Translate this page into:
Juvenile IgA pemphigus: A case report and review of literature
Correspondence Address:
Raghavendra Rao
Additional Professor, Department of Dermatology, Kasturba Medical College, Manipal University, Manipal - 576 104, Karnataka
India
| How to cite this article: Neethu KC, Rao R, Balachandran C, Pai S. Juvenile IgA pemphigus: A case report and review of literature. Indian J Dermatol Venereol Leprol 2016;82:439-442 |
Sir,
A 6-year-old girl, born of a third degree consanguineous marriage, presented with a three year history of recurrent blistering all over the body. At presentation, she had generalized, multiple annular to circinate lesions with central crusting and accumulation of pus at the margins. Some pustules as well as discrete flaccid vesicles with hypopyon formation were also seen on the trunk [Figure - 1]. Blisters, initially containing clear fluid, would become pus-filled within 2 days and then expand peripherally in a ring-like fashion before healing in about 10 days with hyperpigmentation. The oral cavity was normal. A Tzanck smear taken from a vesicle showed polymorphonuclear leukocytes; bacterial culture of pus yielded no growth after 48 hours. Skin biopsy of a vesicle revealed a subcorneal blister containing neutrophils [Figure - 2]. Direct immunofluorescence microscopy from peri-lesional skin showed intercellular IgA staining in the upper epidermis; indirect immunofluorescence microscopy using the patient's serum and normal human skin as a substrate revealed circulating IgA antibodies in a titer of 1:10, with an intercellular epidermal staining pattern [Figure - 3]. Enzyme-linked immunosorbent assays for anti-desmoglein-1 and 3 immunoglobulin G were negative; we did not have the facilities to test for anti-desmocollin-1. A final diagnosis of subcorneal pustular dermatosis type of IgA pemphigus was made. In view of her extensive skin lesions, our patient was commenced on tapering doses of oral steroids (prednisolone 30 mg/day) along with dapsone (25 mg/day), with which she showed good improvement.
 |
| Figure 1: (a) Multiple annular and circinate vesiculopustules all over the body (b) close-up of the back showing some vesicles containing pus in the dependent part (hypopyon sign, indicated by arrow) |
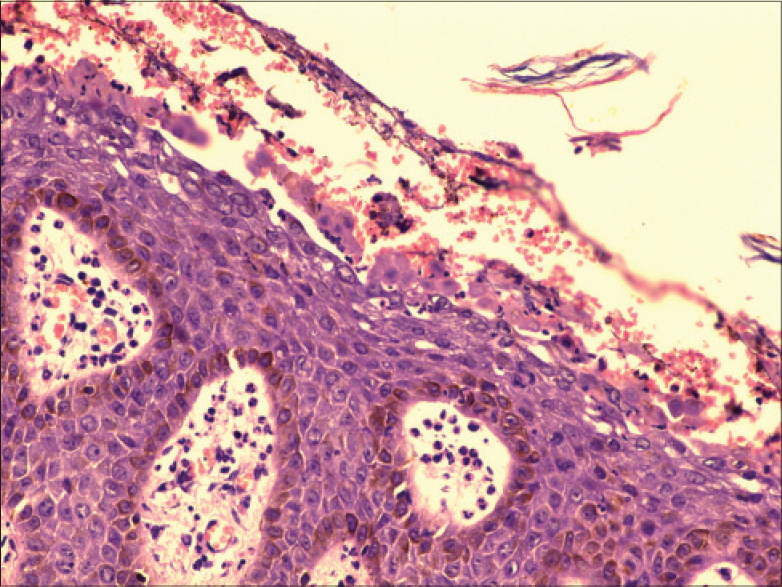 |
| Figure 2: Subcorneal blister containing neutrophils (H and E, ×200) |
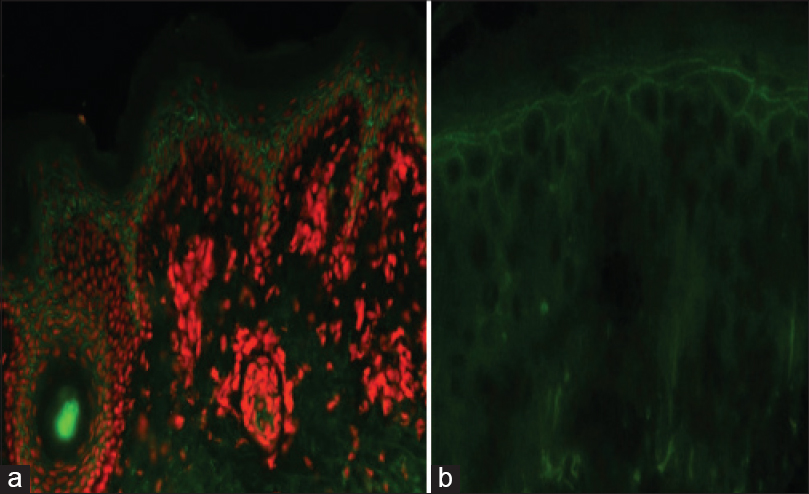 |
| Figure 3: (a) Intercellular staining of upper epidermis with immunoglobulin A by direct immunofluorescence (FITC, ×200). (b) Indirect immunofluorescence using normal human skin as a substrate showing intercellular staining in 1:10 titer (FITC, ×400) |
Autoimmune blistering diseases are rare in the pediatric age group. A retrospective study from a pediatric dermatology referral center catering to a population of 4 million people identified only 23 cases of immunobullous diseases in patients <18 years of age over a 16-year period.[1] The most frequent pediatric immunobullous disease is linear IgA disease (chronic bullous dermatosis of childhood, CBDC); all other conditions occur less frequently in children than in adults. Intercellular deposition of IgA as a primary feature is quite uncommon among children.[2]
IgA pemphigus is a rare subtype of pemphigus; until 2010, only approximately 70 cases had been reported.[3] It occurs most commonly in the middle aged and elderly; the average age of onset is 48 years.[3] There are two types of IgA pemphigus: the subcorneal pustular dermatosis type and the intra-epidermal neutrophilic type. Patients with both types of IgA pemphigus present with vesiculo-pustules. The axilla and groin are the sites of predilection but the trunk and proximal extremities are also commonly involved. Mucous membranes, palms and soles are usually spared.[3]
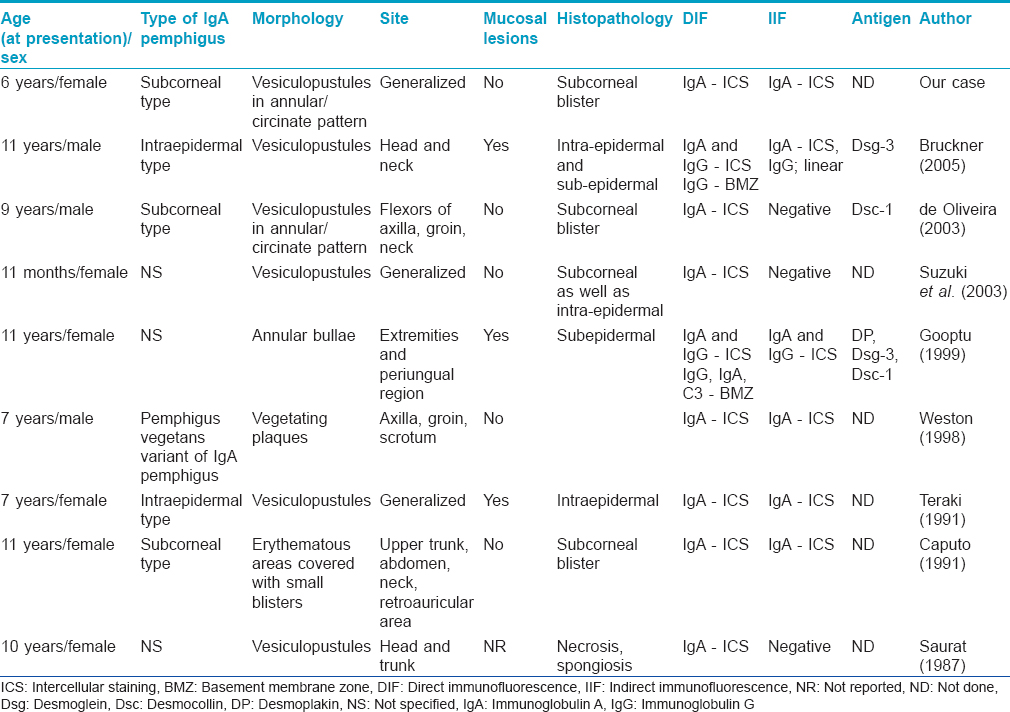
IgA pemphigus appears to be extremely rare in children; we could find only 8 previous reports in the English literature.[2],[4],[5],[6],[7],[8],[9],[10] The youngest reported patient was a 1-month-old girl. It appears to be more common in girls as compared to boys. [Table - 1] summarizes the key clinical and microscopic features of our patient as well as the eight other reported cases of childhood IgA pemphigus. Weston et al. reported a unique pemphigus vegetans variant of IgA pemphigus in a child.[6] Teraki et al. reported a 7-year-old girl with IgA pemphigus who, in addition to cutaneous involvement, had extensive erosions of the buccal mucosa, tongue, palate and tonsils.[9] The antigen associated with the subcorneal pustular dermatosis type was identified as desmocollin-1; the nature of the antigen involved in the intra-epidermal neutrophilic type is still unknown; autoantibodies to either desmoglein-1 or desmoglein-3 have been reported in some cases.[3] Gooptu et al. identified IgA and IgG antibodies to desmoplakin, desmocollin-1 and desmoglein-3 in a child with blistering of the skin and mucous membranes; she did not have an underlying malignancy.[8]
Histopathological examination of IgA pemphigus shows neutrophilic infiltration in the epidermis; occasionally, minimal acantholysis may be found. In the subcorneal pustular dermatosis type, pustules are located subcorneally. The intra-epidermal neutrophilic type, on the other hand, is characterized by suprabasilar cleavage confined to the lower epidermis or involving the entire epidermis. Since acantholysis in IgA pemphigus is minimal and sometimes even absent, it can be argued that immunofluorescence should be employed as an early screening test for the diagnosis of patients with widespread pustular eruptions. Direct immunofluorescence microscopy of peri-lesional skin is the gold standard test and detects IgA deposition in the intercellular spaces of the epidermis in all cases.[3] In the subcorneal pustular dermatosis subtype, IgA deposition is limited to the upper epidermal cell surfaces whereas in the intraepidermal neutrophilic subtype, intercellular IgA staining is seen either throughout the epidermis or restricted to the lower epidermis. Circulating antibodies are found in <50% of patients on standard substrates. The titers are usually low and the clinical significance of antibody titers is not known.[3] IgA pemphigus, particularly of the subcorneal pustular dermatosis type, has been reported to be associated with monoclonal IgA gammopathy. The main differential diagnosis of IgA pemphigus in children includes impetigo contagiosa, linear IgA disease, subcorneal pustular dermatosis and pemphigus foliaceus.[2] The overall prognosis in children with IgA pemphigus seems to be good and the disease can be easily controlled by a combination of low dose steroids and dapsone.[2]
Dapsone is usually considered to be the drug of choice.[3] Other drugs known to be effective include colchicine, prednisone, acitretin, isotretinoin, tetracycline, sulfamethoxypyridazine, cotrimoxazole, methotrexate, cyclosporine, adalimumab, azathioprine and psoralen and ultraviolet A (PUVA) therapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Weston WL, Morelli JG, Huff JC. Misdiagnosis, treatments, and outcomes in the immunobullous diseases in children. Pediatr Dermatol 1997;14:264-72.
[Google Scholar]
|
| 2. |
Caputo R, Pistritto G, Gianni E, Carminati G, Crupi A, Berti E, et al. IgA pemphigus in a child. J Am Acad Dermatol 1991;25 (2 Pt 2):383-6.
[Google Scholar]
|
| 3. |
Porro AM, Caetano Lde V, Maehara Lde S, Enokihara MM. Non-classical forms of pemphigus: Pemphigus herpetiformis, IgA pemphigus, paraneoplastic pemphigus and IgG/IgA pemphigus. An Bras Dermatol 2014;89:96-106.
[Google Scholar]
|
| 4. |
Bruckner AL, Fitzpatrick JE, Hashimoto T, Weston WL, Morelli JG. Atypical IgA/IgG pemphigus involving the skin, oral mucosa, and colon in a child: A novel variant of IgA pemphigus? Pediatr Dermatol 2005;22:321-7.
[Google Scholar]
|
| 5. |
Suzuki M, Karube S, Kobori Y, Usui K, Murata S, Kato H, et al. IgA pemphigus occurring in a 1-month-old infant. J Am Acad Dermatol 2003;48 2 Suppl: S22-4.
[Google Scholar]
|
| 6. |
Weston WL, Friednash M, Hashimoto T, Seline P, Huff JC, Morelli JG. A novel childhood pemphigus vegetans variant of intraepidermal neutrophilic IgA dermatosis. J Am Acad Dermatol 1998;38:635-8.
[Google Scholar]
|
| 7. |
Saurat JH, Merot Y, Salomon D, Didierjean L. Pemphigus-like IgA deposits and vesiculo-pustular dermatosis in a 10-year-old girl. Dermatology 1987;175:96-100.
[Google Scholar]
|
| 8. |
Gooptu C, Mendelsohn S, Amagai M, Hashimoto T, Nishikawa T, Wojnarowska F. Unique immunobullous disease in a child with a predominantly IgA response to three desmosomal proteins. Br J Dermatol 1999;141:882-6.
[Google Scholar]
|
| 9. |
Teraki Y, Amagai N, Hashimoto T, Kusunoki T, Nishikawa T. Intercellular IgA dermatosis of childhood. Selective deposition of monomer IgA1 in the intercellular space of the epidermis. Arch Dermatol 1991;127:221-4.
[Google Scholar]
|
| 10. |
de Oliveira JP, Gabbi TV, Hashimoto T, Aoki V, Santi CG, Maruta CW, et al. Two Brazilian cases of IgA pemphigus. J Dermatol 2003;30:886-91.
[Google Scholar]
|
Fulltext Views
5,036
PDF downloads
2,750





