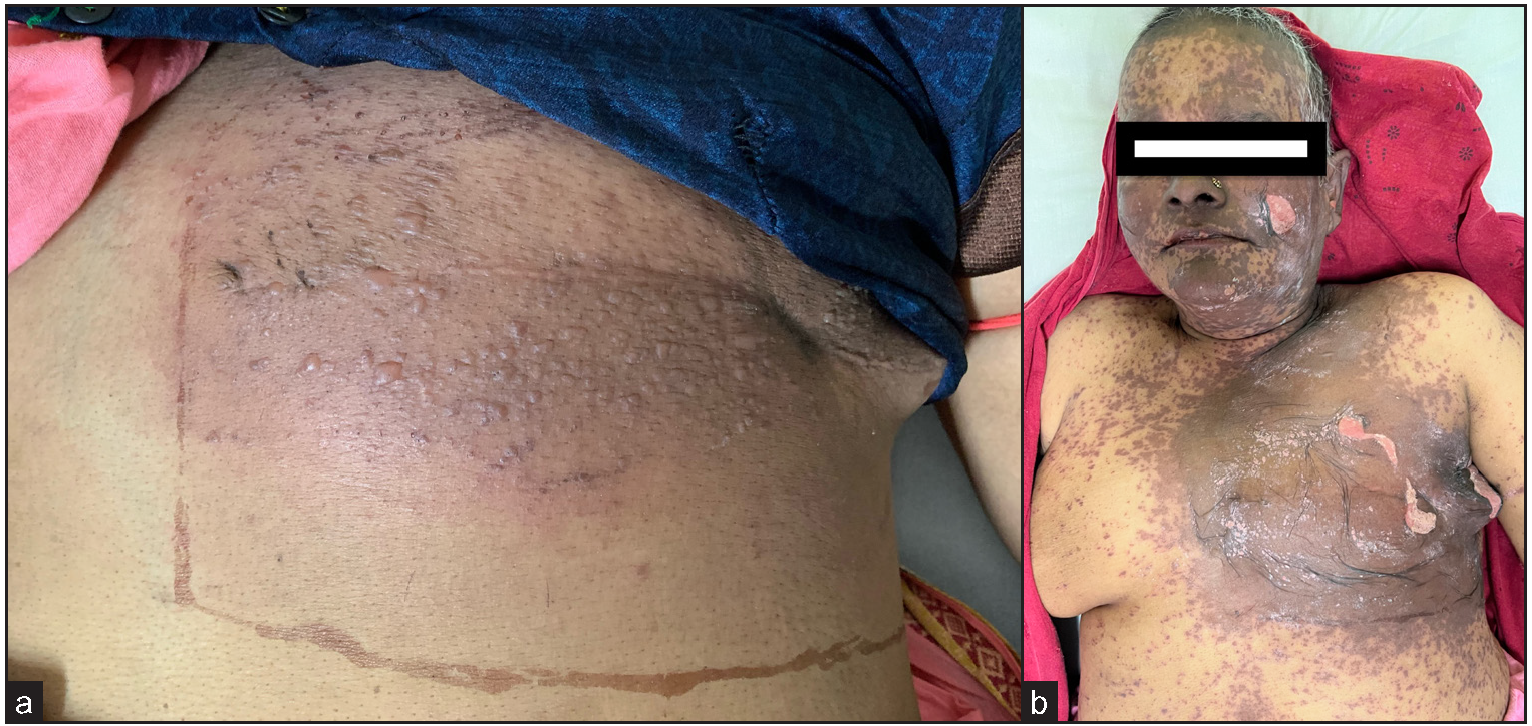
- (a) Multiple vesicles and bullae seen limited to the site of radiotherapy; (b) Extensive involvement of face and trunk in the form of purpuric macules and epidermal detachment localised to radiotherapy site.
A diagnosis of toxic epidermal necrolysis due to carbamazepine (Naranjo score-06) revealed approximately 30% body surface area involvement. Lab investigations, including herpes simplex viruses 1 & 2 IgM titres, were normal. Skin biopsy from chest revealed intense basal vacuolar degeneration leading to dermo-epidermal junction clefting and numerous necrotic keratinocytes. There was a perivascular superficial mononuclear infiltrate with eosinophils [Figures 2a and 2b]. Patient was managed by stopping carbamazepine, administering oral cyclosporine at the dose of 5 mg/kg body weight tapered over the next 2–3 weeks along with other supportive care in the form of diluted potassium permanganate compresses and 1% framycetin cream application and non-steroidal anti-inflammatory drugs for pain management. She showed remarkable improvement in the next 10 days with complete healing of the skin [Figure 3].
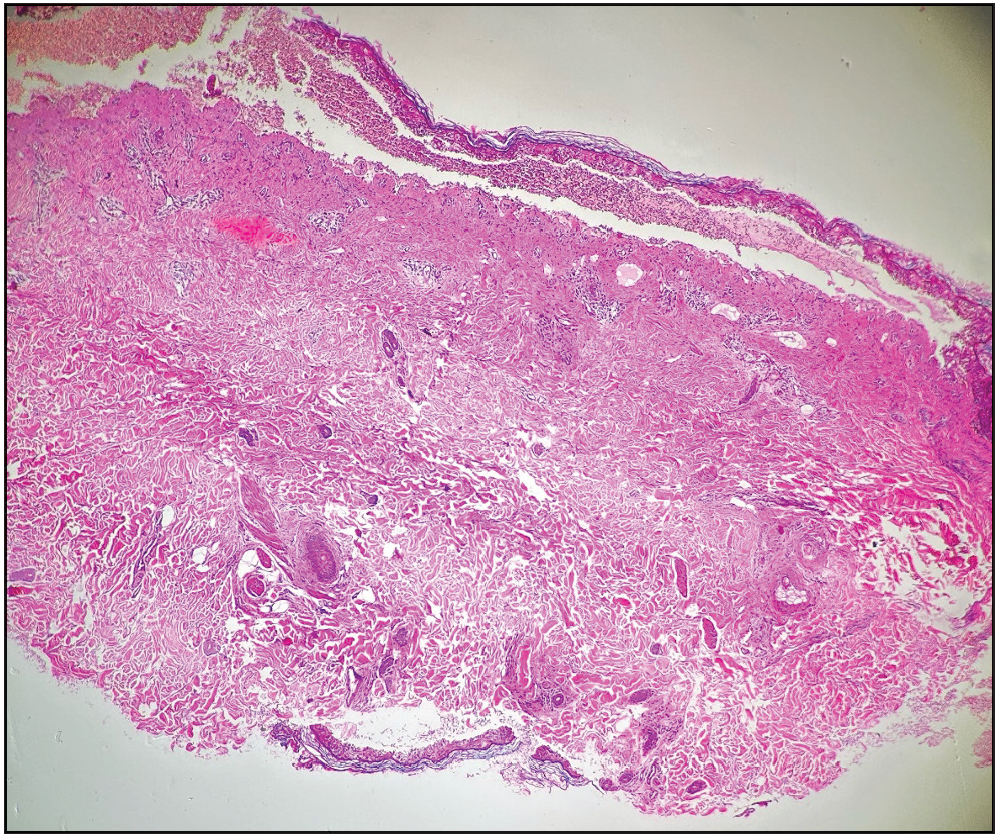
- Dermo-epidermal clefting associated with intense basal vacuolar degeneration (Haematoxylin & eosin, 100×).
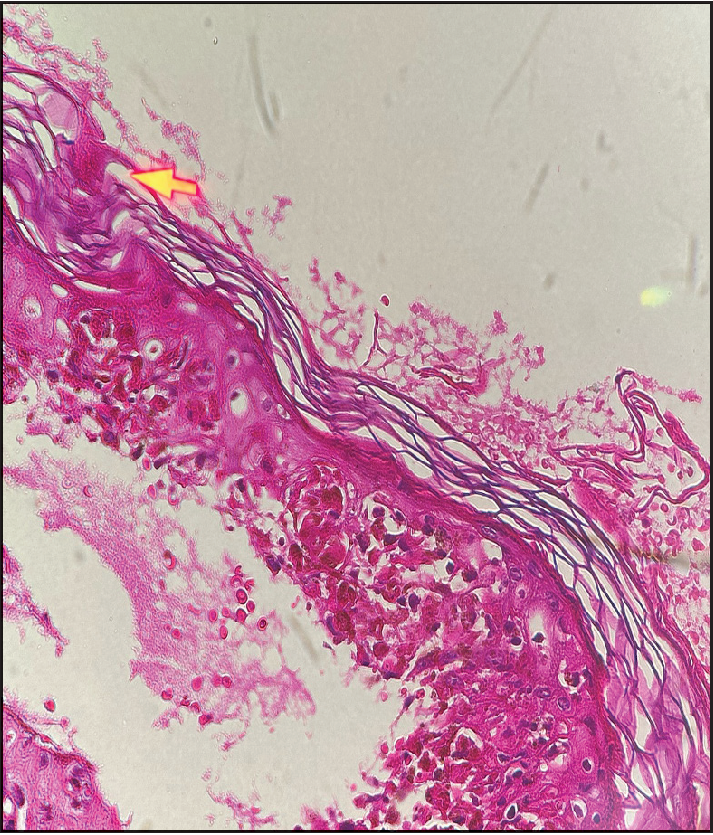
- Basal cell vacoular degeneration with numerous necrotic keratinocytes and a perivascular lymphocytic mononuclear infiltrate with eosinophils (Haematoxylin & eosin, 400×).

- Healing skin lesions one week after starting treatment.
Stevens–Johnson syndrome and toxic epidermal necrolysis are rare and severe mucocutaneous adverse reactions associated with high mortality rate ranging from 1 to 5% for Stevens–Johnson syndrome to 34 to 40% for toxic epidermal necrolysis.2 Multiple aetiologies, include drugs like antibiotics, anticonvulsants, analgesics, antineoplastic drugs, infectious agents and genetic predisposition; idiopathic causes account for 25% of cases.3 A few authors have pointed out the increased risk of Stevens–Johnson syndrome /toxic epidermal necrolysis with phenytoin and cranial radiation therapy, as described by EMPACT syndrome.4 Increased risk of toxic epidermal necrolysis is also there when radiotherapy is given concomitantly with 5-fluorouracil, carbamazepine and phenobarbitone.5
Lately the unique concept of immunocompromised district is used in dermatology to explain why a previously injured cutaneous site may become in time a privileged location for the outbreak of opportunistic infections, tumours and various immune reactions. Our case is one such example of this concept with localisation of skin lesions of toxic epidermal necrolysis predominantly to the irradiated site.
Anticonvulsants should be carefully chosen in patients with cancer who are receiving radiotherapy and patients should be closely monitored for the possibility of erythema multiforme, Stevens–Johnson syndrome or toxic epidermal necrolysis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Erythema multiforme, Stevens Johnson syndrome and toxic epidermal necrolysis syndrome in patients undergoing radiation therapy: a literature review. Am J Clin Oncol. 2014;37:506-13.
- [CrossRef] [PubMed] [Google Scholar]
- Stevens–Johnson syndrome/toxic epidermal necrolysis in a patient receiving concurrent radiation and gemcitabine. Anti-cancer drugs. 2003;14:659-62.
- [CrossRef] [PubMed] [Google Scholar]
- The current understanding of Stevens–Johnson syndrome and toxic epidermal necrolysis. Expert Rev Clin Immunol. 2011;6:803-15.
- [Google Scholar]
- Erythema multiforme associated with phenytoin and cranial radiation therapy: a report of three patients and review of the literature. Int J Dermatol. 2004;43:67-73.
- [CrossRef] [PubMed] [Google Scholar]
- Toxic epidermal necrolysis following phenytoin and cranial irradiation. Indian J Dermatol. 2015;60:424.
- [Google Scholar]
- Toxic epidermal necrolysis induced by phenytoin and whole brain radiotherapy. Actas Dermo-Sifiliográficas (English Edition). 2007;98:483-5.
- [PubMed] [Google Scholar]





