Translate this page into:
A rare case of multiple genital and perianal melanoacanthomas
2 Department of Pathology, KS Hegde Medical Academy, Deralakatte, Mangalore, Karnataka, India
Correspondence Address:
Tonita M Noronha
"Chrisedo," Melthota, Kulshekar, Mangalore - 575 005, Karnataka
India
| How to cite this article: Noronha TM, Girisha BS, Kishanprasad HL, Fernandes MS. A rare case of multiple genital and perianal melanoacanthomas. Indian J Dermatol Venereol Leprol 2012;78:202-204 |
Sir,
Melanocytic lesions have always posed a fascinating and even bewildering array of diagnostic problems for the dermatologist. The term melanoacanthoma was introduced by Mishima and Pinkus in 1960 to designate a benign skin tumor that consisted of proliferating melanocytes and keratinocytes. [1] It is now regarded as a heavily pigmented seborrheic keratosis by most authorities. [2] Cutaneous melanoacanthoma is a painless, slow-growing, benign, mixed neoplasm composed of melanocytes scattered throughout keratinocyte lobules, rather than being limited to the basal layer of these lobules. [3] Although the keratinocytes contain melanin, the bulk of the pigment is present within melanocytes, many of which also have long dendrites. [2] Cutaneous melanoacanthomas are mainly found on the head, particularly the lips, and the trunk.
A 39-year-old male patient, farmer by occupation, presented with multiple pigmented growths over the inner thighs, external genitalia, perianal areas and buttocks since the age of 12 years. To begin with, the lesions were small and asymptomatic, with gradual increase in size. He complained of pain, bleeding and oozing from the lesions since 3 months. There was no history suggestive of risk of exposure to sexually transmitted diseases (STDs). Cutaneous examination revealed multiple hyperpigmented papules, plaques and nodules with a lobulated surface over the upper and medial aspects of both thighs, penile shaft, gluteal cleft and buttocks [Figure - 1]a and b. Mucous membranes were not involved and there was no lymphadenopathy. With these clinical findings, seborrheic keratosis, condyloma acuminata and melanoacanthoma were considered in the differential diagnosis. His complete blood count, renal function tests and blood sugar levels were within normal limits. Venereal Diseases Research Laboratory and human immunodeficiency virus enzyme-linked immunosorbent assay were nonreactive and hepatitis B surface antigen and anti-hepatitis C virus were negative. One of the cutaneous lesions was excised and sent for histopathological examination. Epidermis showed hyperkeratosis, acanthosis and marked papillomatosis with proliferation of spinous layer cells with dense melanin pigmentation. Numerous true and pseudohorn cysts were seen [Figure - 2]a and b. Large dendritic cells with abundant melanin granules were spread throughout the epidermis [Figure - 2]c. Dermis was unremarkable. Features were consistent with melanoacanthoma.
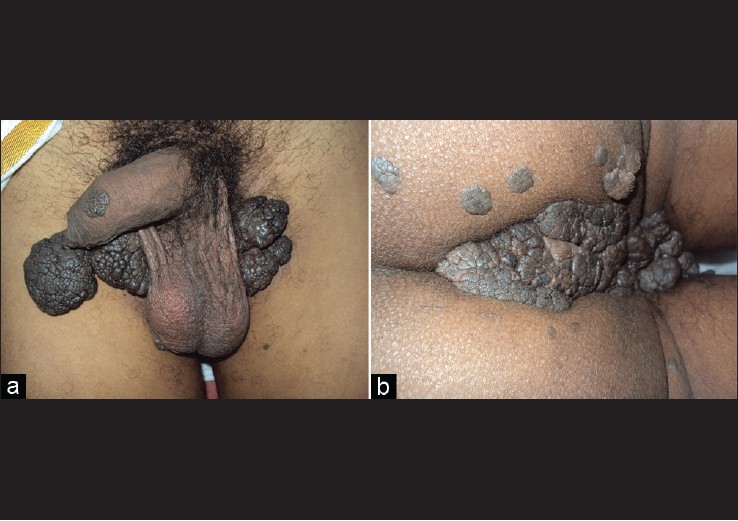 |
| Figure 1: (a) Hyperpigmented plaques and nodules with a lobulated surface over the thighs and penile shaft. (b) Hyperpigmented papules and plaques with a lobulated surface over the gluteal cleft and buttocks |
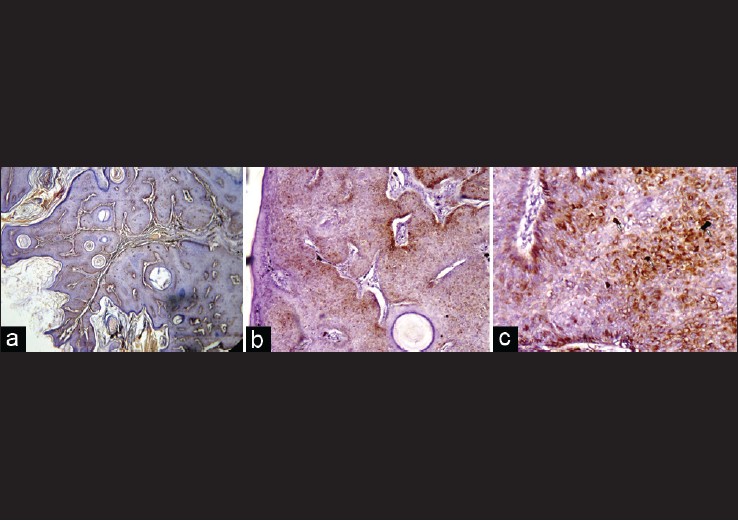 |
| Figure 2: (a) Epidermis showing hyperkeratosis, acanthosis, marked papillomatosis and horn cysts (H and E, × 40). (b) Epidermis showing papillomatosis and proliferation of spinous layer cells with dense melanin pigmentation. Numerous true and pseudohorn cysts also seen (H and E, × 100). (c) Large dendritic cells with abundant melanin dispersed throughout the epidermis shown in arrows (H and E, × 400) |
Melanoacanthoma can be found both on the skin and on the oral mucosa. Although most authors consider cutaneous melanoacanthoma a benign tumor of melanocytes and keratinocytes, some have suggested that it may be a reactive phenomenon induced by localized trauma. [4] Cutaneous melanoacanthomas are painless and slow-growing. Patients are generally asymptomatic; however, trauma or manipulation of the melanoacanthoma may lead to bleeding or inflammation. Patients may live with cutaneous melanoacanthoma for decades before they seek treatment. [4]
Cutaneous melanoacanthomas are found mainly on the trunk or head, often on the lip or eyelid. They have also been observed on the penile shaft. Cutaneous melanoacanthomas may be hyperpigmented or verrucous and round or oval. The lesion may be a papule, plaque, cutaneous horn or nodule. [4]
Melanoacanthoma is a deeply pigmented rare histological variant of seborrheic keratosis. Histologically, two types of melanoacanthomas are described: diffuse type in which melanocytes are unevenly scattered throughout the lesion and clonal type in which melanocytes and keratinocytes are clustered in small nests. [5] Our case was of the diffuse type of melanoacanthoma.
Cutaneous melanoacanthoma is a relatively uncommon tumor and most often solitary. In our case, there were multiple lesions, the smallest measuring 5 mm in diameter and the largest measuring 7.5 cm × 5 cm, situated in an uncommon location. The patient was referred to a plastic surgeon. Excision of the larger lesions and split-skin grafting was done. Histopathology showed features consistent with melanoacanthoma. Case reports of multiple cutaneous melanoacanthomas are rare. Hence, this case is reported.
| 1. |
Lambert WC, Lambert MW, Mesa ML, Schneider LC, Fischman GJ, Abbey AH, et al. Melanoacanthoma and related disorders. Simulants of acral- lentiginous (P-P-S-M) melanoma. Int J Dermatol 1987;26:508-10.
[Google Scholar]
|
| 2. |
Cockerell CJ, Larsen F. Benign epidermal tumors and proliferations. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2 nd ed. Spain: Mosby Elsevier; 2008. p. 1661-4.
[Google Scholar]
|
| 3. |
Kihiczak GG, Centurion SA, Schwartz RA, Lambert WC. Giant cutaneous melanoacanthoma. Int J Dermatol 2004;43:936-7.
[Google Scholar]
|
| 4. |
Schwartz RA, Lambert WC, Kihiczak GG. Cutaneous melanoacanthoma. Available from: http://emedicine.medscape.com/article/1061812. [Last Accessed on 2011 Jul 10].
[Google Scholar]
|
| 5. |
Choudhary SV, Bhake A, Singh A, Gupta S. Pigmented cerebriform growth over forehead. Indian J Pathol Microbiol 2010;53:375-6.
[Google Scholar]
|
Fulltext Views
2,801
PDF downloads
3,224





