Translate this page into:
Uses of hypodermic needle in dermatology
Correspondence Address:
Lakhan Singh Solanki
Department of Dermatology and Venereology, D-Block, 5th Floor, Government Medical College and Hospital, Sector-32, Chandigarh - 160 030
India
| How to cite this article: Solanki LS, Dhingra M, Thami GP. Uses of hypodermic needle in dermatology. Indian J Dermatol Venereol Leprol 2013;79:721-724 |
Introduction
A hypodermic needle is a simple hollow straight metallic instrument, however, its uses in dermatologic procedures are numerous and this article explains briefly its uses under following three broad headings namely-needle as a hook, needle as a cutting instrument and needle as an extractor.
Needle as a Hook
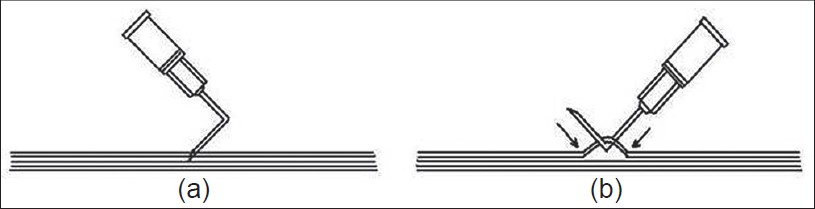
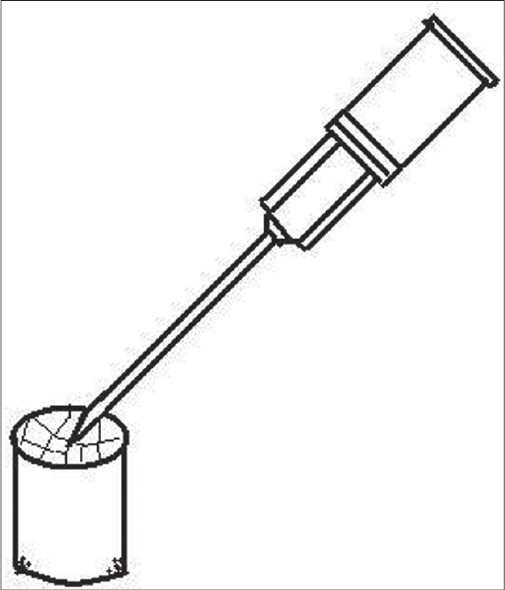
To use needle as a hook, it is bent in the middle at a right angle using an artery forceps, with cutting bevel tip preferably upward, to make it angulated [Figure - 1].
 |
| Figure 1: Photographs of hypodermic needle bent at right angle |
Nerve biopsy
After tissue dissection and adequate exposure of nerve, angulated needle can be used to pierce margin of nerve bundle so as to include only few fascicles. Using bent angle as a fulcrum, pull is applied to partially separate few fascicles from nerve bundle, which are then cut using surgical blade or scissors [Figure - 2].
 |
| Figure 2: (a and b) Nerve biopsy technique with a hypodermic needle |
Dog ear removal
Skin hook or forceps are used to hold the dog ear while excising it and followed by its repair using various techniques. [1],[2] Here, bent needle can be used as a hook to pull the redundant fold/dog ear while excising it with surgical knife [Figure - 3]. As hypodermic needle is being less traumatic to tissue and the same tissue can be used for grafting purpose.
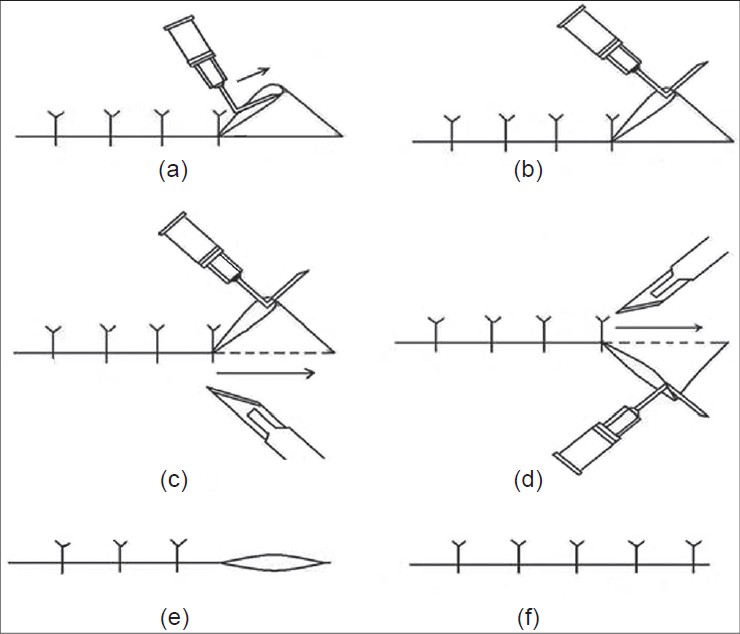 |
| Figure 3: (a-f) Steps for the removal of dog ear using a hypodermic needle |
Knot opening
To open an accidental knot in a fine suture, pointed end of a bent can be easily inserted in a small knot. Now holding the needle at the base using thumb and index finger of right hand and using its bent angle as a hook or fulcrum; it is slide gently to the free end of the suture. The other hand is used to tightly hold the suture at its needle end [Figure - 4].
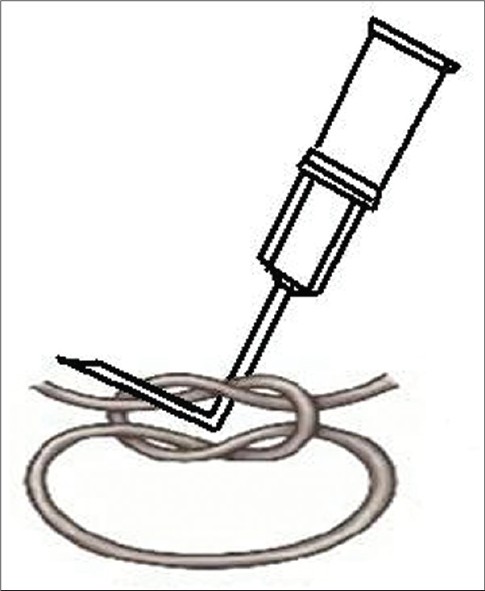 |
| Figure 4: Technique of knot removal by a hypodermic needle |
Suture cutting
To lift the suture away from skin surface, pointed end of bent hypodermic needle can be inserted below tied suture to hook it at its bent angle and then, cut using suture cutting scissors or surgical blade [Figure - 5].
 |
| Figure 5: Technique of suture lifting and cutting by a hypodermic needle |
Needle as a Cutting Instrument
Hypodermic needle can be used for various procedures as a cutting or stabbing instrument.
Drainage of paronychial abscess/small abscess
To drain proximal nail fold abscess in its natural anatomical plane, a 21 G needle with its bevel facing upwards is advanced parallel to the lateral groove along its base until its tip pierces the space below the junction of posterior and lateral nail folds. Same needle can be used to nick the lateral nail fold groove at its most fluctuant point or other small superficial abscesses. [3],[4]
Piercing
Ear piercing can be done using either standard technique (using only one 16 G needle) or simplified technique (using two needles of 21 G and 16 G) after giving local anesthesia. For nose piercing simple technique is advised, using 16 G needle. [5],[6],[7],[8]
Subcision
Subcision is also known as local undermining or subcutaneous incision-less surgery. It is a technique to uplift the scars by cutting the subcutaneous scar bands, especially, rolling type of acne scars. Once scar bands are broken a small hematoma forms below the scar, which leads to the elevation of the scar surface on reabsorption of hematoma. For depressed, bound down scars 18 G or 21 G needle, for fine wrinkles 24 G or 26 G and for deep wrinkles of forehead 16 G or 18 G are selected. For sweeping across large areas consisting of multiple, depressed scars, 16 G or 18 G needle can be used. [9],[10],[11],[12]
Drainage of pustular lesions in Acne
Papulopustular lesions can be incised by 21 G needle, and the contents of the lesion are then drained by exerting circumferential pressure around the pinched up lesion. [12],[13]
Hair transplantation
At the time of sleeving of grafts in hair transplantation, apex of one-half of donor strip is fixed either on wooden tongue spatula or wooden board with 26 G needle. Again during the placement of grafts (by stick and place method), recipient chambers (tunnels) are made all along the marked areas at a distance of 1.5 mm with 1.5 inch long beveled needle. For placing the grafts, 20/21 G is used for single hair grafts, 19 G needle is used for 2-3 hair grafts; and 18 G for 4, 5 or 6 hair grafts. [14]
Seroma/hematoma drainage in skin grafting
After opening the dressing of suction blister grafting or split thickness skin grafting after 24 h, seroma and hematoma if found can be drained by hypodermic needle followed by flushing with saline if required. This is done without removing the ointment impregnated mesh from the grafted area. [1]
Prick test
A small quantity of the test solution is placed on the skin and a prick is made through it with a sharp 22 G or 26 G needle. This should be superficial and not sufficient to draw blood. [15]
Modified prick test
Here, a drop of test solution is placed on the skin than a needle is then inserted very superficially and almost horizontally into the skin and lifted to raise a tiny tent of epidermis, rest is same as in prick test. [15]
Chemical cauterization of xanthelasma
Here, multiple superficial punctures are made over the surface of xanthelasma lesion with a 24 G or 26 G needle at multiple equidistant points so as to cover the area completely. The tip of sharp toothpick is then dipped in phenol and is reinserted through the earlier needle opening. This method of phenol application gives early and better results. [16]
Blister/Vesicle drainage
In bullous disorders like contact allergic and irritant dermatitis, Stevens-Johnson syndrome/Toxic epidermal necrolysis, and burn patients etc.
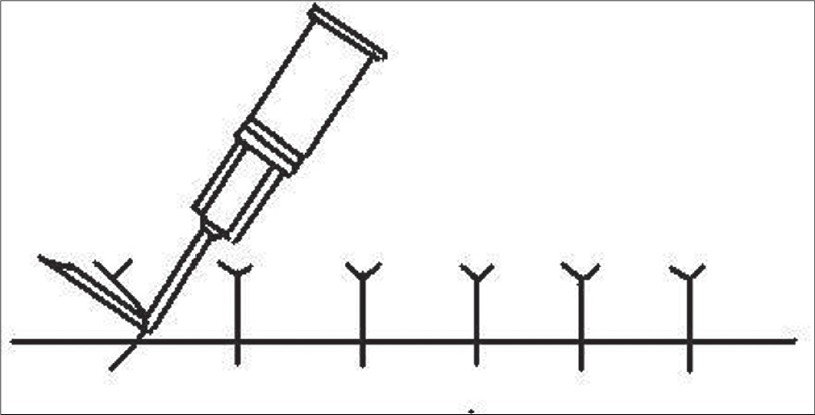
To transfer minigrafts in vitiligo surgery
In the technique suggested by Laxmisha et al., a 23 G hypodermic needle is used to transfer the graft from the saline soaked gauze to the recipient area. Here, the graft is secured by slightly piercing the mini-graft from epidermal side of the graft [Figure - 6]. This technique not only speeds up the procedure but also avoid trauma to the grafts. [17]
 |
| Figure 6: Technique to lift the graft by a hypodermic needle |
Pathergy test
Pathergy test is a common skin test to look for pathergy phenomenon. Based on the site over which it is performed, it is of following two types (1) Oral pathergy test: A prick is given on the mocosa of the lower lip with a 20 G blunt disposable needle. Test is positive if pustule or ulcer forms at the site of prick after 48 h. (2) Skin pathergy test: A prick is given on the hairless part of volar forearm with a 20 G blunt disposable needle. Needle is inserted vertically or at an angle of 45° to a depth of 3-5 mm. Test is positive if pustule or papule of size 1-5 mm forms at the site of prick after 48 h. The test is used as a diagnostic criterion in most diagnostic criteria for Behcet′s disease. Other conditions with positive pathergy phenomenon: Pyoderma gangrenosum, Sweet′s syndrome, eosinophilic pustular folliculitis, Inflammatory bowel syndrome, interferon alfa-treated chronic myeloid leukemia, and healthy individuals. [18]
Intralesional cryotherapy
Conventional surface cryosurgery is usually effective for smaller keloids but often results in pigmentary changes over the keloids. IL cryosurgery could be a preferred mode of therapy for large, bulky keloids, which are unresponsive to IL steroids. All it needs is a small liquid nitrogen Dewar cylinder, a rubber, and a plastic tube taken from a drip-set, adhesive tape, and hypodermic and lumbar puncture needles. The lumbar puncture or hypodermic needle introduced through the lesion until it appeared at the other side followed by passage of liquid nitrogen through the needle keeping freezing time between 20 s and 30 s. The procedure repeated for a second freeze-thaw cycle in the same session. Usually 5-10 sessions of IL cryosurgery are required to provide good results. [19]
Fine needle aspiration cytology
FNAC is safe, inexpensive, non-traumatic and a well-tolerated procedure. It can be used for the diagnosis of various skin conditions such as lipoma, neurofibroma, pilomatrixoma, histiocytoma, chondroid syringoma, neurilemmoma, myxoma, granular cell tumor. Among the malignant skin tumors, basal cell carcinoma, squamous cell carcinoma, melanoma, apocrine carcinoma, Merkel cell carcinoma, sebaceous carcinoma, and malignant cutaneous lymphoproliferative diseases can also be diagnosed by FNAC.
For exophytic lesions, it is performed using a 21-27 G needle and the needle should move gently in the lesion to avoid artifacts or hemorrhage in the tissues. For flat lesions and those suspicious of melanoma even insulin needles can be used to aspirate. [20] Withdrawal of the needle alone through the lesion can yield sufficient material for the establishment of the diagnosis.
Needle as an Extractor
Hypodermic needle can be used as an extractor in the treatment of milia, small retention cysts, comedones, molluscum contagiosum, small calcinosis cutis, senile comedones steatocystoma multiplex, and small foreign body.
Milia
The cutting tip of a 24 G or 25 G bent needle is used to make a superficial epidermal nick at the top of the lesion, thereafter, the angulated portion is used to apply a little pressure, in parallel fashion to the lesion to evacuate the contents. [21]
Comedones
For closed comedones, top of the comedone needs to be slited by a 25 G or 26 G needle, followed by evacuation of the contents in a manner similar to milia enucleation with a bent needle. For open comedones, only pressure with bent angle of the needle is required.
Molluscum contagiosum
Top of the lesion is silted in a manner similar to that of milia by a 25 G needle, followed by enucleation of molluscum body in a manner similar to milia enucleation with a bent needle.
Other Uses
Cotton tipped applicator
After applying small cotton at the tip of a hypodermic needle it can be used to apply Trichloroacetic acid, Phenol, podophylin, and tincture benzoin.
Sensory examination
This is to test pain sensation in leprosy and other cases of peripheral neuropathy.
| 1. |
Kirsner RS, Trent JT. Skin grafting. In: Nouri K, Leal-Khouri S, editors. Techniques in Dermatologic Surgery. 1 st ed. New York: Mosby; 2003. p. 153-62.
[Google Scholar]
|
| 2. |
Salasche SJ, Orengo IF, Siegle RJ, Zivony D. Grafts (M-plasty as Dog-Ear Repair). In: Salasche SJ, Orengo IF, Siegle RJ, editors. Dermatologic Surgery Tips and Techniques. 1 st ed. Newyork: Mosby; 2007. p. 98-9.
[Google Scholar]
|
| 3. |
Keyer JJ, Littler JW, Eaton RG. Surgical treatment of infections and lesions of the parionychium. Hand Clin 1990;6:137-53.
[Google Scholar]
|
| 4. |
Zook EG, Baran R, Haneke E, Dawber RP. Nail surgery and traumatic abnormalities. In: Baran R, Dawbwer RP, editors. Diseases of the Nails and Their Management. 3 rd ed. Oxford: Blackwell Science; 2001. p. 425-514.
[Google Scholar]
|
| 5. |
Bennett RG. Ear piercing. In: Bennett RG, editor. Fundamentals of Cutaneous Surgery. 1 st ed. St Louis: Mosby; 1988. p. 611-5.
[Google Scholar]
|
| 6. |
Duffy MM. A simple instrument for ear piercing. Plast Reconstr Surg 1967;40:92-3.
[Google Scholar]
|
| 7. |
Goldman L, Kitzmiller KW. Earlobe piercing with needles and wire. Arch Dermatol 1965;92:305-6.
[Google Scholar]
|
| 8. |
Watson MG, Campbell JB, Pahor AL. Complications of nose piercing. Br Med J (Clin Res Ed) 1987;294:1262.
[Google Scholar]
|
| 9. |
Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg 1995;21:543-9.
[Google Scholar]
|
| 10. |
Savant SS, Gore D. Acne Scar revision surgery. Ind J Dermato Surg 1999;1:11-22.
[Google Scholar]
|
| 11. |
Jacob CI, Daver JS, Kaminer MS. Acne scarring. A classification system and reviews of treatment options. J Am Acad Dermatol 2001;45:109-17.
[Google Scholar]
|
| 12. |
Savant SS. Surgery for active acne. In: Savant SS, editor. Text Book of Dermatosurgery and Cosmetology. 2 nd ed. India: ASCAD; 2005. p. 626-35.
[Google Scholar]
|
| 13. |
Shalita AR. Surgical methods for the treatment of acne vulgaris. J Dermatol Surg 1975;1:46-8.
[Google Scholar]
|
| 14. |
Savant SS. Hair restoration surgery. In: Savant SS, editor. In: Text Book of Dermatosurgery and Cosmetology. 2 nd ed. India: ASCAD; 2005. p. 254-74.
[Google Scholar]
|
| 15. |
Cox NH, Coulon IH. Diagnosis of skin disease. In: Burns T, Breathnach S, Cox N, Griffith C, editors. Rook's Textbook of Dermatolog. 7 th ed. Oxford: Blackwell Science; 2004. p. 5.1-5.20.
th ed. Oxford: Blackwell Science; 2004. p. 5.1-5.20.'>[Google Scholar]
|
| 16. |
Savant SS. Chemical cauterization. In: Savant SS, editors. Text Book of Dermatosurgery and Cosmetology. 2 nd ed. India: ASCAD; 2005. p. 107-16.
[Google Scholar]
|
| 17. |
Laxmisha C, Thappa DM. Surgical pearl: Use of hypodermic needle to transfer minigrafts. J Am Acad Dermatol 2006;54:707.
[Google Scholar]
|
| 18. |
Sequeira FF, Daryani D. The oral and skin pathergy test. Indian J Dermatol Venereol Leprol 2011;77:526-30.
[Google Scholar]
|
| 19. |
Gupta S, Kumar B. Intralesional cryosurgery using lumbar puncture and/or hypodermic needles for large, bulky, recalcitrant keloids. Int J Dermatol 2001;40:349-53.
[Google Scholar]
|
| 20. |
Zajdela A, Zillhard P, Voillemot N. Cytological diagnosis by fine needle sampling without aspiration. Cancer 1987;59:1201-5.
[Google Scholar]
|
| 21. |
Thami GP, Kaur S, Kanwar AJ. Surgical Pearl: Enucleation of milia with a disposable hypodermic needle. J Am Acad Dermatol 2002;47:602-3.
[Google Scholar]
|
Fulltext Views
15,597
PDF downloads
3,887





