Translate this page into:
Tufted hair folliculitis with linear arrangement
Correspondence Address:
Lee Won-Soo
Department of Dermatology and Institute of Hair and Cosmetic Medicine, Yonsei University Wonju College of Medicine, 162 Ilsan-Dong, Wonju 220-701
Korea
| How to cite this article: Jae-Hong K, Hwa-Young P, Won-Soo L. Tufted hair folliculitis with linear arrangement. Indian J Dermatol Venereol Leprol 2011;77:535 |
Sir,
A 47-year-old woman presented with a 6-year history of tufted hairs that showed a linear arrangement on the scalp. She had suffered recurrent inflammation at the sites of hair tufting. Physical examination revealed a linear arrangement of skin lesion (1.5 × 10 cm) from the vertex area to the lower part of the occiput [Figure - 1]a. Within this area, we observed multiple hair tufts that were composed of multiple hairs emerging from single, dilated follicular ostia [Figure - 1]b. However, there were no definite hairless patches, which are a characteristic feature of cicatricial alopecia. The patient was otherwise healthy and had no family history of similar scalp disorder. Laboratory studies including complete blood cell count (CBC), blood chemistry, thyroid function test and urinalysis were within normal limits.
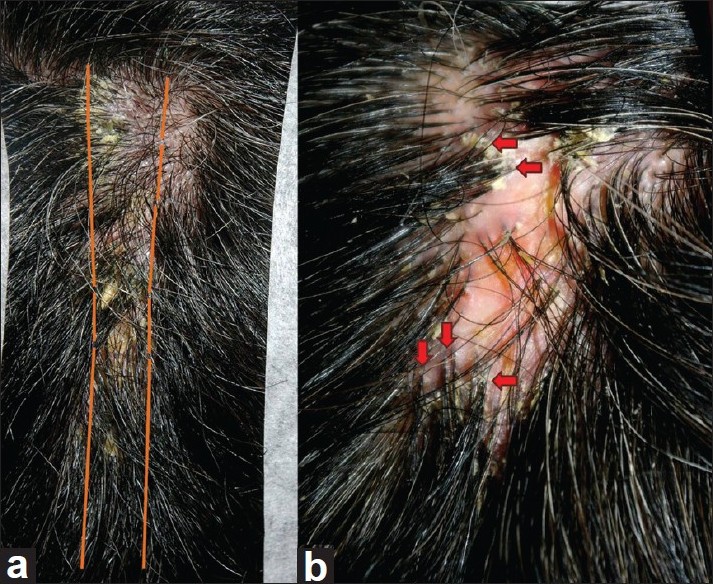 |
| Figure 1: (a) Linear arrangement of skin lesions from the vertex to the lower part of the occiput. (b) Within the affected area, hair tufts were composed of multiple hairs emerging from single, dilated follicular ostia (arrows indicate tufted hairs) |
Biopsy specimens were taken from the occipital skin lesion. Histopathologic examination revealed ruptured folliculitis with perifollicular infiltration of inflammatory cells. In addition, there were variable degrees of lymphohistiocytic cellular infiltrations with foreign body giant cell reactions on higher magnetic fields [Figure - 2].
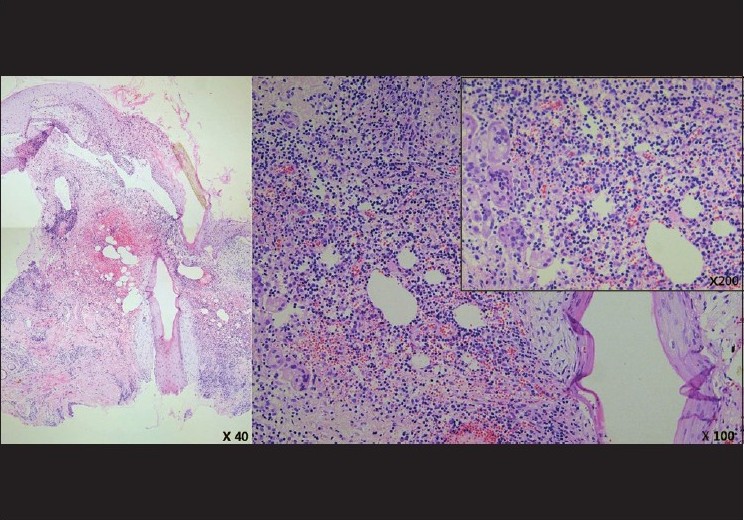 |
| Figure 2: Ruptured folliculitis with perifollicular infiltration of inflammatory cells (H and E, ×40). On higher magnification fields, variable degrees of lymphohistiocytic cellular infiltration with foreign body giant cell reactions are visible (H and E, ×100, ×200) |
On the basis of clinical and histopathologic findings, the patient was diagnosed with tufted hair folliculitis (THF). Oral administration of minocycline 100 mg/day and topical application of antibiotic ointment (fucidic acid) successfully suppressed the progression of hair tufting and perifollicular inflammation. After 1 year of treatment, the patient experienced neither signs of recurrences nor specific side effects related to the medication.
THF is a rare, recurrent, and progressive inflammatory condition of the scalp that is characterized by a peculiar tufting of hair. It may lead to the destruction of follicular units, resulting in permanent scarring alopecia. [1] Several cases have been reported since this disease entity was first described by Smith and Sanderson, [2] and it is still considered a rare dermatologic disorder. Variable factors such as primary hair tufting, local trauma, nevoid malformation and infection with Stapylococcus aureus have been proposed as causative pathomechanisms. [2],[3],[4],[5] However, the exact pathogenesis of THF is not fully understood because of the rare incidence of THF.
The identifying characteristic of this condition in our patient was linear hair tufting arranged from the vertex to the lower part of the occipital area. In contrast, most previously reported cases presented with patch or plaque patterns on the parietal or occipital area. The rare presentation that we observed is not only an interesting clinical pattern, but also a clue that may elucidate the pathomechanism of THF. In our case, there was no definite history of underlying disease or trauma to the scalp. However, secondary changes may have occurred following unrecognized trauma or repeated stimuli from a clinical presentational standpoint. This interpretation favors Pujol′s hypothesis that THF is a secondary phenomenon that occurs only after primary follicular damages. [5]
In conclusion, we report an interesting case of THF that demonstrated an atypical presentation with linear arrangement. Our report may assist in establishing characteristic clinical features of THF, and may be helpful for the further elucidation of the pathomechanism of THF.
| 1. |
Annessi G. Tufted folliculitis of the scalp: A distinctive clinicohistological variant of folliculitis decalvans. Br J Dermatol 1998;138:799-805.
[Google Scholar]
|
| 2. |
Smith NP, Sanderson KV. Tufted hair folliculitis of the scalp. J R Soc Med 1978;71:606-8.
[Google Scholar]
|
| 3. |
Tong AK, Baden HP. Tufted hair folliculitis. J Am Acad Dermatol 1989;21:1096-9.
[Google Scholar]
|
| 4. |
Dalziel KL, Telfer NR, Wilson CL, Dawber RP. Tufted folliculitis. A specific bacterial disease? Am J Dermatopathol 1990;12:37-41.
[Google Scholar]
|
| 5. |
Pujol RM, García-Patos V, Ravella-Mateu A, Casanova JM, de Moragas JM. Tufted hair folliculitis: A specific disease? Br J Dermatol 1994;130:259-60.
[Google Scholar]
|
Fulltext Views
4,569
PDF downloads
3,313





