Translate this page into:
Evaluation of nail fold capillaroscopy changes in patients with diabetic retinopathy and healthy controls, and its correlation with disease duration, HbA1c levels and severity of diabetic retinopathy: An observational study
Corresponding author: Dr. Tejinder Kaur, Department of Dermatology, Venereology and Leprosy, Government Medical College, Amritsar, India. tejinderkaurdr@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahajan M, Kaur T, Singh K, Mahajan BB. Evaluation of nail fold capillaroscopy changes in patients with diabetic retinopathy and healthy controls, and its correlation with disease duration, HbA1c levels and severity of diabetic retinopathy: An observational study. Indian J Dermatol Venereol Leprol. 2024;90:782-8. doi: 10.25259/IJDVL_232_2023
Abstract
Background
Diabetic retinopathy (DR) is an important microvascular complication of long-term type 2 diabetes mellitus (T2DM) leading to blindness if not properly diagnosed and managed. It can develop as early as 7 years before the diagnosis of diabetes. Nail fold capillaroscopy (NFC) is a non-invasive technique for observing capillary microvasculature and there are few studies which have explored the use of NFC in diabetes mellitus patients.
Objective
To study the nail fold capillaroscopic alterations in patients with T2DM having diabetic retinopathy and compare them to healthy controls. The secondary objective was to correlate the NFC findings with the duration of diabetes, haemoglobin A1c (HbA1c) levels and the severity of DR.
Materials and methods
This cross-sectional observational study enrolled 200 patients - 100 cases with T2DM having diabetic retinopathy (as per the American Diabetes Association criteria and Diabetic Retinopathy Disease Severity Scale) and 100 healthy age and sex-matched controls. All patients were subjected to NFC and ophthalmological assessment.
Results
NFC revealed that patients with DR showed significantly higher frequencies of tortuous, dilated, bushy, meandering, angulated capillaries, avascular areas and micro-haemorrhages as compared to healthy controls (p < 0.05). In proliferative DR (PDR), the frequency of tortuous, bushy capillaries, and avascular areas was statistically high and the capillary density was reduced as compared to non-proliferative DR. The DR patients with longer disease duration (>20) years had a significantly higher frequency of tortuous capillaries, avascular areas, meandering, angulated and dilated capillaries. The frequency of tortuosity, avascular areas, and bushy areas was significantly higher in patients with poor glycaemic control (HbA1c >11).
Limitations
A larger sample size study with different demographic populations could have provided a broader picture of NFC changes in T2DM patients with DR.
Discussion
NFC may act as a surrogate marker of retinal involvement in patients with DM and should be performed at regular intervals.
Conclusion
NFC is a quick, simple, safe, and non-invasive method to assess the capillaroscopic alterations in diabetic patients which inturn can help in assessing the severity of DR.
Keywords
Nail fold capillaroscopy
Proliferative diabetic retinopathy
Non-proliferative diabetic retinopathy
Type 2 diabetes mellitus
HbA1c levels
Introduction
Nail fold capillaroscopy (NFC) is a simple, non-invasive, painless in vivo technique to assess microvasculature. It is an established method to assess microcirculation in connective tissue diseases (CTDs) and helps in the early diagnosis and monitoring of Systemic sclerosis (SSc). The proximal nail fold, being an acral area, is affected early by disorders that affect microvasculature and has the advantage of easy accessibility for repeated examination.1 Diabetic retinopathy (DR) is the most common microvascular complication of diabetes and remains a major cause of preventable blindness.2 As compared to studies evaluating the retinal microvascular changes in diabetics, very little is known regarding the NFC features of these patients.3 The objectives of the present study were to assess the nail fold capillaries in diabetic retinopathy to evaluate the micro-vascular involvement, to identify if there is any correlation between nail fold capillaroscopic findings and the severity of DR and determine whether NFC changes have a relationship with the duration of diabetes and glycaemic index.
Materials and Methods
This cross-sectional observational study enrolled 200 patients that included 100 cases of DR and 100 healthy age and sex-matched controls and was conducted in the Department of Dermatology and Ophthalmology of a tertiary care institute over 1.5 years. Sample size calculation was done using convenience sampling. The Institutional Ethical Committee approved the study protocol (IEC No-3385/D-26/2020 Batch). Adults (>18 years) diagnosed with T2DM, based on the American Diabetes Association criteria (ADA)4 and DR as per Diabetic Retinopathy Disease Severity Scale5 and consenting to the study protocol, were included. Patients who did not give consent, those with type 1 diabetes mellitus, nail unit infections, trauma, patients with known CTD or on drugs affecting peripheral circulation, patients with aesthetic treatments in the last two weeks before the study, and pregnant and lactating females were excluded. Informed written consent was taken from all the patients, before their inclusion in the study [Figure 1].
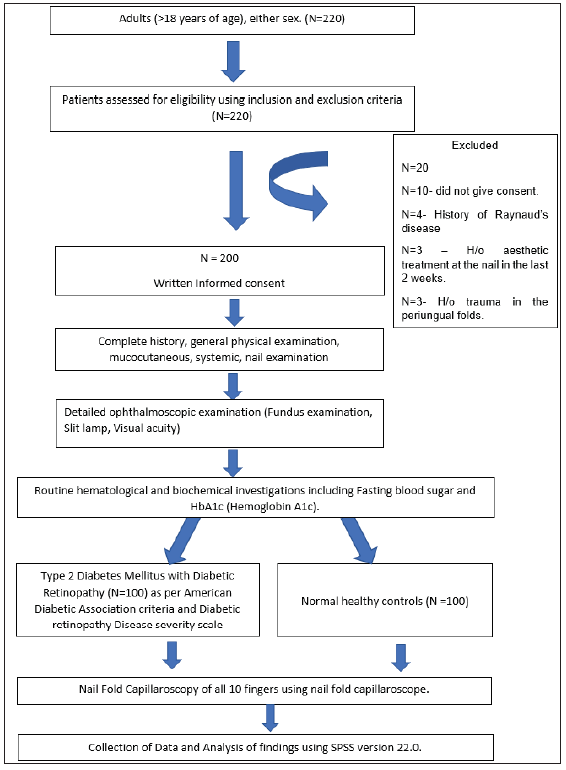
- The protocol of the study conducted.
A detailed NFC examination was done for all 10 fingernails, using a dermatoscope (AM 7515MZT Dino-Lite Edge Dermatoscope with 20x–220x magnification). The patients were made to sit for 15–20 min at an ambient temperature (around 20–22°C), with their hands at the level of the heart. Before the procedure nail plate and folds were cleaned with spirit and ultrasound gel was applied to the PNF to improve capillary visibility. NFC was performed, first at a low magnification for global visualisation of capillaries in the entire PNF and then at a higher magnification to assess individual capillary architectural change. Later the NFC changes were evaluated by the supervisor and recorded.
Qualitative morphological alterations in the capillary loops were visualised in all the fingers. The presence of dilated and giant capillaries (width of the capillary >2 times or >10 times the normal respectively); tortuous (capillary limb curled but not crossing over), neo-angiogenesis/bushy capillaries (small, multiple buds originating from the distal loop); meandering (limbs crossed upon themselves several times); micro-haemorrhages, capillary dropouts; avascular areas (absence of two or more adjacent capillaries from the distal-most row); and bizarre capillaries (atypical morphology not conforming to the predefined morphologies) were recorded.6,7 Receding capillaries were seen as individual capillaries maintaining their position in the distal-most row but present slightly proximal to the distal-most loops. They represent that the capillary had receded backwards but had not dropped out yet. A special type of tortuous capillary reported was angulated capillary where one or both the arms of the distal capillary loop were seen to bend at an angle.3 The visibility of the subpapillary plexus was also recorded [Figures 2–8].
![Nail fold capillaroscopy showing normal capillaries and dilated capillaries. (black arrow). [195.1 X] (DL0 – first dermoscopic calibration, DL1 – second dermoscopic calibration, H – represents the line used during the calibration.)](/content/126/2024/90/6/img/IJDVL-90-6-782-g2.png)
- Nail fold capillaroscopy showing normal capillaries and dilated capillaries. (black arrow). [195.1 X] (DL0 – first dermoscopic calibration, DL1 – second dermoscopic calibration, H – represents the line used during the calibration.)
![Nail fold capillaroscopy showing bushy capillaries and tortuous capillaries. (black arrow). [203.1x]](/content/126/2024/90/6/img/IJDVL-90-6-782-g3.png)
- Nail fold capillaroscopy showing bushy capillaries and tortuous capillaries. (black arrow). [203.1x]
![Nail fold capillaroscopy showing cross-linked (black arrow, blue circle), meandering capillaries (black arrow, blue circle) and avascular areas (blue arrow). [203.6 X]](/content/126/2024/90/6/img/IJDVL-90-6-782-g4.png)
- Nail fold capillaroscopy showing cross-linked (black arrow, blue circle), meandering capillaries (black arrow, blue circle) and avascular areas (blue arrow). [203.6 X]
![Nail fold capillaroscopy showing dilated and giant (black arrow) capillaries. [71.4x]. DL0: first dermoscopic calibration, DL1: second dermoscopic calibration, DL2: third dermoscopic calibration, H (red lines) signify the line used during calibration.](/content/126/2024/90/6/img/IJDVL-90-6-782-g5.png)
- Nail fold capillaroscopy showing dilated and giant (black arrow) capillaries. [71.4x]. DL0: first dermoscopic calibration, DL1: second dermoscopic calibration, DL2: third dermoscopic calibration, H (red lines) signify the line used during calibration.
![Nail fold capillaroscopy showing angulated capillaries (blue arrow). [149.8x]](/content/126/2024/90/6/img/IJDVL-90-6-782-g6.png)
- Nail fold capillaroscopy showing angulated capillaries (blue arrow). [149.8x]
![Nail fold capillaroscopy showing reduced capillary density and bushy capillaries (red arrow). [155.5x]. DL0: dermoscopic calibration used. H (red line) signify the line used during calibration.](/content/126/2024/90/6/img/IJDVL-90-6-782-g7.png)
- Nail fold capillaroscopy showing reduced capillary density and bushy capillaries (red arrow). [155.5x]. DL0: dermoscopic calibration used. H (red line) signify the line used during calibration.
![Nail fold capillaroscopy showing reduced capillary density, microhaemorrhages (green arrow) and avascular areas (blue arrow). [155.5x]. DL0: dermoscopic calibration used. H (red line) signify the line used during calibration.](/content/126/2024/90/6/img/IJDVL-90-6-782-g8.png)
- Nail fold capillaroscopy showing reduced capillary density, microhaemorrhages (green arrow) and avascular areas (blue arrow). [155.5x]. DL0: dermoscopic calibration used. H (red line) signify the line used during calibration.
Results were tabulated and analysed objectively at the end of the study statistically. Categorical variables were presented in number and percentage, and continuous variables were presented as mean ± SD. Quantitative variables were compared using an unpaired t-test between two groups. Qualitative variables were correlated using the Chi-square test. A ‘p’ value of <0.05 was considered statistically significant. The data were analysed using Statistical Package for Social Sciences (SPSS) version 22.0.
Results
A total of 100 patients with diabetic retinopathy and 100 healthy controls were evaluated and the baseline characteristics are summarised in Table 1.
| Baseline characteristics | Cases -Diabetic Retinopathy (n = 100), n (%) | Healthy controls (n = 100), n (%) | p-value |
|---|---|---|---|
| Mean age ±SD (years) | 58.32 ± 9.00 | 56.43 ± 7.62 | 0.926 |
| Male: Female ratio | 48:52 | 59:41 | 0.156 |
| Mean disease duration ±SD (years) | 12.24 ± 5.121 | - | |
| PDR | 14.52 ± 4.229 | - | |
| Severe NPDR | 11.92 ± 3.752 | - | |
| Moderate NPDR | 9.75 ± 5.149 | - | |
| Mild NPDR | 6.20 ± 4.658 | - | |
| BMI | 25.86 ± 3.77 | 23.97 ± 3.50 | |
| Mean fasting blood sugar ±SD (mg/dl) | 177.01 ± 48.40 | 94.91 ± 3.75 | |
| Mean HbA1c±SD (%) | 8.80 ± 1.60 | 5.43 ± 0.21 | |
| NFC parameters | |||
| Presence of dilated capillaries | 55 (55%) | 6 (6%) | 0.001* |
| Evidence of capillary dropouts | 4 (4%) | 7 (7%) | 0.352 |
| Presence of avascular areas | 71 (71%) | 3 (3%) | 0.001* |
| Presence of micro-haemorrhages | 27 (27%) | 5 (5%) | 0.001* |
| Bushy capillaries | 42 (42%) | 3 (3%) | 0.001* |
| Meandering capillaries | 33 (33%) | 7 (7%) | 0.001* |
| Tortuosity (>5% of capillaries) | 82 (82%) | 19 (19%) | 0.001* |
| Reduced capillary density | 61 (61%) | 9 (9%) | 0.001* |
| Subpapillary plexus visibility | 10 (10%) | 4 (4%) | 0.096 |
| Receding capillaries | 19 (19%) | 7 (7%) | 0.012* |
| Angulated capillaries | 31 (31%) | 0 | 0.001* |
| Normal capillary distribution | 9 (9%) | 89 (89%) | 0.001* |
BMI: Body mass index, HbA1c: Haemoglobin A1c, SD: Standard deviation, NPDR: Non-proliferative diabetic retinopathy, PDR: Proliferative diabetic retinopathy
NFC: Nail fold capillaroscopy. *p-value<0.05 was taken as statistically significant.
The qualitative capillary changes in healthy controls and patients with DR are depicted in Table 1. The difference in the NFC changes between healthy controls and DR patients was statistically significant (p = 0.001).
Patients with DR were further subdivided into those with proliferative DR (PDR) and non-proliferative DR (NPDR) (mild, moderate and severe) as per Diabetic Retinopathy Disease Severity Scale5 and their nail fold changes were observed and analysed [Table 2]. Statistically significant morphological capillary alterations were observed in PDR as compared to NPDR [Figures 9 and 10].
| NFC parameters | NPDR (n = 50), n (%) | PDR (n = 50), n (%) | p value | ||
|---|---|---|---|---|---|
| Mild (n = 5), n (%) | Moderate (n = 32), n (%) | Severe (n = 13), n (%) | |||
| Presence of dilated capillaries | 4 (80%) | 16 (50%) | 10 (76.92%) | 25 (50%) | 0.202 |
| Evidence of capillary dropouts | 0 | 0 | 0 | 4 (8%) | 0.244 |
| Presence of avascular areas | 0 | 13 (40.63%) | 11 (84.62%) | 47 (94%) | 0.001* |
| Presence of micro-haemorrhages | 1 (20%) | 1 (3.13%) | 4 (30.77%) | 21 (42%) | 0.002* |
| Bushy capillaries | 0 | 3 (9.38%) | 4 (30.77%) | 35 (70%) | 0.001* |
| Meandering capillaries | 0 | 0 | 2 (15.38%) | 31 (62%) | 0.001* |
| Tortuosity (>5% of capillaries) | 2 (40%) | 19 (59.38%) | 11 (84.62%) | 50 (100%) | 0.001* |
| Reduced capillary density | 0 | 3 (9.38%) | 10 (76.92%) | 48 (96%) | 0.001* |
| Subpapillary plexus visibility | 0 | 1 (3.13%) | 1 (7.69%) | 8 (16%) | 0.230 |
| Receding capillaries | 0 | 0 | 0 | 19 (38%) | 0.001* |
| Angulated capillaries | 0 | 0 | 3 (23.08) | 28 (56%) | 0.001* |
NFC: Nail fold capillaroscopy, NPDR: Non-proliferative diabetic retinopathy, PDR: Proliferative diabetic retinopathy. *p value <0.05 was taken as significant.
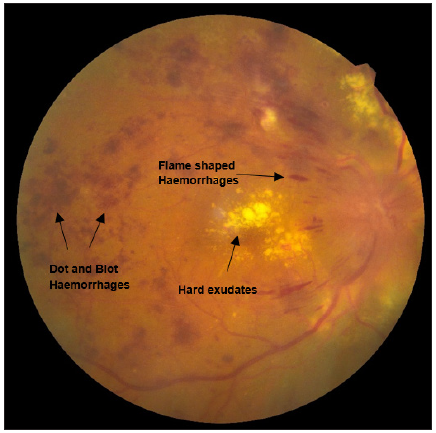
- Fundus examination showing findings suggestive of proliferative diabetic retinopathy with clinically significant macular oedema (CSME). Black arrows suggesting dot and blot haemorrhages, flame shaped haemorrhages and hard exudates.
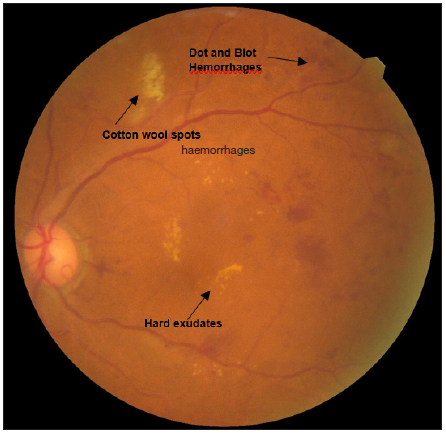
- Fundus examination showing findings (black arrows suggesting dot and blot haemorrhages, cotton wool spots and hard exudates) suggestive of moderate nonproliferative diabetic retinopathy.
The NFC parameters were compared in DR patients according to the duration of diabetes [Table 3]. The findings were found to be statistically significant (p < 0.03). Patients with DR were analysed based on their haemoglobin A1c (HbA1c) levels (<7%, 7–9%, 9.1–11%, >11%) reflecting their glycaemic control and the comparison is depicted in Table 4. Morphological capillary changes were more commonly seen in those with poor glycaemic control and were details are given in Table 4.
| NFC Parameters | Duration of diabetes (in years) | P-value | ||||
|---|---|---|---|---|---|---|
| ≤5 (n = 9), n (%) | 6–10 (n = 27), n (%) | 11–15 (n = 47), n (%) | 16–20 (n = 13), n (%) | >20 (n = 4), n (%) | ||
| Presence of dilated capillaries | 6 (66.67%) | 14 (51.85%) | 24 (51.06%) | 8 (61.54%) | 3 (75%) | 0.778 |
| Evidence of capillary dropouts | 0 | 0 | 3 (6.38%) | 1 (7.69%) | 0 | 0.588 |
| Presence of avascular areas | 1 (11.11%) | 16 (59.26%) | 38 (80.85%) | 12 (92.31%) | 4 (100%) | 0.001* |
| Presence of micro-haemorrhages | 0 | 5 (18.52%) | 17 (36.17%) | 3 (23.08%) | 2 (50%) | 0.112 |
| Bushy capillaries | 0 | 6 (22.22%) | 27 (57.45) | 7 (53.85%) | 2 (50%) | 0.003* |
| Meandering capillaries | 0 | 4 (14.81%) | 18 (38.30%) | 8 (61.54%) | 3 (75%) | 0.03* |
| Tortuosity (>5% of capillaries) | 3 (33.33%) | 20 (74.07) | 42 (89.36%) | 13 (100%) | 4 (100%) | 0.001* |
| Reduced capillary density | 0 | 10 (37.04%) | 36 (76.60%) | 12 (92.31%) | 3 (75%) | 0.001* |
| Subpapillary plexus visibility | 0 | 0 | 8 (17.02%) | 1 (7.69%) | 1 (25%) | 0.105 |
| Receding capillaries | 0 | 3 (11.11%) | 12 (25.53%) | 3 (23.08%) | 1 (25%) | 0.315 |
| Angulated capillaries | 0 | 4 (14.81%) | 17 (36.17%) | 7 (53.85%) | 3 (75%) | 0.005* |
NFC: Nail fold capillaroscopy, *p value<0.05 was taken as significant.
| NFC parameters | HbA1c levels | P-value | |||
|---|---|---|---|---|---|
| <7.0 (n = 15), n (%) | 7.0–9.0 (n = 42), n (%) | 9.1–11.0 (n = 36), n (%) | >11.0 (n = 7), n (%) | ||
| Presence of dilated capillaries | 6 (40%) | 23 (54.76%) | 24 (66.67%) | 2 (28.57%) | 0.150 |
| Evidence of Capillary drop outs | 0 | 0 | 3 (8.33%) | 1 (14.29%) | 0.109 |
| Presence of avascular areas | 8 (53.33%) | 24 (57.14%) | 32 (88.89%) | 7 (100%) | 0.002* |
| Presence of microhaemorrhagesC | 2 (13.33%) | 11 (26.19%) | 12 (33.33%) | 2 (28.57%) | 0.537 |
| Bushy capillaries | 3 (20%) | 12 (28.57%) | 22 (61.11%) | 5 (71.43%) | 0.003* |
| Meandering capillaries | 3 (20%) | 5 (11.90%) | 21 (58.33%) | 4 (57.14%) | 0.001* |
| Tortuosity (>5% of capillaries) | 10 (66.67%) | 30 (71.43%) | 35 (97.22%) | 7 (100%) | 0.005* |
| Reduced capillary density | 4 (26.67%) | 17 (40.48%) | 33 (91.67%) | 7 (100%) | 0.001* |
| Subpapillary plexus visibility | 1 (6.67%) | 4 (9.52%) | 4 (11.11%) | 1 (14.29%) | 0.943 |
| Receding capillaries | 1 (6.67%) | 4 (9.52%) | 12 (33.33%) | 2 (28.57%) | 0.027* |
| Angulated capillaries | 1 (6.67%) | 8 (19.05%) | 17 (47.22%) | 5 (71.43%) | 0.001* |
NFC: Nail fold capillaroscopy, HbA1c: haemoglobin A1c, *P < 0.05 was taken as significant.
Discussion
NFC can be used to assess T2DM-related complications in the proximal nail fold capillaries.8 The most common qualitative capillary changes in healthy controls were tortuous, meandering, capillary dilation and micro-haemorrhages as observed in previous studies.3,9,10 In our study, the NFC changes were significantly higher (p = 0.001) in DR patients. Tortuosity, avascular areas, reduced capillary density, micro-haemorrhages, and dilated, bushy, receding and angulated capillaries were common NFC findings in DR patients. The typical findings in diabetes may be due to the advanced glycation end-products (AGEs), which are known to be associated with macro- and microvascular complications.11 One of the pathomechanisms is the apoptosis of retinal capillary pericytes and endothelial cells.12 Contrarily, the well-known NFC features of CTD may be due to interaction between VEGF, antiangiogenic factors (angiostatin, endostatin, tumstatin, canstatin) and elevated levels of hypoxia-induced factor, which affects the capillaries and the surrounding connective tissue matrix.13 Thus, NFC features are regressive in advanced disease (capillary dropouts, avascular areas) and predominantly proliferative in early stages (capillary dilation, giant, bushy capillaries).
Maldonado et al. demonstrated that NFC changes in diabetic patients collaborated with ophthalmological findings in 18% of patients.14 A study done by Kaminska–Winciorek reported that the presence of mega capillaries, abnormal loops and altered capillary densities were seen more in DM of longer duration and high HbA1C.15 Various other studies have also recorded reduced capillary density, tortuosity, neoangiogenesis, haemorrhages, and avascular zones as the common findings in diabetics, which significantly correlated with the presence and degree of DR, duration and control of diabetes.16–20
The findings of our study were consistent with those of Mohanty et al., which reported tortuosity in 100% of patients with PDR and 81.8% with NPDR.21 In a study by Chang et al., including 35 diabetic patients and 20 healthy controls, it was found that tortuosity was the most common finding in PDR (68%).22
We studied the NFC features in DR patients according to the duration of diabetes. The findings were consistent with the study by Uyar et al. in which it was reported that diabetes years of patients having tortuosity, aneurysm, bizarre and micro-haemorrhage were significantly longer in patients with DR than without DR.8 Positive correlation of capillaroscopic findings and diabetes duration was also stated in Chang et al. study.22 The findings in our study are not consistent with the study done by Barchetta et al. in which NFC findings were independent of the duration of diabetes.16 Although these findings do not predict when the microvascular changes formed, there is a significant correlation between diabetes years and capillaroscopic findings in our study. It can be assumed that early detection of tortuosity, reduced capillary density, and dilated and microhaemorrhages may be a precursor of DR.
We studied the correlation of nail fold capillaries with the glycaemic index of the patient. The findings were consistent with the studies done by Hsu et al,18 Uyar et al 8 and, Rajaei et al 23 s which identified mega capillaries, increased tortuosity and neoangiogenesis as frequent changes in diabetic patients with longer duration and high HbA1c.
In a study done by El-Khalik et al, there was a significantly longer disease duration and significantly higher HbA1c in patients with DR than with non-DR.24 Also, it was seen that the frequencies of tortuosity and precapillary oedema were increased significantly in patients with HbA1c≥7% compared to patients with HbA1c <7% and most of these patients were with diabetic retinopathy. This could be attributed to some studies showing HbA1c as a predictor of diabetic retinopathy. A study revealed that when HbA1c was ≥6.8%, the odds ratio for diabetic retinopathy increased significantly.25
Limitations
A larger sample size study with different demographic populations could have provided a broader picture of NFC changes in type 2 DM.
Conclusion
Changes in NFC in diabetics had a significant association with the severity of DR, disease duration, and glycaemic control. These changes perhaps run parallel to the changes in the retina. Hence, nail fold capillaroscopy can be used as a valuable non-invasive tool not only for the diagnosis of microvascular complications but also for the prognosis of the disease and identifying patients at high risk of DR, thereby helping in early diagnosis and improving the quality of life of patients.
Ethical approval
The ethical approval number is 3385/D-26/2020 batch from Government Medical college, Amritsar, Punjab.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
References
- Capillaroscopy and the measurement of capillary pressure. Br J Clin Pharmacol. 2000;50:501-13.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetic retinopathy: Mechanism, diagnosis, prevention, and treatment. Bio Med Res Int. 2015;2015:854593.
- [CrossRef] [PubMed] [Google Scholar]
- Nail fold capillaroscopic changes in patients with type 2 diabetes mellitus: An observational, comparative study. Indian J Med Spec. 2020;11:28-33.
- [Google Scholar]
- Diagnosis and management of diabetes: Synopsis of the 2016 American Diabetes Association standards of medical care in diabetes. Ann Intern Med. 2016;164:542-52.
- [CrossRef] [PubMed] [Google Scholar]
- Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110:1677-82.
- [CrossRef] [PubMed] [Google Scholar]
- Capillaroscopic patterns in rheumatic diseases. Acta Reum Port. 2007;32:29-36.
- [PubMed] [Google Scholar]
- Assessment of the relationship between diabetic retinopathy and nailfold capillaries in type 2 diabetics with a non-invasive method: Nailfold videocapillaroscopy. J Diabetes Res. 2016;2016:7592402.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nailfold capillary patterns in healthy subjects: A real issue in capillaroscopy. Microvasc Res. 2013;90:90-5.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative nailfold capillaroscopy findings in a population with connective tissue disease and in normal healthy controls. Ann Rheum Dis. 1996;55:507-12.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetes and advanced glycation endproducts. J Intern Med. 2002;251:87-101.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of advanced glycation end products on accelerated apoptosis of retinal capillary cells under in vitro conditions. Life Sci. 2005;76:1051-60.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular disease in scleroderma: Angiogenesis and vascular repair. Rheum Dis Clin North Am. 2008;34:73-9.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold capillaroscopy in diabetes mellitus. Microvasc Res. 2017;112:41-6.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetic microangiopathy in capillaroscopic examination of juveniles with diabetes type 1. Postepy Hig Med Dosw. 2012;66:51-9.
- [PubMed] [Google Scholar]
- High prevalence of capillary abnormalities in patients with diabetes and association with retinopathy. Diabet Med. 2011;28:1039-44.
- [CrossRef] [PubMed] [Google Scholar]
- Microvascular abnormalities in capillaroscopy correlate with higher serum IL-18 and sE-selectin levels in patients with type 1 diabetes complicated by microangiopathy. Folia Histochem Cytobiol. 2011;49:104-10.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold capillary abnormalities are associated with type 2 diabetes progression and correlated with peripheral neuropathy. Medicine. 2016;95
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Computerized video-capillaroscopy alteration related to diabetes mellitus and its complications. In: Oxygen transport to tissue XL. 2018. p. :363-8.
- [Google Scholar]
- The evaluation of nailfold videocapillaroscopy findings in patients with type 2 diabetes with and without diabetic retinopathy. North Clin Istanb. 2019;6:146-50.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Can nailfold capillaroscopy be a screening tool for diabetic retinopathy-A hospital based cross-sectional study in Orissa, India. J Evid Based Med Healthc. 2021;8:1479-83.
- [Google Scholar]
- Use of dynamic capillaroscopy for studying cutaneous microcirculation in patients with diabetes mellitus. Microvasc Res. 1997;53:121-7.
- [CrossRef] [PubMed] [Google Scholar]
- Nailfold capillaroscopy findings in diabetic patients (A pilot cross-sectional study) Open J Pathol. 2015;5:65-72.
- [Google Scholar]
- Nail folds capillaries abnormalities associated with type 2 diabetes mellitus progression and correlation with diabetic retinopathy. Clin Med Insights: Endocrinol Diabetes. 2022;15:11795514221122828.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A comparison of the association of fasting plasma glucose and HbA1c levels with diabetic retinopathy in Japanese men. J Diabetes Res. 2020;2020
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






