Translate this page into:
Uncommon presentations of lupus miliaris disseminatus faciei
2 Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Dipankar De
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh
India
| How to cite this article: Vinay K, Mahajan R, Saikia UN, De D, Handa S. Uncommon presentations of lupus miliaris disseminatus faciei. Indian J Dermatol Venereol Leprol 2016;82:426-429 |
Sir,
Lupus miliaris disseminatus faciei is an uncommon granulomatous disorder predominantly involving the centro-facial area, including the region around the eyelids. It usually presents as multiple skin colored or yellowish brown papules and pustules, which heal to leave behind pock-like scars. Although extrafacial involvement and a nodular morphology of lesions have been reported, these are very uncommon.[1],[2],[3] Herein, we report four patients of lupus miliaris disseminatus faciei with simultaneous involvement of facial and extra-facial regions. Three of the patients also had prominent nodular and a few nodulo-cystic lesions. We were unable to find previous reports of this presentation.
A 32-year-old male patient presented with multiple, disfiguring “acne-like” lesions on the face, chest and upper back since 6 months. The lesions were asymptomatic but were gradually increasing in extent with appearance of new papules on face. During this time, none of the lesions showed spontaneous regression. On examination, multiple, brownish papular lesions with central scarring were noted on the forehead, cheeks and helix of the ears [Figure - 1]a. Lesions of similar morphology were also present on the chest and upper back. There were multiple, firm, freely mobile, nodulo-cystic lesions on the forehead [Figure - 1]a and [Figure - 1]b. Chest radiography was normal and Mantoux intradermal test was negative. A skin biopsy obtained from a papular lesion showed multiple epithelioid cell granulomas in the periappendageal dermis [Figure - 2]a and [Figure - 2]b. A slit-skin smear for lepra bacilli obtained from the papules was negative. Histopathological examination of a nodulo-cystic lesion showed a cyst wall made of fibro-collagenous tissue, devoid of lining epithelium (pseudo-cyst). Multiple compact epithelioid cell granulomas with giant cells were also noted in the cyst wall [Figure - 2]c and [Figure - 2]d. Based on these features, a clinical diagnosis of lupus miliaris disseminatus faciei was made and the patient was treated with oral minocycline, 100 mg twice daily. After 18 months of follow-up, there was complete resolution of nodulo-cystic lesions. Most of the papular lesions had healed with pock- like scars [Figure - 1]a and [Figure - 1]b.
 |
| Figure 1: Multiple brownish papules on the cheeks, forehead and concha with a prominent nodule on forehead (arrow) (a). Following treatment with oral minocycline, there was a complete healing of the lesions with pock like scars (b) |
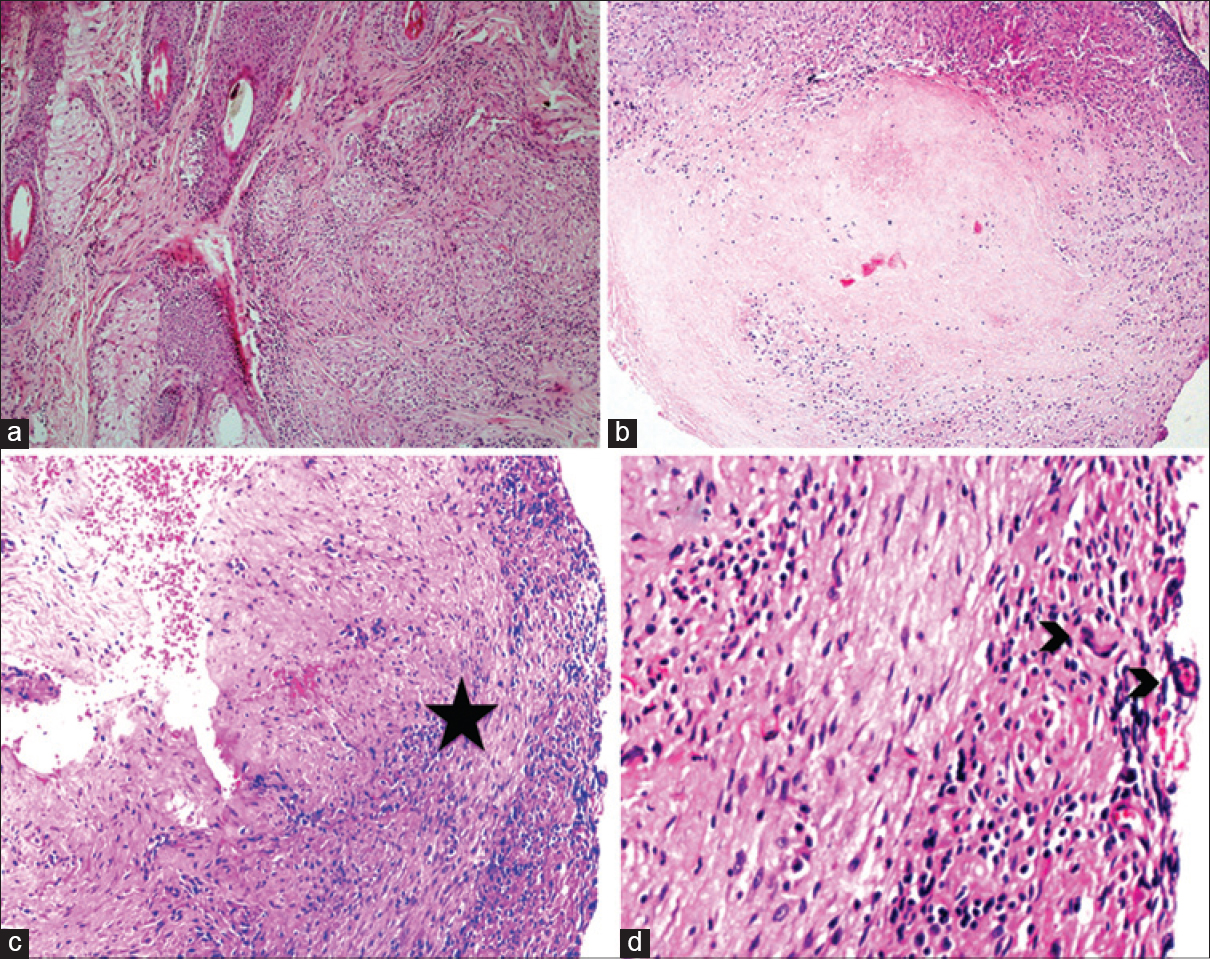 |
| Figure 2: Compact non-necrotizing granulomas around hair follicles (a) and large area of caseous necrosis bordered by epithelioid histiocytes, H and E, ×200 (b). Cystic lesion showing a fibrous capsule devoid of epithelium (star, H and E, ×200) (c). The cyst wall contains many epithelioid cells and giant cells (arrow, H and E ×400) (d) |
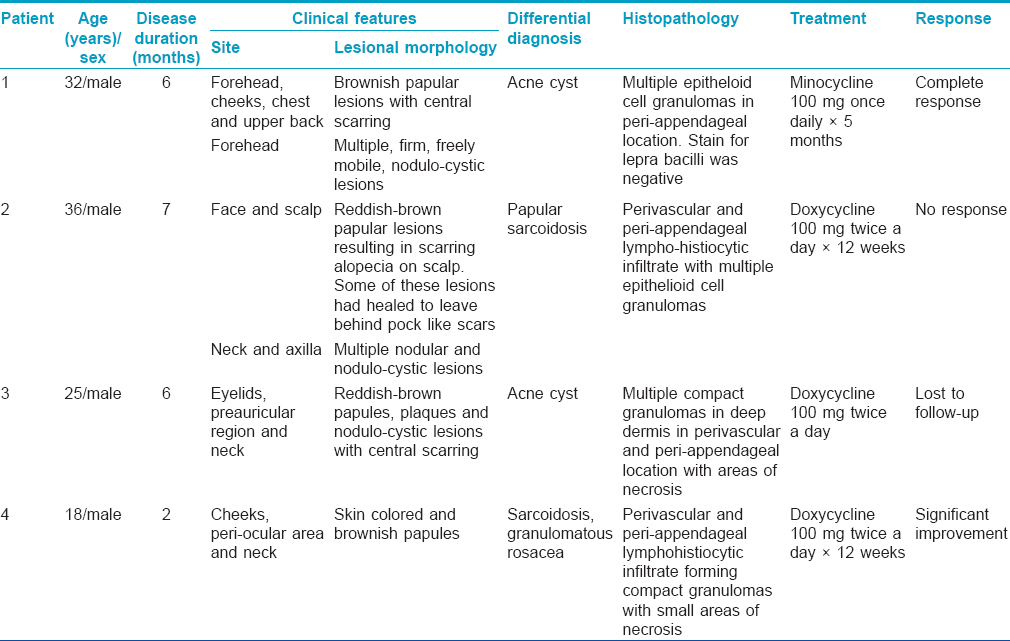
Following this, we came across three other patients of lupus miliaris disseminatus faciei with extra-facial lesions, two of them having prominent nodulo-cystic lesions (patients 2 and 3). Similar to our index case, all three patients had skin colored to reddish-brown papular lesions distributed predominantly on the centro-facial region. All of them had extra-facial lesions involving the neck and upper chest. Patient 2 also had involvement of axilla and scalp resulting in scarring alopecia [Figure - 3]a and [Figure - 3]b. Chest radiography was normal and Mantoux intradermal test was negative in all three cases. The salient investigations, histopathological findings and treatment response are summarized in [Table - 1].
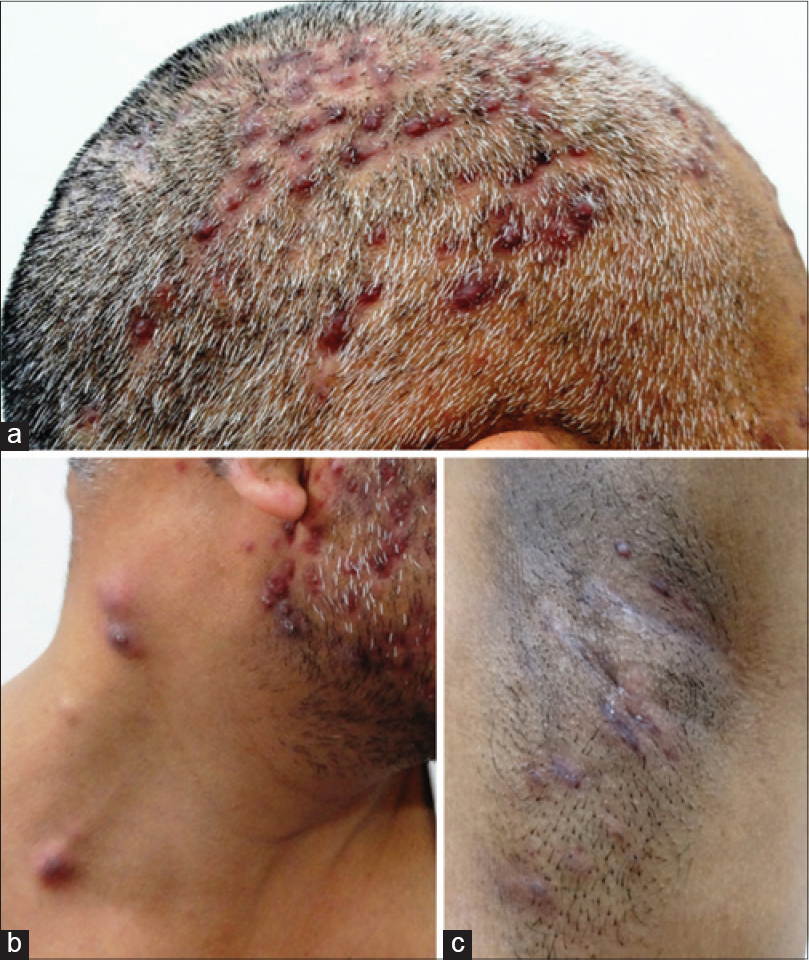 |
| Figure 3: Patient 2 showing reddish brown papular lesions over the scalp causing scarring alopecia (a) reddish brown papular lesions on the face and nodular lesions on the neck (b). Reddish brown papulo-nodular lesions involving the axilla (c) |
The nosological status of lupus miliaris disseminatus faciei has been a matter of debate ever since its first description. Radcliffe-Crocker initially coined the term 'acne agminata' to describe the condition although it bore only a remote resemblance to acne and the lesions were not always grouped.[4] The other names of this entity, that is, lupus disseminata and granulomatous rosacea have their detractors. More recently, a broad term “facial idiopathic granulomas with regressive evolution” (FIGURE) has been proposed, which would unify this entity along with other non-specific granulomatous disorders occurring on centro-facial area under a single name.[5]
Classically, the lesions in lupus miliaris disseminatus faciei are papular or pustular and are confined to the face. All four patients in the present series had lesions extending beyond the facial region. Another atypical feature seen in the patients was the presence of nodular and nodulo-cystic lesions. Nath et al. described a patient of lupus miliaris disseminatus faciei with reddish-brown papules and nodules on facial and extra-facial sites.[3] Their patient resembled our cases although the lesions were less inflammatory and not cystic. Such nodulo-cystic lesions need to be differentiated from epidermoid cysts and acne cysts. Sanz-Sánchez et al. reported a patient of lupus miliaris disseminatus faciei with co-existing epidermoid cyst and hypothesised that the rupture of the cysts may be related to the appearance of lupus miliaris disseminatus faciei.[6] Rupture of acne nodules and epidermoid cysts can incite a granulomatous response which can closely mimic lupus miliaris disseminatus faciei.[7] However, in such cases, the inflammation is generally suppurative, associated with rupture, distortion and destruction of appendages ultimately leading to scarring.[7] Caseous necrosis, typical of lupus miliaris disseminatus faciei is not seen in ruptured cysts.
Hillen et al. and Bedlow et al. have each reported a case of axillary acne agminata.[1],[2] Similar to our third patient, the case reported by Hillen et al.[1] also had classical lesions of lupus miliaris disseminatus faciei on the face. Interestingly, our patient additionally had scalp involvement resulting in scarring alopecia. We were able to find only one other such published report.[8]
Nodular lesions in lupus miliaris disseminatus faciei are under-recognized and/or under-reported.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hillen U, Schröter S, Denisjuk N, Jansen T, Grabbe S. Axillary acne agminata (lupus miliaris disseminatus faciei with axillary involvement). J Dtsch Dermatol Ges 2006;4:858-60.
[Google Scholar]
|
| 2. |
Bedlow AJ, Otter M, Marsden RA. Axillary acne agminata (lupus miliaris disseminatus faciei). Clin Exp Dermatol 1998;23:125-8.
[Google Scholar]
|
| 3. |
Nath AK, Sivaranjini R, Thappa DM, Basu D. Lupus miliaris disseminatus faciei with unusual distribution of lesions. Indian J Dermatol 2011;56:234-6.
[Google Scholar]
|
| 4. |
Radcliffe-Crocker H, editor. Diseases of the Skin. 3rd ed. London: Lewis; 1903.
[Google Scholar]
|
| 5. |
Skowron F, Causeret AS, Pabion C, Viallard AM, Balme B, Thomas L. F.I.GU.R.E.: facial idiopathic granulomas with regressive evolution. is 'lupus miliaris disseminatus faciei' still an acceptable diagnosis in the third millennium? Dermatology 2000;201:287-9.
[Google Scholar]
|
| 6. |
Sanz-Sanchez T, Dauden E, Moreno de Vega MJ, Fraga J, Garcia-Diez A. [Lupus miliaris disseminatus faciei associated with epidermal cysts]. Actas Dermosifiliogr 2005;96:320-2.
[Google Scholar]
|
| 7. |
Marks R, Dalziel K, Dykes PJ. Inflammation caused by intracutaneous implantation of stratum corneum. Br J Dermatol 1984;111 Suppl 27:109-13.
[Google Scholar]
|
| 8. |
Uchiyama M, Tsuboi R. Lupus miliaris disseminatus faciei involving the scalp resulted in cicatricial alopecia. J Dermatol 2013;40:760-1.
[Google Scholar]
|
Fulltext Views
6,092
PDF downloads
3,031





