Translate this page into:
Pemphigus vegetans of Hallopeau masquerading as acrodermatitis continua suppurativa
Corresponding author: Dr. Rashmi Jindal, Department of Dermatology, Venereology and Leprosy, Himalayan Institute of Medical Sciences, Swami Ram Nagar, Doiwala, Dehradun - 248 140, Uttarakhand, India. rashmijindal98@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jindal R, Chauhan P, Raturi S. Pemphigus vegetans of hallopeau masquerading as acrodermatitis continua suppurativa. Indian J Dermatol Venereol Leprol 2021;87:560-2.
Sir,
Pemphigus vegetans is a variant of pemphigus vulgaris accounting for less than 5% of its cases, characterized by papillomatous vegetations predominantly involving the intertriginous regions.1 The two known clinical forms of pemphigus vegetans Hallopeau and Neumann differ primarily in their initial presentation, with verrucous plaques starting de-novo in former and vesicles/bullae evolving into papillomatous vegetations in later. Atypical/ unusual manifestations of pemphigus vegetans with lesions limited to periorificial area, fingertip, tongue, nail folds and scalp have been reported previously and emphasize on the propensity to misdiagnose especially in the absence of oral involvement.2-4 The reported case further highlights the importance of entertaining pemphigus vegetans as a differential in recalcitrant verrucous plaques albeit localized in distribution.
A 60-year-old man having generalized vitiligo for 30 years presented to the dermatology outpatient department with erythematous-crusted plaques over the dorsum of great toes for six months [Figure 1]. Despite multiple courses of oral antibiotics (amoxicillin and linezolid) and topical anti-inflammatory creams (betamethasone valerate and clotrimazole) given elsewhere, with a presumptive diagnosis of paronychia, the lesions continued to progress and involved the remaining toes with subsequent destruction of great toenails. Cutaneous examination revealed erythematous crusted and partly verrucous plaques [highlighted on dermoscopy, Figure 2] with multiple pustules on the distal phalanges of both great toes associated with nail destruction. The rest of the toes had bright red erythema with multiple isolated to confluent studded pustules. Differential diagnoses of vegetating herpes, acrodermatitis continua suppurativa, paraneoplastic pemphigus, and pyoderma gangrenosum were contemplated. Bacterial swabs from pustules were sterile. Routine laboratory tests were inconspicuous. Tzanck smear displayed acantholytic cells; histopathology revealed suprabasal cleft with tombstoning of basal keratinocytes and abundant acantholytic cells [Figure 3].

- Erythematous crusted verrucous plaques with multiple pustules on the distal phalanges of both great toes associated with nail destruction. Other toes showing bright red erythema with multiple isolated to confluent studded pustules
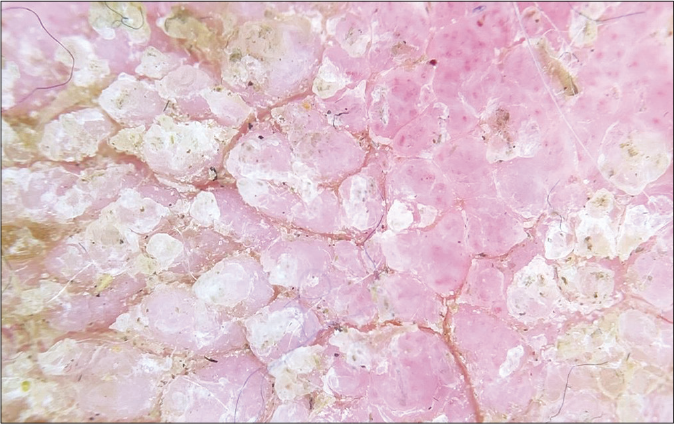
- Verrucous excrescences on dermoscopy with Dermlite DL 200 Hybrid, polarized mode (×100)
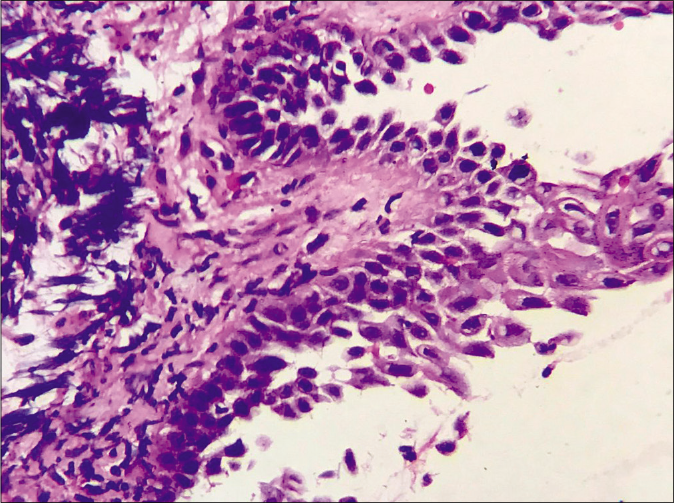
- Row of tombstone appearance of basal keratinocytes and multiple acantholytic cells in the blister cavity (H and E, ×400)
The diagnosis of pemphigus vegetans of Hallopeau was additionally confirmed by direct immunofluorescence of perilesional skin that exhibited intercellular deposits of IgG and C3 [Figure 4]. Due to financial restrictions indirect immunofluorescence for desmoglein-1 and 3 could not be performed. The patient was started on oral prednisolone and azathioprine in a dose of 1 mg/ kg body weight and 2mg/kg body weight respectively with marked improvement at four weeks [Figure 5]. The dose of prednisolone was slowly tapered to 0.25mg/kg body weight over a period of 16 weeks and azathioprine was continued in the same dose. Patient was last seen at 16 weeks and is maintaining remission with regular follow-up.

- Intercellular deposits of immunoglobulin G on direct immunofluorescence

- Significant improvement after 4 weeks of treatment with 40 mg/day of oral prednisolone
In the reported case, clinical picture mimicked acrodermatitis continua suppurativa, which was the provisional diagnosis once the bacterial swabs were reported as sterile. The otherwise good health of patients was against the diagnosis of paraneoplastic pemphigus as well as vegetating herpes. Absence of oral involvement dissuaded from considering pemphigus vegetans as a differential. Acantholytic cells in tzanck smear were disregarded as a secondary phenomenon seen in bacterial as well as viral infections. However, histopathology settled the diagnosis with a classical row of tombstones appearance and further confirmation was done with direct immunofluorescence. The undue delay in the diagnosis of the reported case could have been prevented with an early skin biopsy, which should be mandatory in non-responsive dermatoses. Being uncommon, diagnosis of pemphigus vegetans is at times overlooked especially in localized disease. Mergler et al. has reported exclusive involvement of right fingertip in the form of a circumferential-crusted plaque as a manifestation of pemphigus vegetans and further reviewed ten more cases without oral involvement. Erroneous diagnosis of pemphigus vegetans as eczema with paronychia has been previously reported. The diagnosis was delayed as lesions responded partially to topical corticosteroids. However, skin biopsy performed for relapses confirmed the diagnosis.4 Pemphigus vegetans being uncommon should not be forgotten and must be kept as a differential in patients presenting with recalcitrant verrucous or papillomatous plaques. The involvement of intertriginous regions and the oral cavity may not always be present and should not be considered essential. Though a variant of pemphigus vulgaris, pemphigus vegetans fails to reflect the same immunologically as reported in diverse studies. Anti desmoglein-1 (Dsg1) and anti-desmoglein-3 (Dsg3) antibodies may not always be identified instead certain cases show anti-desmocollin positivity.5 A recent review failed to correlate anti Dsg1 and anti Dsg3 with skin and/or mucosal involvement.1 Indirect immunofluorescence could not be performed in the reported case due to limited institutional infrastructure. Further research might delineate a subset of pemphigus vegetans associated with the absence of oral involvement owing to preferential autoantibody production against specific antigens.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Atypical clinical and serological manifestation of pemphigus vegetans: A case report and review of the literature. Case Rep Dermatol. 2017;9:121-30.
- [CrossRef] [PubMed] [Google Scholar]
- Pemphigus vegetans of the tongue: A diagnostic and therapeutic challenge. Int J Dermatol. 2013;52:350-1.
- [CrossRef] [PubMed] [Google Scholar]
- "Pemphigus vegetans of the scalp" J Eur Acad Dermatol Venereol. 2016;30:368-70.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic paronychia and onychomadesis in pemphigus vegetans: An unusual presentation in a rare autoimmune disease. Case Rep Med. 2018;2018:5980937.
- [CrossRef] [PubMed] [Google Scholar]
- Anti-desmocollin autoantibodies in nonclassical pemphigus. Br J Dermatol. 2015;173:59-68.
- [CrossRef] [PubMed] [Google Scholar]





