Translate this page into:
Angiolymphoid hyperplasia with arterial ectasia and arteriovenous malformation: Response to intra-arterial embolization
2 Department of Radiology, Jawaharlal Nehru Medical College, Sawangi, Wardha, Maharashtra, India
Correspondence Address:
Nitin R Lade
Department of Dermatology, Jawaharlal Nehru Medical College, Sawangi, Wardha, Maharashtra
India
| How to cite this article: Lade NR, Banode P, Dhope N, Tharafdar P, Saoji V. Angiolymphoid hyperplasia with arterial ectasia and arteriovenous malformation: Response to intra-arterial embolization. Indian J Dermatol Venereol Leprol 2016;82:413-415 |
Abstract
Angiolymphoid hyperplasia with eosinophilia is a rare disease characterized by vascular proliferation of unknown origin. The lesions are mostly seen in the head and neck region and are characterized by papules or nodules. A 20-year-old man presented with a 1 year history of reddish papulo-nodular lesions overlying a pulsatile swelling on the left auricular area. Histopathology was suggestive of angiolymphoid hyperplasia with eosinophilia. B-mode ultrasonography, color Doppler and angiography revealed arterial ectasia and arteriovenous malformation of the left auricular artery. Such malformations have been reported previously, in association with angiolymphoid hyperplasia with eosinophilia. The cutaneous lesions responded well to transarterial embolization of the nidus.Introduction
Wells and Whimster first described angiolymphoid hyperplasia with eosinophilia in 1969.[1] It is an uncommon benign vascular neoplasm of unknown origin also known as epithelioid hemangioma as the endothelial cells demonstrate an epithelioid morphology.[2] Rarely, it may associated with underlying arterial ectasia or arteriovenous malformation.
Case Report
A 20-year-old man presented with a 1 year history of itchy, erythematous papules and nodules on the left ear and retroauricular region associated with bleeding on trauma and intermittent pain. At places, hemorrhagic crusts were seen [Figure - 1]. A non-tender, ill-defined, soft, compressible, pulsatile mass of 3 cm × 2 cm size was palpable in the left retroauricular region, pushing the pinna forward. The patient described feeling the pulsatile swelling develop under the left retroauricular area lesions a few months prior to presentation. No regional or systemic lymphadenopathy was seen. There was no history of headache, visual, or neurological impairment, prior trauma, topical applications or similar complaints in the family. He had previously been treated with five sessions of cryotherapy for the skin lesions with partial response and rapid relapse. Complete blood count, liver and kidney functions were normal.
 |
| Figure 1: (a) Erythematous papulonodular lesions with pulsatile swelling, pushing left pinna forward, (b) about 70% clearance after embolization |
Histopathological examination revealed multiple dilated vascular channels with epithelioid endothelial cells and a perivascular inflammatory infiltrate in the dermis composed of lymphocytes and eosinophils. No lymphoid follicle formation was observed [Figure - 2]. B-mode ultrasonography of the left retroauricular region showed ectatic dilatation of a posterior auricular artery with a hypoechoic shadow in the arterial wall suggestive of mural thickening due to intra-arterial pathology [Figure - 3]. Color doppler of the lesion revealed high vascularity within the lesion (nidus), and; on spectral doppler, low resistance blood flow was observed within the arteries. Arterialization of the draining vein was also observed, suggesting an underlying arteriovenous malformation [Figure - 4]. Vascular channels were also observed within the thickened arterial wall. Angiography demonstrated a high flow nidus with feeder branches from the posterior auricular artery which itself exhibited ectatic dilatation. [Figure - 5]. No intracranial vascular connection was observed. As the patient was not willing to undergo surgery, radiological intervention was planned. Under general anesthesia, using the right transfemoral approach, selective access to the nidus of arteriovenous malformation was achieved using Progreat microcatheter (Terumo) and then superselective embolization was performed with a 20% mixture of N-butyl acrylate glue and lipiodol. Around 90% embolization was achieved during the first session. There were no procedural or post-procedural complications. Follow-up after 6 weeks showed around 70% clearance of the skin lesions with the remaining lesions decreasing in size. It requires further sessions to embolise it completely. Retroauricular mass and pulsation disappeared. Angiography showed almost complete obliteration of vascular ectasia [Figure - 5].
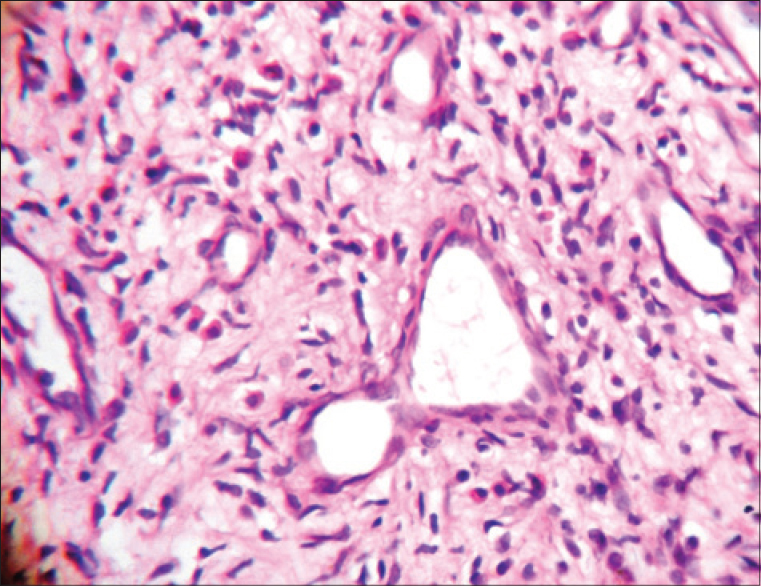 |
| Figure 2: Multiple dilated vascular channels with inflammatory cells and epithelioid endothelial cells |
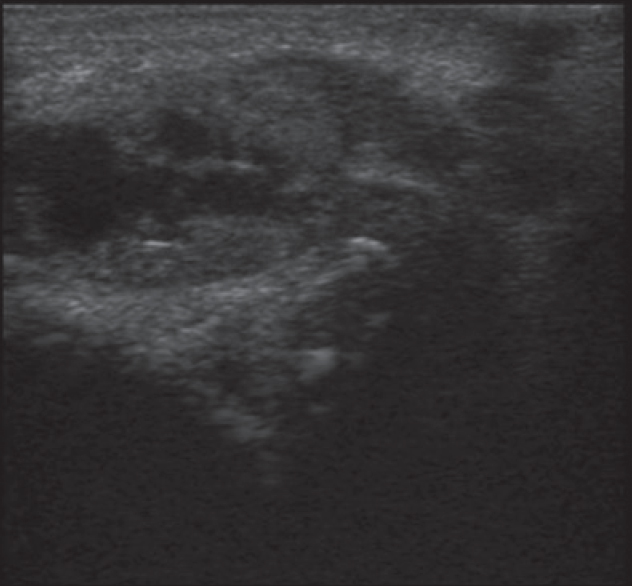 |
| Figure 3: B-mode ultrasonography showing dilatation and thickening of left postauricular artery |
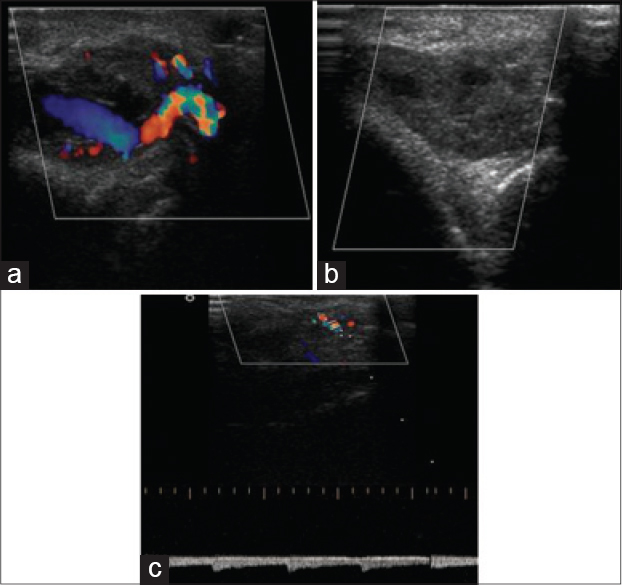 |
| Figure 4: Color Doppler studies showing (a) increased vascularity of the artery, (b) posttreatment obliteration of the blood flow, (c) low resistance blood flow seen in arteries and arterialization in draining vein suggestive of arteriovenous malformation |
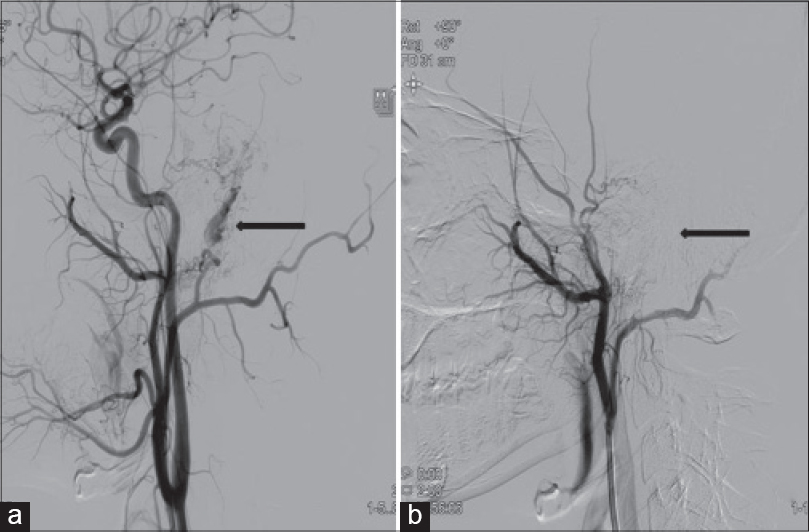 |
| Figure 5: (a) Angiography revealed ectasia, (b) post procedure, there is complete obliteration of vascular ectasia |
Discussion
Angiolymphoid hyperplasia with eosinophilia is a benign proliferation of capillaries and venules that usually affects young adults, with the head and neck region being the most frequent site of occurrence.[3],[4],[5] Cutaneous lesions are usually asymptomatic but may be pruritic, painful and hemorrhagic and manifest as papules, nodules, or plaques.[4],[5] Peripheral eosinophilia is an inconsistent feature seen in 21% of cases.[4],[5] Diagnosis is based on the histological identification of small vessel proliferation lined by epithelioid endothelial cells, associated with a mixed inflammatory infiltrate as seen in our case.[3],[4],[5]
It is unclear whether this entity represents a reactive proliferation or a low-grade neoplastic process.[6] When it occurs in the subcutaneous/deep soft tissue, a medium sized vessel such as an artery (39%) or vein (24%) is often observed close to, or in continuity with the lesion.[3] However, the presence of cutaneous lesions along with ectasia and arteriovenous malformation of the underlying artery is a rare presentation.[7] Such cases may be poorly responsive to treatment and have a high recurrence rate.[8] This may explain why the lesions in our patient failed to respond to multiple sessions of cryotherapy.
The high vascularity of the thickened arterial wall in our patient could represent intra-arterial angiolymphoid hyperplasia. However since the lesion was not excised, this is difficult to confirm. Similar case reports of pulsatile lesions on the neck and axillary areas turned out to be intra-arterial angiolymphoid hyperplasia. However no associated cutaneous lesions were reported.[9],[10] Its association with arteriovenous malformation and ectasia is a rare phenomenon. The presence of cutaneous lesions could be a reactive proliferation due to the underlying ectasia, arteriovenous malformation or intra-arterial pathology.[11] This finding is again supported by the subsidence of around 70% of the skin lesion after arterial embolization. A similar case was reported by Aoki et al.[12] We suggest active evaluation of angiolymphoid hyperplasia with eosinophilia for associated underlying vascular anomalies, the treatment of which may help the cutaneous lesions.
Acknowledgment
Special thanks to Late Dr. Anand Goverdhan for his support.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Wells GC, Whimster IW. Subcutaneous angiolymphoid hyperplasia with eosinophilia. Br J Dermatol 1969;81:1-14.
[Google Scholar]
|
| 2. |
Allen PW, Ramakrishna B, MacCormac LB. The histiocytoid hemangiomas and other controversies. Pathol Annu 1992;27 Pt 2:51-87.
[Google Scholar]
|
| 3. |
Fetsch JF, Weiss SW. Observations concerning the pathogenesis of epithelioid hemangioma (angiolymphoid hyperplasia). Mod Pathol 1991;4:449-55.
[Google Scholar]
|
| 4. |
Chun SI, Ji HG. Kimura's disease and angiolymphoid hyperplasia with eosinophilia: Clinical and histopathologic differences. J Am Acad Dermatol 1992;27(6 Pt 1):954-8.
[Google Scholar]
|
| 5. |
Chong WS, Thomas A, Goh CL. Kimura's disease and angiolymphoid hyperplasia with eosinophilia: Two disease entities in the same patient: Case report and review of the literature. Int J Dermatol 2006;45:139-45.
[Google Scholar]
|
| 6. |
Calonje E. Vascular tumors: Tumors and tumors-like conditions of blood vessels and lymphatics. In: Elder D, Elenitsas R, Johnson B Jr, Murphy G, Xu X, editors. Lever's Histopathology of the Skin. 10th ed. Philadelphia: Lippincott William and Wilkins; 2009. p. 1022.
[Google Scholar]
|
| 7. |
Onishi Y, Ohara K. Angiolymphoid hyperplasia with eosinophilia associated with arteriovenous malformation: A clinicopathological correlation with angiography and serial estimation of serum levels of renin, eosinophil cationic protein and interleukin 5. Br J Dermatol 1999;140:1153-6.
[Google Scholar]
|
| 8. |
Olsen TG, Helwig EB. Angiolymphoid hyperplasia with eosinophilia. A clinicopathologic study of 116 patients. J Am Acad Dermatol 1985;12(5 Pt 1):781-96.
[Google Scholar]
|
| 9. |
Cornelius RS, Biddinger PW, Gluckman JL. Angiolymphoid hyperplasia with eosinophilia of the head and neck. AJNR Am J Neuroradiol 1995;16 4 Suppl: 916-8.
[Google Scholar]
|
| 10. |
Bhat SP, Moorthy N, Ramalingam R, Jayapal M, Nanjappa MC. Angiolymphoid hyperplasia with eosinophilia presenting as a giant axillary artery aneurysm. Vascular 2010;18:49-52.
[Google Scholar]
|
| 11. |
Nix M. Angiolymphoid hyperplasia with eosinophilia in association with a vascular malformation. Clin Exp Dermatol 2009;47:272-3.
[Google Scholar]
|
| 12. |
Aoki M, Kimura Y, Kusunoki T, Tahara S, Kawanah S. Angiolymphoid hyperplasia with eosinophilia associated with anomalous dilatation of occipital artery: IL-5 and VEGF expression of lesional mast cells. Arch Dermatol 2002;138:982-4.
[Google Scholar]
|
Fulltext Views
2,710
PDF downloads
1,840





