Translate this page into:
Vancomycin-induced linear IgA bullous dermatosis mimicking toxic epidermal necrolysis
Correspondence Address:
Chung Wen-Hung
Department of Dermatology, Chang Gung Memorial Hospital, 199, Tung Hwa North Road, Taipei 105
Taiwan
| How to cite this article: Jheng-Wei L, Yi-Chin S, Wen-Hung C. Vancomycin-induced linear IgA bullous dermatosis mimicking toxic epidermal necrolysis. Indian J Dermatol Venereol Leprol 2011;77:537 |
Sir,
Drug-induced linear immunoglobulin A (IgA) bullous dermatosis (LABD) is an unusual autoimmune bullous disorder characterized by linear IgA deposition along the basement membrane zone. It is most commonly associated with intravenous vancomycin therapy. [1] We report a case of vancomycin-associated LABD whose clinical pattern mimics toxic epidermal necrolysis (TEN).
A 41-year-old woman was admitted to our hospital because of recurring headache, fever, and progressive decline of consciousness over 2 weeks. A presumptive diagnosis of bacterial meningitis was made and she was initially treated with vancomycin and ceftriaxone. However, 10 days later, multiple tense bullae on erythematous bases developed on her trunk and limbs, except the palms and soles [Figure - 1]a and b. Positive Nikolsky′s sign was also found. The initial differential diagnoses included vancomycin-induced LABD and TEN. Subsequently, discontinuation of vancomycin and ceftriaxone was recommended. A skin biopsy taken from a single site demonstrated a subepidermal vesicle containing many neutrophils and few lymphocytes [Figure - 2]a and b. Direct immunofluorescence (DIF) of the perilesional skin revealed positive linear IgA at the epithelial basement membrane zone [Figure - 3]. A diagnosis of vancomycin-associated LABD was established. No new blisters had developed 3 days after the discontinuation of vancomycin, and the eruption was completely treated in 2 weeks.
 |
| Figure 1: (a) Buttocks showing tense bullae with background erythema. (b) Large flaccid confluent bullae with background erythema and widespread denudation on the right arm |
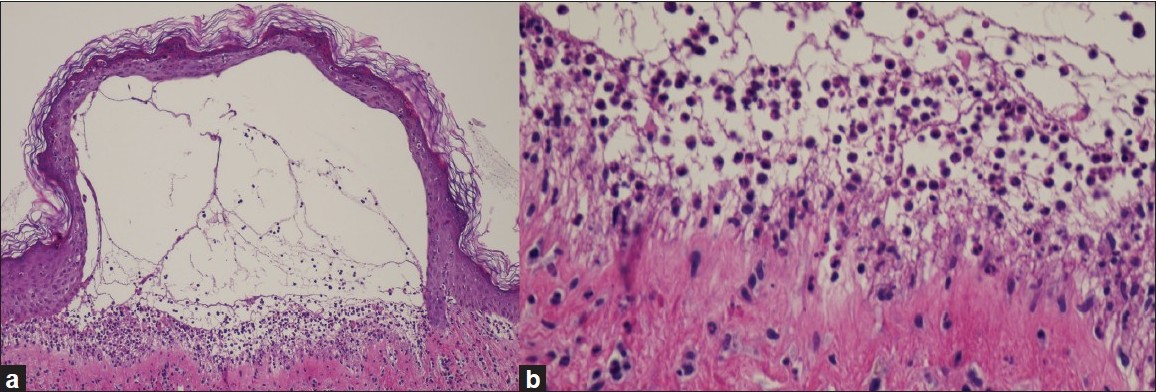 |
| Figure 2: (a) Subepidermal vesicle containing many inflammatory cells (H and E, ×40). (b) Subepidermal vesicle containing many neutrophils but few eosinophils (H and E, ×400) |
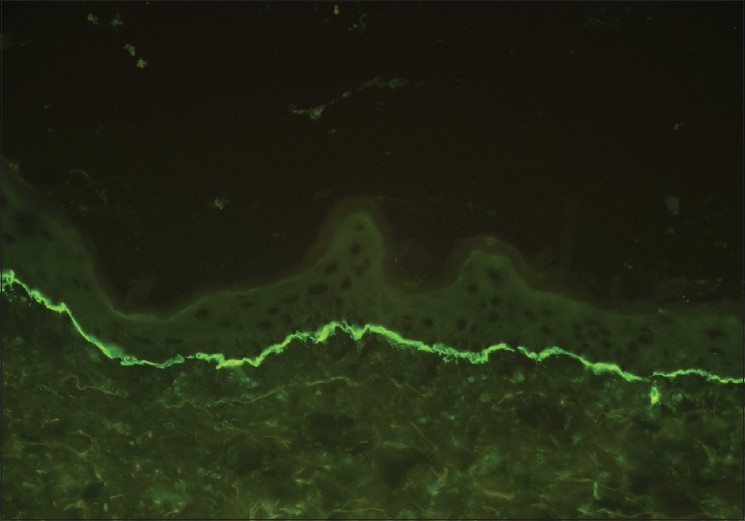 |
| Figure 3: DIF testing of perilesional skin revealed a positive linear IgA at the basement membrane zone |
LABD is associated with various disorders such as gastrointestinal diseases, autoimmune diseases, and malignancies. The significance of these associations is elusive, but they may play a role in the initial stimulation of the IgA mucosal immune system. [2]
Although our patient′s clinical presentation resembled TEN, a skin biopsy suggested a diagnosis of LABD. The histologic findings revealed a dermoepidermal separation with the occurrence of scattered dyskeratotic cells in epidermis and prominent spongiosis in the dermoepidermal junction at perilesional skin; these events presumably contribute to a positive Nikolsky′s sign. Recent exposure to vancomycin indicated the diagnosis of vancomycin-associated LABD. There is a low possibility that drug-induced LABD occurred concurrently with TEN because the blisters cleared upon withdrawal of the possible offending drugs and complete re-epithelialization occurred during the following 2 weeks.
LABD is associated with medications including penicillin, ceftriaxone and metronidazole, captopril, and interleukin-2. However, vancomycin has been most consistently implicated. [3] This patient was administered ceftriaxone and vancomycin during the course of her illness; hence, determining the offending agent was somewhat difficult. The most likely offending agent is vancomycin because of the timing of its administration, the clearing of symptoms after its withdrawal, and the frequency of vancomycin asociated LABD cases. However, we cannot rule out the possibility that ceftriaxone was the offending drug. According to the Naranjo ADR Probability Scale, the final score was 6; this indicated that either vancomycin or ceftriaxone could probably cause the eruption. [4]
The underlying pathogenesis of drug-induced LABD was believed to be an immune-mediated reaction rather than a direct toxicity process. The two drugs are unlikely to exert synergistic adverse reaction, making the presentation more severe.
The mainstay treatment for drug-induced LABD is withdrawal of the offending agent. [3] In the English literature, less than 10 cases of drug-induced LABD clinically mimicking TEN have been reported. [5] Vancomycin was implicated in 5 cases. The prognosis for LABD remains excellent if vancomycin is discontinued. Physicians should consider LABD as a differential diagnosis in patients with TEN or blistering diseases and must perform skin biopsies and immunofluorescence microscopy for early diagnosis.
| 1. |
Collier PM, Wojnarowska F. Drug-induced linear immunoglobulin a disease. Clin Dermatol 1993;24:529-33.
[Google Scholar]
|
| 2. |
Coelho S, Tellechea O, Reis JP, Mariano A, Figueiredo A. Vancomycin-associated linear IgA bullous dermatosis mimicking toxic epidermal necrolysis. Int J Dermatol 2006;137:995-6.
[Google Scholar]
|
| 3. |
Dellavalle RP, Burch JM, Tayal S, Golitz LE, Fitzpatrick JE. Vancomycin-associated linear IgA bullous dermatosis mimicking toxic epidermal necrolysis. J Am Acad Dermatol 2003;48:S56-7.
[Google Scholar]
|
| 4. |
Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981;30:239-45.
[Google Scholar]
|
| 5. |
Waldman MA, Black DR, Callen JP. Vancomycin-induced linear IgA bullous disease presenting as toxic epidermal necrolysis. Clin Exp Dermatol 2004;29:633-6.
[Google Scholar]
|
Fulltext Views
2,145
PDF downloads
2,548





