Translate this page into:
Sebaceous cell carcinoma developing in epidermodysplasia verruciformis
2 Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Dipankar De
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh - 160 012
India
| How to cite this article: Kambhampati SB, Vinay K, De D, Handa S, Gaspar BL, Saikia UN. Sebaceous cell carcinoma developing in epidermodysplasia verruciformis. Indian J Dermatol Venereol Leprol 2016;82:433-435 |
Sir,
Epidermodysplasia verruciformis is a rare genodermatosis with an increased susceptibility to infection by specific strains of human papilloma virus. These patients are also predisposed to develop various cutaneous malignancies, most commonly squamous cell carcinoma especially on the sun-exposed areas.[1] We report a patient with epidermodysplasia verruciformis who subsequently developed sebaceous cell carcinoma. We were unable to find any previous report of sebaceous cell carcinoma in association with this condition.
A 28-year-old man presented with a 20-year history of asymptomatic, erythematous, raised lesions on the neck, face and hands along with multiple flat hypopigmented lesions on the trunk and extremities. His elder sister had also suffered from similar skin lesions since early childhood. In 2008, he had been diagnosed to have epidermodysplasia verruciformis at another healthcare facility before he presented to us and had received acitretin 25mg/day for 1 year then with minimal improvement. Two years back, he noticed an increase in size of a pre-existing lesion on his right parotid region which became painful and eventually formed an ulcerated fungating mass with purulent discharge. His current medications included topical emollients and sunscreens. Physical examination revealed multiple, well-defined, irregular, hypopigmented plaques of variable size on the trunk and extremities in addition to erythematous, flat-topped papules and plaques on dorsal hands and neck [Figure - 1]. A 5 cm × 3 cm ulcero-proliferative mass was seen overlying the right angle of the mandible. On palpation, it was free from the underlying bone.
 |
| Figure 1: (a) An ulceroproliferative mass of 5 cm × 3 cm on the right angle of mandible. (b) Multiple well-defined hypopigmented plaques of variable size resembling pitryiasis versicolor on the upper limb and trunk and multiple flat, skin colored papules resembling plane warts on the dorsum of the hand. (c) 2 months after undergoing wide local excision |
Histopathological examination of a biopsy from the mass revealed surface ulceration and the presence of tumor cells which were arranged as clusters and lobules in the underlying dermis. The tumor cells had large centrally placed pleomorphic nuclei, conspicuous nucleoli, abundant vacuolated cytoplasm, scalloping of nuclei and mitotic activity suggestive of sebaceous carcinoma. Immunohistochemistry with epithelial membrane antigen was diffusely positive and periodic acid-Schiff stain was negative thus confirming the diagnosis of sebaceous carcinoma [Figure - 2]. Histopathological examination of a biopsy from a flat-topped papule revealed mild hyperkeratosis, acanthosis and papillomatosis with full thickness dysplasia suggestive of Bowen's disease [Figure - 3]. The clinical presentation was characteristic and the histopathological features were considered to be consistent with lesions seen in epidermodysplasia verruciformis, though histopathological findings typical of the disease were not seen. An abdominal ultrasound, colonoscopy, chest X-ray and routine urine examination were unremarkable, thus excluding an association with Muir-Torre syndrome. There was no clinical evidence of distant metastasis. Computed tomographic imaging of the head, neck, thorax and abdomen did not reveal any radiological evidence of metastasis. He underwent wide local excision and is currently undergoing radiotherapy.
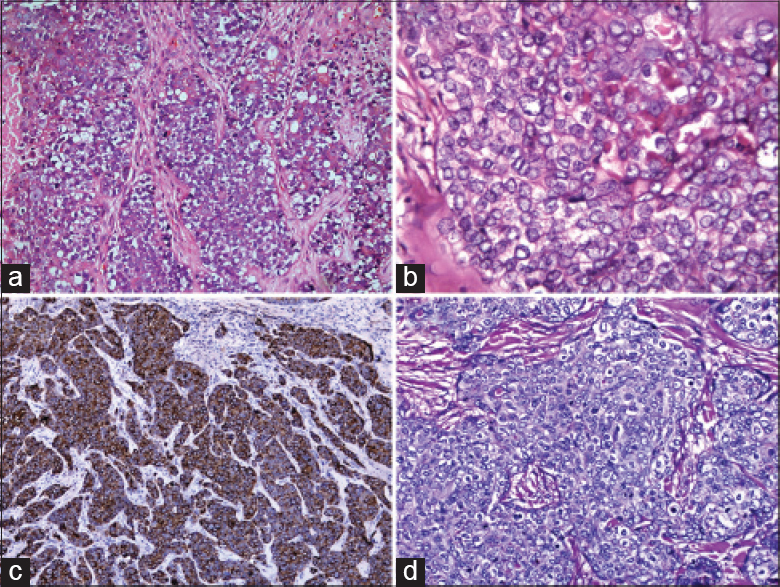 |
| Figure 2: (a) Tumor cells with abundant multivacuolated cytoplasm and brisk mitosis. (H and E, ×200) (b) High power view showing tumor cells with centrally placed nuclei. (H and E, ×400). (c) Immunohistochemistry with epithelial membrane antigen showing diffuse positivity. (Epithelial membrane antigen, ×100). (d) Immunohistochemistry with periodic acid-Schiff stain showing diffuse negativity. (Periodic acid-Schiff, ×200) |
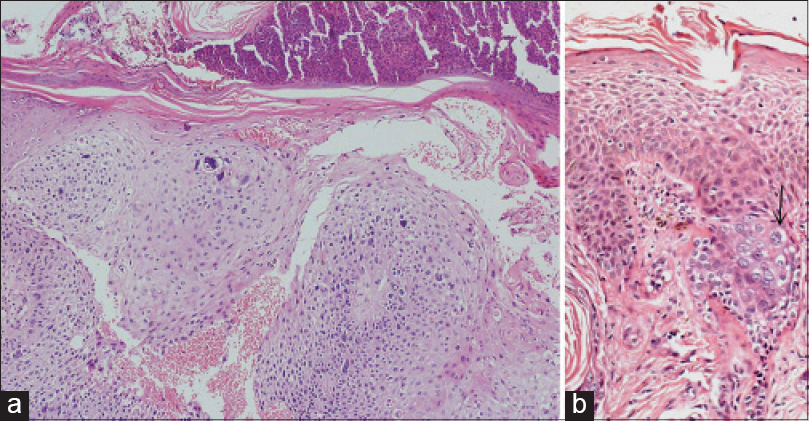 |
| Figure 3: (a) Mild hyperkeratosis, acanthosis, papillomatosis and full thickness dysplasia (H and E, ×200). (b) Focus of large cells with pale cytoplasm, perinuclear halo and prominent nucleoli (arrow) (H and E, ×200) |
Epidermodysplasia verruciformis is an autosomal recessive disorder due to mutations in the epidermodysplasia verruciformis 1 and epidermodysplasia verruciformis 2 genes located on chromosome 17q25. The disease was first described by Lewandowsky and Lutz in 1922.[2] The condition presents with widespread and persistent human papilloma virus infection, mostly due to subtypes 5 and 8.[1] It is believed that there occurs selective loss of T-lymphocyte immune response against human papilloma virus, most likely due to the defective presentation of viral antigens on the surface of keratinocytes leading to widespread infection.[3] Mutation in epidermodysplasia verruciformis genes is also proposed to cause unchecked proliferation of stem cells and transient amplifying cells infected with human papilloma virus 5 and 8.[4]
The disease manifests as two main phenotypes which differ in the potential for malignant transformation. The more benign lesions typically present as flat, wart-like, hypopigmented or hyperpigmented papules that may coalesce to form scaly patches or plaques with irregular borders resembling tinea versicolor. These lesions are most prevalent on the trunk, neck and extremities. The lesions with greater malignant potential present more variably as verrucous and seborrheic keratosis-like lesions, occurring more frequently on sun-exposed surfaces including face, hands and feet. About 30–60% of individuals with the condition eventually develop skin malignancies, mostly in the fourth and fifth decade. The common malignancies reported are squamous cell carcinoma and Bowen's disease. Adnexal carcinoma is also reported, but is rare.[2]
Sebaceous carcinoma is a rare tumor associated with a high rate of local recurrence and metastasis to lymph nodes and internal organs. The periocular region is most commonly affected. Histopathologically, the tumor consists of irregular lobules and sheets of cells with varying degrees of sebaceous differentiation that show scalloped, centrally located nuclei with foamy multi-vacuolated cytoplasm due to the presence of intra-cytoplasmic lipids. Areas of necrosis, marked nuclear atypia and abnormal mitotic figures may also be noted. Histologically, the clear cell variant of squamous cell carcinoma can mimic sebaceous carcinoma. Immunohistochemistry with periodic acid-Schiff stain and epithelial membrane antigen helps to differentiate these two tumors as clear cell carcinoma shows moderate to strong periodic acid-Schiff positivity and epithelial membrane antigen negativity.[5] Over expression of p53 and human papilloma virus infection has been implicated in the pathogenesis and progression of sebaceous carcinoma thus explaining its likely occurrence in our patient.[6]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Gül U, Kiliç A, Gönül M, Cakmak SK, Bayis SS. Clinical aspects of epidermodysplasia verruciformis and review of the literature. Int J Dermatol 2007;46:1069-72.
[Google Scholar]
|
| 2. |
Sri JC, Dubina MI, Kao GF, Rady PL, Tyring SK, Gaspari AA. Generalized verrucosis: A review of the associated diseases, evaluation, and treatments. J Am Acad Dermatol 2012;66:292-311.
[Google Scholar]
|
| 3. |
Sá NB, Guerini MB, Barbato MT, Di Giunta G, Nunes DH. Epidermodysplasia verruciformis: Clinical presentation with varied forms of lesions. An Bras Dermatol 2011;86 4 Suppl 1:S57-60.
[Google Scholar]
|
| 4. |
Orth G. Genetics of epidermodysplasia verruciformis: Insights into host defense against papillomaviruses. Semin Immunol 2006;18:362-74.
[Google Scholar]
|
| 5. |
Al-Arashi MY, Byers HR. Cutaneous clear cell squamous cell carcinoma in situ: Clinical, histological and immunohistochemical characterization. J Cutan Pathol 2007;34:226-33.
[Google Scholar]
|
| 6. |
Hayashi N, Furihata M, Ohtsuki Y, Ueno H. Search for accumulation of p53 protein and detection of human papillomavirus genomes in sebaceous gland carcinoma of the eyelid. Virchows Arch 1994;424:503-9.
[Google Scholar]
|
Fulltext Views
3,243
PDF downloads
2,445





