Translate this page into:
Viva questions from the IJDVL
2 Department of Dermatology, K J Somaiya Medical College and Research Centre, Mumbai, Maharashtra, India
Correspondence Address:
Vishalakshi Viswanath
Department of Dermatology, Rajiv Gandhi Medical College, Thane, Maharashtra
India
| How to cite this article: Viswanath V, Vasani R. Viva questions from the IJDVL. Indian J Dermatol Venereol Leprol 2016;82:468-473 |
Focus Topic: Acquired Palmoplantar Keratoderma
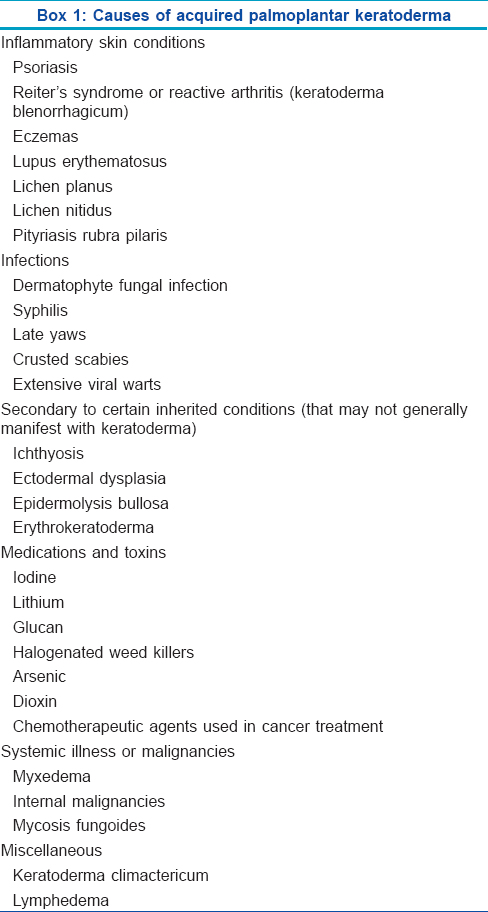
What are the causes of acquired palmoplantar keratoderma?
The causes of acquired palmoplantar keratoderma are outlined in [Box 1].
Discuss the likely diagnoses based on the clinical history and findings given below
A 56-year-old obese hypertensive woman presented with painful, hyperkeratotic, erythematous, fissured plaques on the ball of the foot and heel for one year with aggravation of the symptoms in winter. She also gave a history of similar lesions appearing on the center of the palm for the past 2 months. Rest of the cutaneous examination including the scalp and nails are normal. There are no associated systemic symptoms.
There are two possibilities that one can consider in this case of acquired palmoplantar keratoderma.
The first possibility is keratoderma climactericum (climacteric = menopause in females). It is seen in obese, postmenopausal females and presents with erythematous hyperkeratotic painful fissured plaques on the pressure-dependent areas that tend to become confluent with time with similar lesions appearing on the palms. These patients give a history of worsening in winter. Treatment consists of weight reduction, topical keratolytics, estradiol and oral retinoids.
The second possibility is palmoplantar psoriasis. It can occur in identical circumstances, but the absence of lesions elsewhere (other classical sites of psoriasis, nails, scalp and arthritis) makes it less likely. Diffuse gross and centripalmar hyperkeratotic plaques are seen. Scalloped margins (Festonne) and depressed plaques (Caro-Seaner) on the sides of the fingers and involvement of knuckles suggest the diagnosis. Different morphologies can be seen in palmoplantar psoriasis. There can be hyperkeratotic plaques (resembling chronic hyperkeratotic eczema), erythematous patches or plaques studded with minute superficial pustules and discrete scaly plaques or patches.
How does palmoplantar psoriasis differ from hyperkeratotic eczema?
Palmoplantar psoriasis is very difficult to differentiate from hyperkeratotic hand and foot eczema and they may at times alternate. A sharply defined edge at the wrist, forearm or palm; absence of vesiculation and dull red thickening of the skin on the knuckles are useful pointers toward a psoriatic etiology.
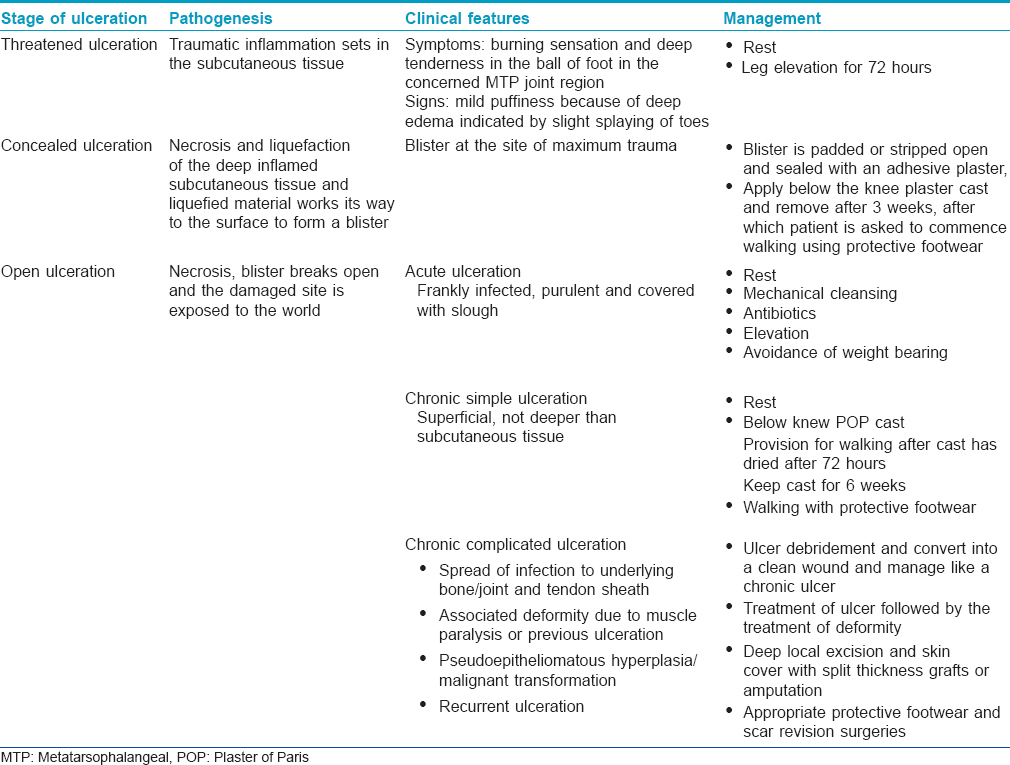
Crossword on acquired palmoplantar keratoderma
Use the clues provided in [Box 2] to complete the crossword on acquired palmoplantar keratoderma in [Figure - 1]. Answers are provided on page number.
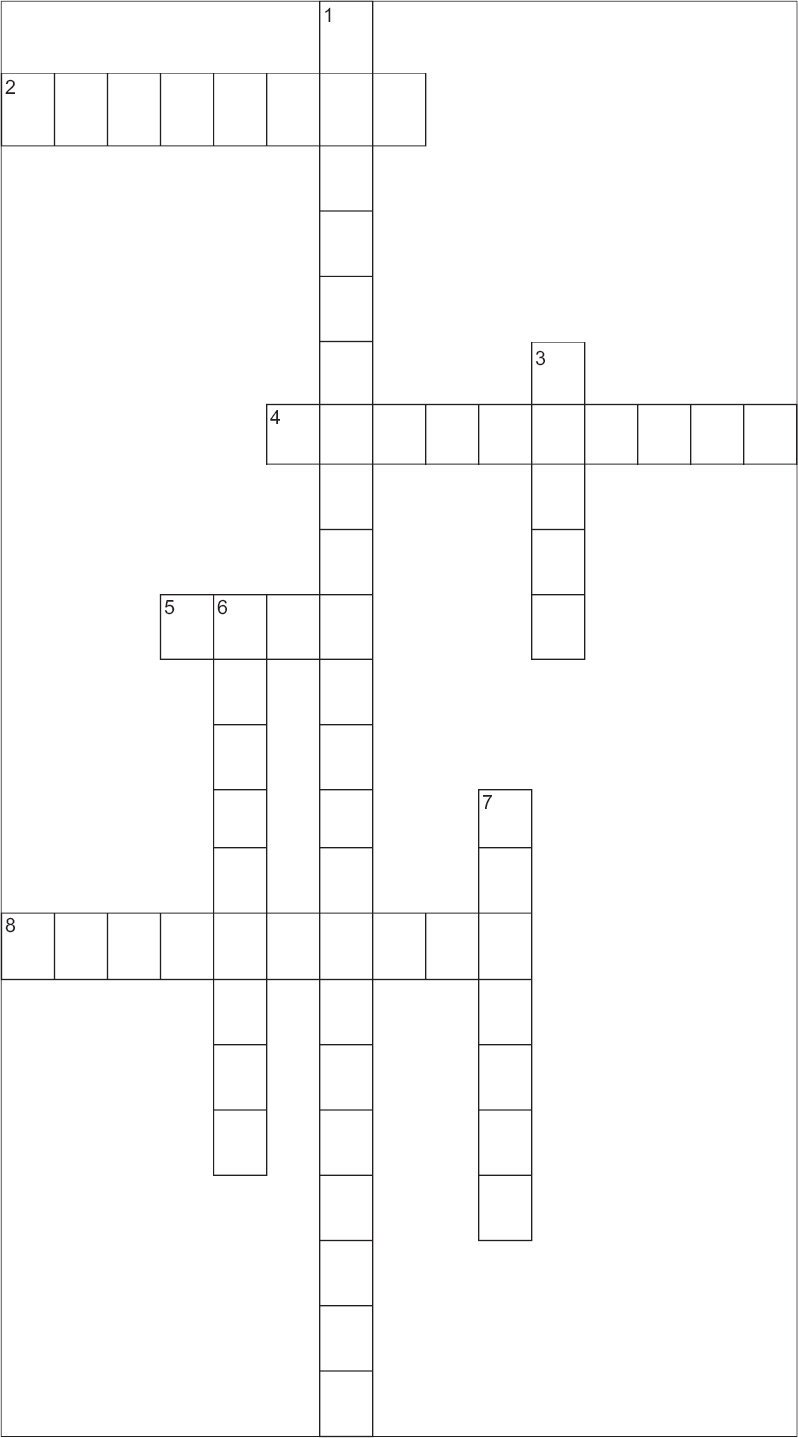 |
| Figure 1: Crossword on acquired palmoplantar keratoderma Answers are provided in [Figure - 2] on page 473. |
Trophic Ulcer
What are the most common sites of a trophic ulcer on the foot?
Trophic ulcers result due to an injury to an area which is compromised due to disease, vascular insufficiency or sensory loss. In leprosy, it can occur due to injury through a fissure in the skin or it commonly occurs due to the breakdown of tissue from within on account of intrinsic muscle paralysis. Hence, the front part of sole (ball of the foot) in the metatarso-phalangeal joint region is the most common site of ulceration in leprosy patients in 80% of the cases. The mid-lateral part of the sole underlying the region of the cubo-metatarsal joint and heel is the next common site comprising 5–10% of the cases.
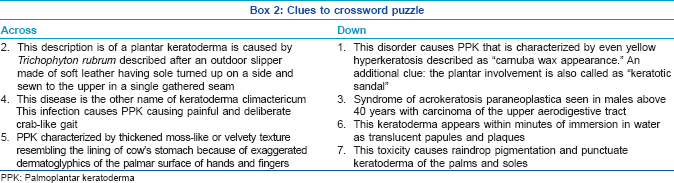
Describe the stages of trophic ulceration?
The various stages of trophic ulcer, pathogenesis, clinical features and management are outlined in [Table - 1].
What are the methods of prevention of trophic ulceration?
The methods for the prevention of trophic ulceration include education, self-care procedures and protective footwear.
- Education
- Self-care procedures:
- Inspection – To identify early signs of damage
- Soaking – In plain water for 20–30 min
- Scraping – Gentle scraping with a rough cloth, brush or a flat stone with a rough surface without sharp edges
- Oiling – To retain the water, apply a thin layer of mineral oil such as liquid paraffin, petroleum jelly or vegetable oil such as neem oil
- Dressing with clean and sterile materials
- Minimize walking: Define safe limits of walking.
- Safe protective footwear at all times, even inside the house.
Describe the type of footwear used in trophic ulceration
The footwear used by patients with trophic ulceration is designed to minimize further trauma and to decrease pressure at vulnerable sites. The structure of footwear with its relevant function is outlined in [Table - 2].
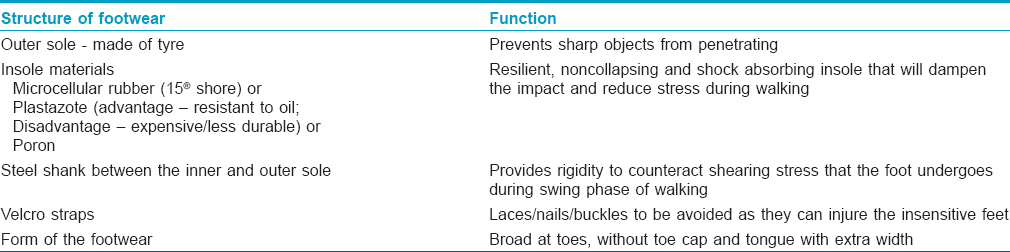
Modifications in footwear can be done based on patient needs.
- Additional metatarsal bar obliquely across the sole about 25 mm proximal to the metatarsal heads or inserting a medial arch support that reduces pressure considerably in patients with plantar scars
- Molded insoles help to decrease the higher pressure at vulnerable sites and in cases where even short distance walking causes the scars to breakdown, orthosis can be used with molded insoles.
What are the offloading measures in trophic ulceration?
Offloading pressure off the ulcer is the key to successful management of a trophic ulcer. Once the ulcer heals, in the early phase (6–8 weeks), it is still liable to breakdown, and more restrictive types of offloading devices need to be used before the patient can graduate to specialized footwear. The modalities of offloading include:
- Strict bed rest
- Use of crutches
- Wheel chairs
- Walkers
- Pressure-reducing measures such as air cushions and water beds
- Plaster boots (total contact casting) and removable contact casting
- Half shoes and specialized footwear.
Imatanib
Enumerate the Food and Drug Administration-approved uses of imatinib
Imatinib is a tyrosine kinase inhibitor that targets break cluster region-abelson tyrosine kinase, platelet-derived growth factor and v-kit Hardy-Zuckerman 4 feline sarcoma viral gene homolog (KIT).
The Food and Drug Administration approved uses include Philadelphia-chromosome-positive adult chronic myelogenous leukemia, KIT-positive metastatic gastrointestinal stromal tumor, acute myelogenous leukemia, myelodysplastic/myeloproliferative diseases, hypereosinophilic syndrome, aggressive mastocytosis, refractory dermatofibrosarcoma protuberans and metastatic malignant melanoma.
Enumerate the cutaneous side effects of imatinib
The most common toxicities with imatinib are nausea, myalgia, skin rashes and edema.
Among the dermatological side effects, maculopapular rash is the most common. Other side effects include xerosis, photosensitivity, angular cheilitis, psoriasiform rash and pigmentary changes. Rarer side effects include acute generalized exanthematous pustulosis, urticaria, lichenoid reaction and painful oral erosions.
Pigmentary changes are common and usually manifest as hypopigmentation; however, hyperpigmentation may also be seen. Hypopigmentation may manifest as generalized skin lightening, vitiligo-like lesions and hair graying; it is common since the drug inhibits melanogenesis via inhibition of the binding of ligands to c-kit receptors. Hyperpigmentation is uncommon and may be seen on the skin, palatal mucosa, nails, teeth, hair and gums. Melasma-like pigmentation has also been recently described. Hyperpigmentation is attributed to the formation of a drug-melanin metabolite; other theories include drug-induced cytotoxic response to epidermal “neoantigen” and the presence of a specific KIT mutation and its interaction with other receptors.
Epidermodysplasia Verruciformis
What is epidermodysplasia verruciformis?
Epidermodysplasia verruciformis is a rare genodermatosis with an increased susceptibility to infection by specific strains of human papilloma virus (subtypes 5 and 8). It is an autosomal recessive disorder due to mutations in the epidermodysplasia verruciformis 1 and epidermodysplasia verruciformis 2 genes located on chromosome 17q25. It was first described by Lewandowsky and Lutz in 1922.
What are the clinical features of epidermodysplasia verruciformis?
The disease manifests as two main phenotypes which differ with respect to the potential for malignant transformation. The benign lesions manifest as flat, wart-like, hypopigmented or hyperpigmented papules that may coalesce to form scaly patches or plaques with irregular borders resembling tinea versicolor. These lesions are most prevalent on the trunk, neck and extremities. The lesions with malignant potential manifest as verrucous and seborrheic keratosis-like lesions and occur more frequently on photo-exposed sites including face, hands and feet.
Enumerate the treatment options and malignancies associated with epidermodysplasia verruciformis
Photoprotection should be strictly advised and patients should be kept under observation for the development of premalignant and malignant tumors. Treatment options include systemic retinoids, interferons, cimetidine and topical imiquimod, immunotherapy and vitamin D analogs.
About 30–60% of the patients develop skin malignancies, mostly in the fourth and fifth decades. The common malignancies are squamous cell carcinoma and Bowen's disease. Adnexal carcinoma is uncommonly reported.
Itolizumab
What is the mechanism of the action of itolizumab?
Itolizumab is a novel humanized monoclonal antibody developed in India for moderate/severe chronic plaque psoriasis. It inhibits T-cell proliferation induced by activated leukocyte cell adhesion molecules and interleukin-2 by binding to the extracellular scavenger receptor cysteine-rich distal domain 1 of CD6. It downregulates the phosphorylation of intracellular proteins and also reduces the production of interferon-γ, interleukin-6 and tumor necrosis factor-α.
What is the dosage regimen for itolizumab in psoriasis?
Itolizumab is administered as an intravenous infusion at a dose of 1.6 mg/kg in 250 ml of normal saline over 3 h. The recommended dosage for psoriasis is 1.6 mg/kg body weight, once every 2 weeks for 12 weeks and 1.6 mg/kg once in 4 weeks until 24 weeks have elapsed.
Why are infections less commonly encountered with itolizumab in comparison to other biologicals?
Itolizumab binds to CD6, a highly glycosylated membrane protein predominantly expressed on lymphocytes. The CD6 co-stimulatory pathway contributes to Th1 activation and differentiation of T-cells, promoting a pro-inflammatory response. The immunomodulatory effects are thus not produced by inhibiting ligand binding and inducing T-cell depletion. They are effected by turning receptor binding nonproductive, either by inhibiting new receptor formation or by stimulating the loss of existing receptors or by causing a blockage followed by internalization or downregulation of receptors. Hence, no significant alteration of the lymphocyte count or signs of immunosuppression is documented at any dose of itolizumab monotherapy. Thus, the infection rates with itolizumab (18%) are lowest in phase III trials in comparison to other biologicals (ustekinumab, 22–31%; etanercept, 27%, adalimumab, 29% and infliximab, 42%).
Lymphatic Filariasis
Which are the important species and the commonly affected geographic areas for lymphatic filariasis?
Wuchereria bancrofti, Brugia malayi, Onchocerca volvulus and Loa loa are the important filarial species responsible for lymphatic filariasis.
Lymphatic filariasis is endemic worldwide and nearly 1.4 billion people are estimated to be at risk globally. Asia, Africa, Pacific Islands, South America and the Caribbean basin are the most affected geographic areas. In India, the endemic states are Bihar with the highest endemicity (over 17%), Kerala (15.7%) and Uttar Pradesh (14.6%).
What are the clinical manifestations of lymphatic filariasis?
Lymphatic filariasis can have varied clinical manifestations: acute lymphadenitis, acute lymphangitis, asymptomatic subcutaneous swelling, funiculo-epididymoorchitis, chronic lymphedema, hydrocele, lymph node swellings, nodules in breast, thyroid or salivary gland, tropical pulmonary eosinophilia and chyluria. Recurrent episodes of lymphangitis predispose to chronic lymphedema and increased bacterial and fungal infections. Gradually, patients develop deformities and the quality of life is affected.
Which are the non-invasive techniques of diagnosing lymphatic filariasis?
Non-invasive methods for the diagnosis of lymphatic filariasis include the following:
Imaging techniques (ultrasonography and magnetic resonance imaging) demonstrate the continuous twirling motion of echogenic particles representing either adult filarial worms or microfilaria in scrotal lymphatics (filarial dance sign). Lymphoscintigraphy aids in the demonstration of anatomical and functional abnormalities in lymphatic channels using radiolabeled dextran.
Demonstration of microfilariae is possible in blood smears or from fine-needle aspiration cytology smears. Peripheral venous blood smears sampled at midnight or after diethylcarbamazine provocation during the day can show microfilariae. Fine-needle aspiration cytology offers an easy, inexpensive and quick method to demonstrate microfilariae and adult worms; however, it has a low detection rate.
Species identification can be done by the use of immunochromatographic and deoxyribonucleic acid probes using polymerase chain reaction.
What are the treatment modalities for lymphatic filariasis?
Treatment modalities include diethylcarbamazine at 6 mg/kg single dose or daily for 12 days in divided doses, oral ivermectin 200 μg/kg and albendazole 400 mg twice daily for 2 weeks. In endemic countries, mass administration of a single annual dose of oral albendazole 400 mg and diethylcarbamazine 6 mg/kg of body weight is recommended for the prevention of transmission.
The management of chronic lymphedema includes limb elevation, local care, regular exercise, massage, intermittent pneumatic compression of the affected part and surgical procedures such as lymph node venous shunt, omentoplaxy, excisional surgery and skin grafting.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Fulltext Views
9,590
PDF downloads
3,415





